Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Funded articles
- Page Path
- HOME > Browse articles > Funded articles
Original Article
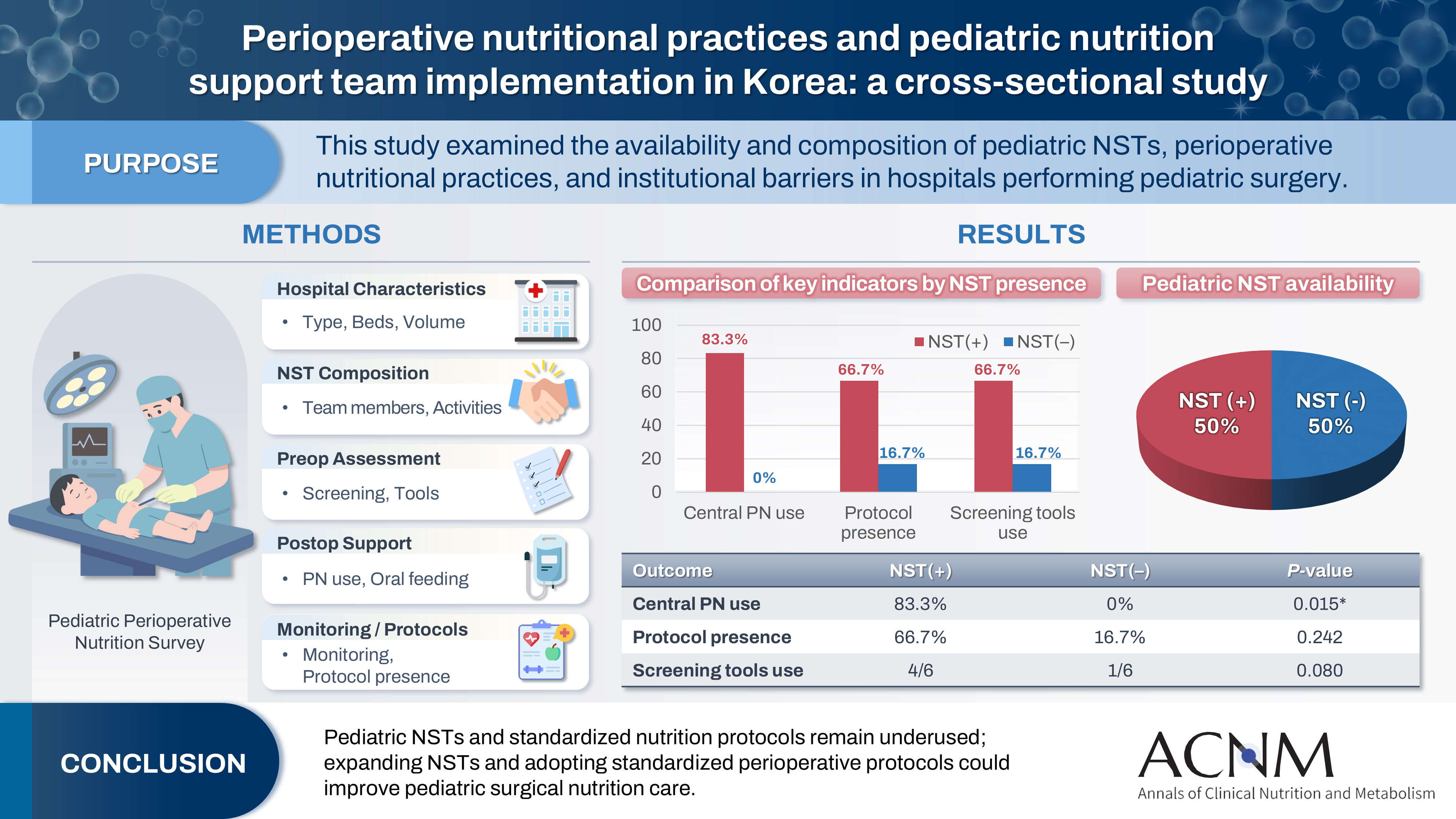
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
- Funded: Korean Society of Surgical Metabolism and Nutrition
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 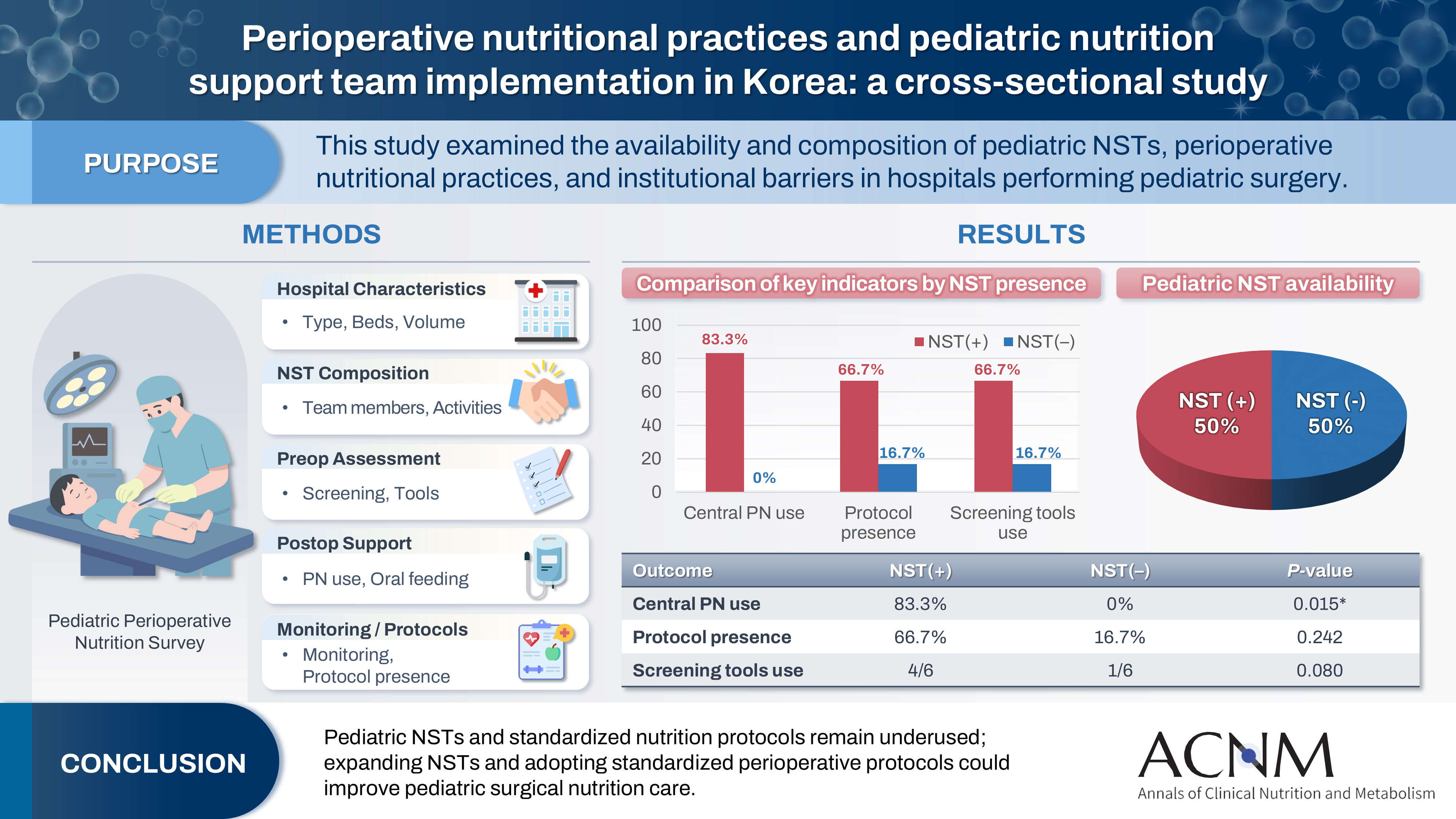
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 1,443 View
- 22 Download

Guideline
- The 2024 Korean Enhanced Recovery After Surgery guidelines for hepatobiliary and pancreatic surgery
- Kwangpyo Hong, Hongbeom Kim, Hyung Sun Kim, Hae Won Lee, Ho Joong Choi, YoungRok Choi, Jae Do Yang, Sung-Moon Jeong, Dae Wook Hwang, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2025;17(3):172-180. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0034
- Funded: National Cancer Center
-
 Abstract
Abstract
 PDF
PDF - Purpose
The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition has developed comprehensive guidelines for hepatobiliary and pancreatic (HBP) surgery by adapting established international protocols. These guidelines provide evidence-based recommendations specifically tailored to the Korean healthcare system and address perioperative management for both pancreatoduodenectomy and hepatectomy.
