Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Surgical Metabolism and Nutrition > Volume 6(2); 2015 > Article
- ORIGINAL ARTICLE Intestinal Rehabilitation after Extensive Bowel Resection in Post-Gastrectomy Patients
- Seung Rim Han, M.D.1, Sanghoon Lee, M.D.1,2, Chae-Youn Oh, M.D.1,2, Hyun-Jung Kim, Ph.D.2, Hyo Jung Park, R.Ph., M.S.2, Jun Ho Lee, M.D., Ph.D.1, Tae Sung Sohn, M.D., Ph.D.1, Jae Moon Bae, M.D., Ph.D.1, Jeong-Meen Seo, M.D., Ph.D.1,2
-
Surgical Metabolism and Nutrition 2015;6(2):33-37.
DOI: https://doi.org/10.18858/smn.2015.6.2.33
Published online: December 30, 2015
Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
Department of Intestinal Rehabilitation Team, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
Department of Intestinal Rehabilitation Team, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- Correspondence to: Jeong-Meen Seo, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Ilwon-ro, Gangnam-gu, Seoul 06351, Korea Tel: +82-2-34103477, Fax: +82-2-34100040 E-mail: jm0815.seo@samsung.com
Copyright: © The Korean Society of Surgical Metabolism and Nutrition
This is an Open Access article distribute under the terms of the Creative Commons Attribution Non-commercial License (http://creativecommons.org/license/by-nc/3.0.) which permits unrestricted non-commercial use, distribution,and reproduction in any medium, provided the original work is properly cited.
- 871 Views
- 0 Download
Abstract
-
Purpose: Surgical complications requiring massive bowel resection after gastrectomy are rare. However, when such an event occurs the patient may develop short bowel syndrome and intestinal failure. We report our experience of intestinal rehabilitation in four post-gastrectomy patients.
-
Materials and Methods: From January 2011 to June 2014, four cases of short bowel syndrome were identified in post-gastrectomy patients. All patients were managed by a multidisciplinary team specialized in the care of intestinal failure patients. Patients’ medical records were reviewed retrospectively.
-
Results: The original diagnosis was early gastric cancer in all patients. One patient had synchronous esophageal cancer. Patients required extensive bowel resection due to bowel strangulation from internal herniation (3 cases), superior mesenteric artery torsion (1 case). Remnant small bowel length ranged from 10 cm to 80 cm and partial resection of the colon was performed in three cases. One patient received serial transverse enteroplasty (STEP) and one patient is receiving continuous enteral feeding via surgical gastrostomy. There were no cases of intestinal failure-associated liver disease. Two patients are receiving home parenteral nutrition in varying degrees. Two patients have been weaned off parenteral nutrition.
-
Conclusion: Four post-gastrectomy patients with short bowel syndrome were managed. Despite application of various medical and surgical measures, weaning off parenteral nutrition was difficult in these patients.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| SBS type | Jejuno-ileostomy | Jejuno-colostomy | Jejuno-colostomy | End Jejunostomy |
| Remnant SB Length | 60 cm from JJ | 60 cm from JJ | 80 cm from GJ | 10 cm from JJ |
| IRT referral after SBS | 18 months | 4 months | 1 month | 1 month |
| Interventions | STEP | CEF | CEF viagastrostomy | - |
| Outcome | Wean | Wean | EN with PN | Home TPN |
| Time to wean* | 16 months | 8 months | Ongoing† | -‡ |
| IFALD | No | No | No | No |
| CLABSI | 2 | No | No | No |
SBS = short bowel syndrome; SB = small bowel; JJ = jejuno-jejunostomy; GJ = gastro-jejunostomy; IRT = intestinal rehabilitation therapy; STEP = serial transverse enteroplasty; CEF = continuous enteral feeding; EN = enteral nutrition; PN = parenteral nutrition; TPN = total parenteral nutrition; IFALD = intestinal failure-associated liver disease; CLABSI = central line-associated blood stream infection.
*Interval time from intestinal rehabilitation therapy to completely enteral autonomy.
†During 6-month follow-up period from referred to intestinal rehabilitation team (IRT).
‡During 4-month follow-up period from referred to IRT.