Methods
The HBP subcommittee reviewed existing international ERAS guidelines and conducted an adaptation process. Key questions were identified based on national survey results from Korean HBP surgeons and were prioritized according to clinical relevance. The committee focused on elements supported by moderate- to high-quality evidence with strong recommendation grades. Literature searches were conducted through January 2025, and evidence quality was evaluated using GRADE methodology. Four key questions underwent formal assessment, and eight additional questions were adapted from international guidelines.
Results
Twelve key questions were selected and addressed, covering critical perioperative care domains: prehabilitation, preoperative nutritional assessment and support, anti-thrombotic prophylaxis, prophylactic abdominal drainage, preoperative biliary drainage, smoking and alcohol cessation, pre-anesthetic medication, minimally invasive surgical approaches, prophylactic nasogastric intubation, postoperative glycemic control, perianastomotic drainage management, and early mobilization protocols. Each recommendation was assigned specific evidence levels and graded for strength. High-quality evidence supported strong recommendations for the routine avoidance of prophylactic drainage in uncomplicated hepatectomy, early drain removal after pancreatoduodenectomy in low-risk patients, elimination of routine nasogastric decompression, and the implementation of early mobilization strategies.
Conclusion
These Korean-adapted ERAS guidelines for HBP surgery are expected to standardize perioperative care, reduce postoperative complications, shorten hospital stays, and enhance overall patient outcomes across Korean healthcare institutions.
- 1,625 View
- 39 Download

Original Articles
- Insulinotropic action of L-carnitine and branched-chain amino acids following energy intake in healthy, young Japanese women: a non-randomized controlled trial
- Yoichi Sakurai, Hideyuki Namba, Satoshi Odo
- Ann Clin Nutr Metab 2025;17(2):139-148. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0011
- Funded: Ministry of Education, Culture, Sports, Science and Technology, Grant-inAid for Scientific Research
-
 Abstract
Abstract
 PDF
PDF - Purpose
The present study uses healthy human volunteers to examine the insulinotropic action of L-carnitine and branched-chain amino acids (BCAAs) after energy intake.
Methods
A total of 39 young, healthy human volunteers were assigned to receive oral doses of either L-carnitine alone (L group, n=10) or L-carnitine combined with a single or long-term continuous dose of BCAAs. Controls (C group, n=16) received none of these. L-carnitine was administered orally at 1,000 mg/d for 14 days, and BCAA was administered orally either once just before exercise (L+SB group, n=6), or every day for 14 days (L+CB group, n=7) until 2 days before the experiment. After overnight fasting, 200 kcal of glucose and oral nutritional supplement were administered to prevent hypoglycemia. Blood glucose, free-fatty acid, and serum insulin levels were measured to examine the insulinotropic action before and after exercise.
Results
Blood glucose and serum insulin levels in the L group were significantly lower than those in the C group. While the serum insulin levels were higher after energy administration than those in the fasting state in all groups, these were significantly higher in the L+SB group and in the L+CB group compared with those in the L group. The insulinotropic action after energy intake remained even after the repeated administration of BCAA discontinued 2 days before the experi¬ment and even after serum BCAA levels remained the same.
Conclusion
While the insulinotropic action appeared after a single dose of BCAA, it was also potentiated by long-term repeated oral administration of BCAA.
- 1,213 View
- 13 Download

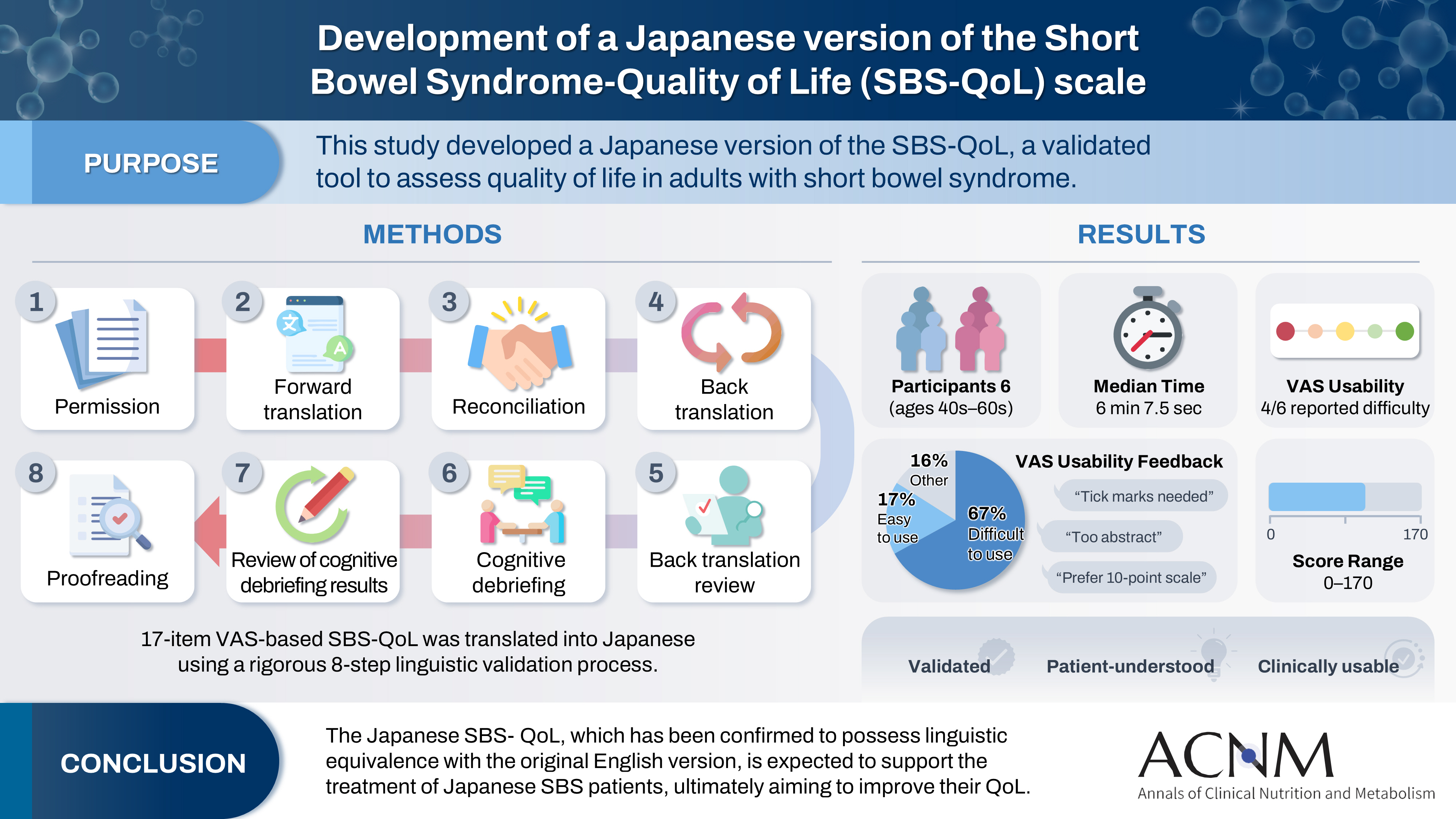
- Development of a Japanese version of the Short Bowel Syndrome-Quality of Life (SBS-QoL) scale
- Yuko Tazuke, Mayu Suzuki, Sae Kikuchi, Kaori Ishiguro, Hiroomi Okuyama
- Ann Clin Nutr Metab 2025;17(2):132-138. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0016
- Funded: Takeda Pharmaceutical Company Limited
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 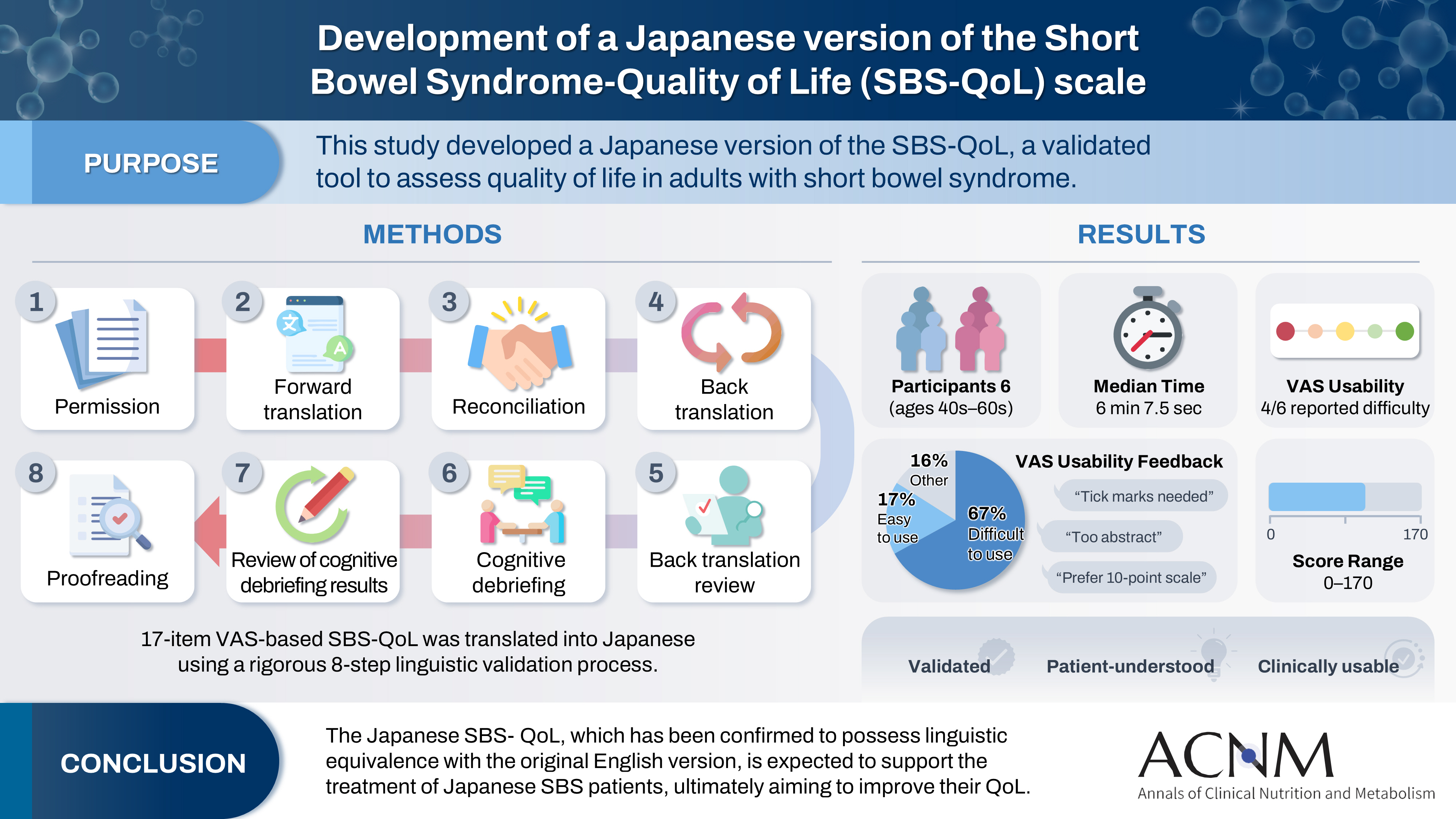
- Purpose
The Short Bowel Syndrome‐Quality of Life (SBS‐QoL) scale is a reliable and sensitive instrument developed to measure and evaluate the quality of life (QoL) in adult patients with short bowel syndrome (SBS). In Japan, increasing attention has been given to the assessment of QoL in patients with SBS; however, no Japanese‐language SBS‐specific scale is currently available. This study aimed to develop a Japanese version of the SBS‐QoL based on the original English version.
Methods
A provisional Japanese version was created in accordance with the guidelines of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force, utilizing a process of forward translation, adjustment, and back translation.
Results
Cognitive debriefing using the provisional Japanese version was conducted with six Japanese patients with SBS. Based on these results, the Japanese wording was evaluated and revised, leading to the creation of the final Japanese version.