DISCUSSION
- 1. Thompson JS. Comparison of massive vs. repeated resection leading to short bowel syndrome. J Gastrointest Surg 2000;4:101-4. ArticlePubMed
- 2. Carlsson E, Bosaeus I, Nordgren S. What concerns subjects with inflammatory bowel disease and an ileostomy? Scand J Gastroenterol 2003;38:978-84. ArticlePubMed
- 3. Thompson JS, DiBaise JK, Iyer KR, Yeats M, Sudan DL. Postoperative short bowel syndrome. J Am Coll Surg 2005;201:85-9. ArticlePubMed
- 4. Yi HW, Kim SM, Kim SH, Shim JH, Choi MG, Lee JH, et al. Complications leading reoperation after gastrectomy in patients with gastric cancer: frequency, type, and potential causes. J Gastric Cancer 2013;13:242-6. ArticlePubMedPMC
- 5. Messing B, Crenn P, Beau P, Boutron-Ruault MC, Rambaud JC, Matuchansky C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999;117:1043-50. ArticlePubMed
- 6. Bakker H, Bozzetti F, Staun M, Leon-Sanz M, Hebuterne X, Pertkiewicz M, et al. Home parenteral nutrition in adults: a european multicentre survey in 1997. ESPEN-Home Artificial Nutrition Working Group. Clin Nutr 1999;18:135-40. ArticlePubMed
- 7. Javid PJ, Malone FR, Reyes J, Healey PJ, Horslen SP. The experience of a regional pediatric intestinal failure program: successful outcomes from intestinal rehabilitation. Am J Surg 2010;199:676-9. ArticlePubMed
- 8. Modi BP, Langer M, Ching YA, Valim C, Waterford SD, Iglesias J, et al. Improved survival in a multidisciplinary short bowel syndrome program. J Pediatr Surg 2008;43:20-4. ArticlePubMedPMC
- 9. Hukkinen M, Merras-Salmio L, Sipponen T, Mutanen A, Rintala RJ, Mäkisalo H, et al. Surgical rehabilitation of short and dysmotile intestine in children and adults. Scand J Gastroenterol 2015;50:153-61. ArticlePubMed
- 10. Duro D, Kamin D, Duggan C. Overview of pediatric short bowel syndrome. J Pediatr Gastroenterol Nutr 2008;47(Suppl 1):S33-6. ArticlePubMed
- 11. Goulet O, Baglin-Gobet S, Talbotec C, Fourcade L, Colomb V, Sauvat F, et al. Outcome and long-term growth after extensive small bowel resection in the neonatal period: a survey of 87 children. Eur J Pediatr Surg 2005;15:95-101. ArticlePubMed
- 12. Soden JS. Clinical assessment of the child with intestinal failure. Semin Pediatr Surg 2010;19:10-9. ArticlePubMed
- 13. Sulkowski JP, Minneci PC. Management of short bowel syndrome. Pathophysiology 2014;21:111-8. ArticlePubMed
- 14. Amiot A, Messing B, Corcos O, Panis Y, Joly F. Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin Nutr 2013;32:368-74. ArticlePubMed
- 15. Kelly DA. Preventing parenteral nutrition liver disease. Early Hum Dev 2010;86:683-7. ArticlePubMed
- 16. Quirós-Tejeira RE, Ament ME, Reyen L, Herzog F, Merjanian M, Olivares-Serrano N, et al. Long-term parenteral nutritional support and intestinal adaptation in children with short bowel syndrome: a 25-year experience. J Pediatr 2004;145:157-63. ArticlePubMed
- 17. King B, Carlson G, Khalil BA, Morabito A. Intestinal bowel lengthening in children with short bowel syndrome: systematic review of the Bianchi and STEP procedures. World J Surg 2013;37:694-704. ArticlePubMedPDF
- 18. Sudan D, Thompson J, Botha J, Grant W, Antonson D, Raynor S, et al. Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg 2007;246:593-601; discussion 601-4. ArticlePubMed
- 19. Rege AS, Sudan DL. Autologous gastrointestinal reconstruction: review of the optimal nontransplant surgical options for adults and children with short bowel syndrome. Nutr Clin Pract 2013;28:65-74. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