Conclusion
The Japanese SBS‐QoL, which has been confirmed to possess linguistic equivalence with the original English version, is expected to support the treatment of Japanese SBS patients, ultimately aiming to improve their QoL.
- 1,776 View
- 19 Download

- Evaluation of the modified Nutrition Risk in Critically Ill score in Korean critically ill patients with COVID-19: a retrospective cohort study
- Won Ho Han, Jong-Mog Lee, Jae Hoon Lee, Hyun Mi Lee, Ji-Yeon Kim, Mok Young Jang, Sung-Sik Han
- Ann Clin Nutr Metab 2025;17(2):125-131. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0009
- Funded: National Cancer Center
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
We evaluated the efficacy of the modified Nutrition Risk in Critically Ill (mNUTRIC) score for malnutrition screening and its association with mortality in intensive care unit (ICU) patients with COVID-19.
Methods
The nutritional status of 129 COVID-19 ICU patients admitted between February 2021 and May 2022 was assessed using American Society for Parenteral and Enteral Nutrition/Academy of Nutrition and Dietetics (ASPEN/AND) criteria. The sensitivity, specificity, and clinical correlations of the mNUTRIC score were analyzed.
Results
Of the 129 patients, 35 (27.1%) met the ASPEN/AND malnutrition criteria. Multivariable analysis identified the mNUTRIC score, underlying malignancy, and mechanical ventilation as significant factors associated with malnutrition. The mNUTRIC score had a sensitivity of 77.1% and specificity of 63.8% (area under the curve [AUC], 0.71; 95% confidence interval [CI], 0.62–0.79) for diagnosing malnutrition, improving to 88.6% and 80.9%, respectively, after adjusting for malignancy and ventilation (AUC, 0.89; 95% CI, 0.82–0.95). Patients with a low mNUTRIC score had a mortality rate of 2.9% and a median ICU stay of 7.7 days (range, 0–84.2 days), whereas those with a high score (≥5) had a mortality rate of 13.1% and a median ICU stay of 10.2 days (range, 1.4–88.5 days) (P=0.046 and P=0.011, respectively).
Conclusion
The mNUTRIC score is an effective screening tool for malnutrition in ICU patients with COVID-19, especially those with malignancy or requiring mechanical ventilation, and is strongly associated with mortality and length of ICU stay.
- 3,095 View
- 31 Download

- Development of a pre- and re-habilitation protocol for gastrointestinal cancer surgery
- Eun Young Kim, Jung Hoon Bae, Jiseon Kim, Eun Joo Yang, Sang-Jae Park, In Kyu Lee, on behalf of the Task Force Team for Development and Trial Application of Pre/Rehabilitation Protocol in GI Cancer Surgery
- Ann Clin Nutr Metab 2025;17(1):25-40. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0001
- Funded: Korean Society of Surgical Metabolism and Nutrition
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
Surgical resection is the primary curative treatment for gastrointestinal (GI) cancer; however, it is associated with high postoperative complication rates and impaired recovery. Frailty, malnutrition, and sarcopenia increase morbidity and mortality, underscoring the need for perioperative rehabilitation programs. Standardized rehabilitation protocols during the perioperative period are currently lacking in Korea. We aimed to develop an evidence-based rehabilitation protocol for GI cancer patients to enhance postoperative outcomes and facilitate clinical implementation.
Methods
A multidisciplinary task force team comprising experts in surgery, clinical nutrition, and rehabilitation medicine conducted a systematic literature search and comprehensive review from 2012 to 2022 to develop a standardized pre- and re-habilitation protocol for GI cancer surgery. The protocol underwent external validation and subsequent refinements before being finalized through expert consensus.
Results
The protocol development process was organized into four consecutive phases: keyword selection, literature review and case report form development, initial protocol drafting, and external validation leading to the final version of the protocol. The final version of the rehabilitation protocol is presented in the main text and included as Supplements.
Conclusion
This protocol provides a standardized clinical guideline based on the latest evidence-based pre- and re-habilitation strategies and is designed for seamless integration into routine clinical practice. By facilitating proactive rehabilitation interventions, it aims to improve outcomes in GI cancer patients who are at high risk of postoperative complications, functional decline, and malnutrition.
- 3,565 View
- 111 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN First
First Prev
Prev