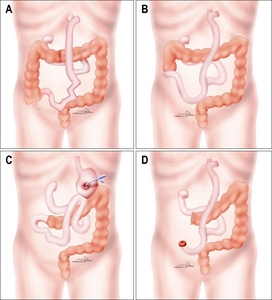
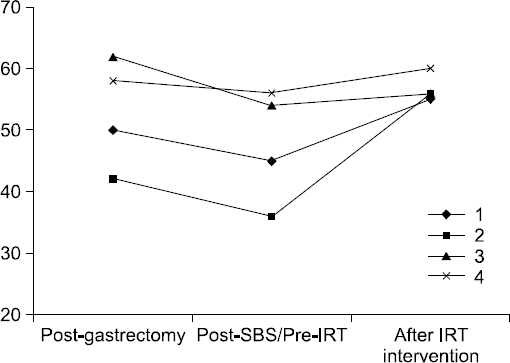
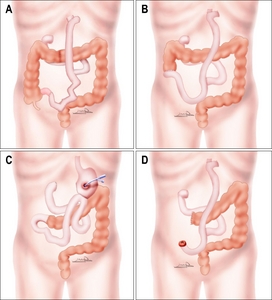
Fig. 1
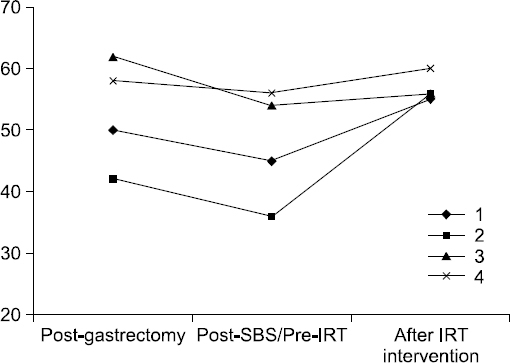
Fig. 2
Demographics of patients referred to intestinal rehabilitation
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| Sex/Age | M/55 | M/70 | M/56 | M/64 |
| Diagnosis | EGC withesophageal cancer | EGC | EGC | EGC |
| Operation | Total gastrectomy, esophagectomy with ECJ | Total gastrectomy | LADG (Billroth –II) | Total gastrectomy |
| Catastrophic event | Internal herniation | Internal herniation | Internal herniation | SMA torsion |
| Event time (from initial OP) | 3 months | 22 months | 15 months | 48 months |
| SBS type | Jejuno-ileostomy | Jejuno-colostomy | Jejuno-colostomy | End Jejunostomy |
| Remnant SB Length | 60 cm from JJ | 60 cm from JJ | 80 cm from GJ | 10 cm from JJ |
| IC valve | Intact | No | No | No |
| Remnant colon | 50% of colon | 80% of colon | 50% of colon | 50% of colon |
EGC = early gastric cancer; ECJ = esophago-colo-jejunostomy; LADG = laparoscopic assisted distal gastrectomy; SMA = superior mesenteric artery; SBS = short bowel syndrome; SB = small bowel; JJ = jejuno-jejunostomy; GJ = gastro-jejunostomy; IC = ileo-cecal; OP = operation.
Outcome of patients after intestinal rehabilitation
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| SBS type | Jejuno-ileostomy | Jejuno-colostomy | Jejuno-colostomy | End Jejunostomy |
| Remnant SB Length | 60 cm from JJ | 60 cm from JJ | 80 cm from GJ | 10 cm from JJ |
| IRT referral after SBS | 18 months | 4 months | 1 month | 1 month |
| Interventions | STEP | CEF | CEF viagastrostomy | - |
| Outcome | Wean | Wean | EN with PN | Home TPN |
| Time to wean |
16 months | 8 months | Ongoing |
- |
| IFALD | No | No | No | No |
| CLABSI | 2 | No | No | No |
SBS = short bowel syndrome; SB = small bowel; JJ = jejuno-jejunostomy; GJ = gastro-jejunostomy; IRT = intestinal rehabilitation therapy; STEP = serial transverse enteroplasty; CEF = continuous enteral feeding; EN = enteral nutrition; PN = parenteral nutrition; TPN = total parenteral nutrition; IFALD = intestinal failure-associated liver disease; CLABSI = central line-associated blood stream infection.
*Interval time from intestinal rehabilitation therapy to completely enteral autonomy.
†During 6-month follow-up period from referred to intestinal rehabilitation team (IRT).
‡During 4-month follow-up period from referred to IRT.
EGC = early gastric cancer; ECJ = esophago-colo-jejunostomy; LADG = laparoscopic assisted distal gastrectomy; SMA = superior mesenteric artery; SBS = short bowel syndrome; SB = small bowel; JJ = jejuno-jejunostomy; GJ = gastro-jejunostomy; IC = ileo-cecal; OP = operation.
SBS = short bowel syndrome; SB = small bowel; JJ = jejuno-jejunostomy; GJ = gastro-jejunostomy; IRT = intestinal rehabilitation therapy; STEP = serial transverse enteroplasty; CEF = continuous enteral feeding; EN = enteral nutrition; PN = parenteral nutrition; TPN = total parenteral nutrition; IFALD = intestinal failure-associated liver disease; CLABSI = central line-associated blood stream infection. Interval time from intestinal rehabilitation therapy to completely enteral autonomy. During 6-month follow-up period from referred to intestinal rehabilitation team (IRT). During 4-month follow-up period from referred to IRT.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN Cite
Cite

