Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Current issue
- Page Path
- HOME > Browse articles > Current issue
Editorial
- Annals of Clinical Nutrition and Metabolism (ACNM): a new milestone toward global recognition
- Suk-Kyung Hong
- Ann Clin Nutr Metab 2025;17(3):163-164. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0038
- 532 View
- 22 Download

Guidelines
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
- Ja Kyung Min, Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Jung Mi Song, Hyunjung Kim, Jae Hak Kim, Kyung Won Seo, Sung Shin Kim, Chi-Min Park, Jeongyun Park, Eunjung Kim, Eunmi Sul, Sung-Sik Han, Jeong Wook Kim, Seungwan Ryu, Minji Seok, Jinhee Yoon, Eunhee Kong, Youn Soo Cho, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(3):165-171. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0037
-
 Abstract
Abstract
 PDF
PDF - Purpose
We developed evidence-based recommendations for selecting and initiating the enteral nutrition (EN) delivery route in adult and pediatric patients to improve safety and standardize practice in Korea.
Methods
Key questions covered feeding tube selection, methods to verify tube placement, confirmation in pediatric patients, and timing of EN following percutaneous endoscopic gastrostomy (PEG). Recommendations were drafted and refined through multidisciplinary expert consensus under the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Results
Feeding tube selection should be based on gastrointestinal anatomy, function, and expected EN duration. Short-term feeding is recommended with nasogastric or orogastric tubes, whereas long-term feeding should use percutaneous or surgical routes such as PEG. Tube position must always be verified before use, preferably with radiography or pH testing; auscultation alone is unreliable and should not be used. In pediatric patients, radiographic confirmation remains the gold standard, although pH testing and insertion-length assessment may be considered when imaging is not feasible. After PEG, EN can be initiated safely within 4 hours in both adults and children without increasing complications if trained staff monitor for leakage or infection.
Conclusion
This guideline offers a structured framework for safe and timely EN tailored to patient characteristics. Early verification and multidisciplinary collaboration help reduce complication, improving outcomes of EN therapy.
- 686 View
- 39 Download

- The 2024 Korean Enhanced Recovery After Surgery guidelines for hepatobiliary and pancreatic surgery
- Kwangpyo Hong, Hongbeom Kim, Hyung Sun Kim, Hae Won Lee, Ho Joong Choi, YoungRok Choi, Jae Do Yang, Sung-Moon Jeong, Dae Wook Hwang, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2025;17(3):172-180. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0034
-
 Abstract
Abstract
 PDF
PDF - Purpose
The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition has developed comprehensive guidelines for hepatobiliary and pancreatic (HBP) surgery by adapting established international protocols. These guidelines provide evidence-based recommendations specifically tailored to the Korean healthcare system and address perioperative management for both pancreatoduodenectomy and hepatectomy.
Methods
The HBP subcommittee reviewed existing international ERAS guidelines and conducted an adaptation process. Key questions were identified based on national survey results from Korean HBP surgeons and were prioritized according to clinical relevance. The committee focused on elements supported by moderate- to high-quality evidence with strong recommendation grades. Literature searches were conducted through January 2025, and evidence quality was evaluated using GRADE methodology. Four key questions underwent formal assessment, and eight additional questions were adapted from international guidelines.
Results
Twelve key questions were selected and addressed, covering critical perioperative care domains: prehabilitation, preoperative nutritional assessment and support, anti-thrombotic prophylaxis, prophylactic abdominal drainage, preoperative biliary drainage, smoking and alcohol cessation, pre-anesthetic medication, minimally invasive surgical approaches, prophylactic nasogastric intubation, postoperative glycemic control, perianastomotic drainage management, and early mobilization protocols. Each recommendation was assigned specific evidence levels and graded for strength. High-quality evidence supported strong recommendations for the routine avoidance of prophylactic drainage in uncomplicated hepatectomy, early drain removal after pancreatoduodenectomy in low-risk patients, elimination of routine nasogastric decompression, and the implementation of early mobilization strategies.
Conclusion
These Korean-adapted ERAS guidelines for HBP surgery are expected to standardize perioperative care, reduce postoperative complications, shorten hospital stays, and enhance overall patient outcomes across Korean healthcare institutions.
- 1,625 View
- 39 Download

Original Articles
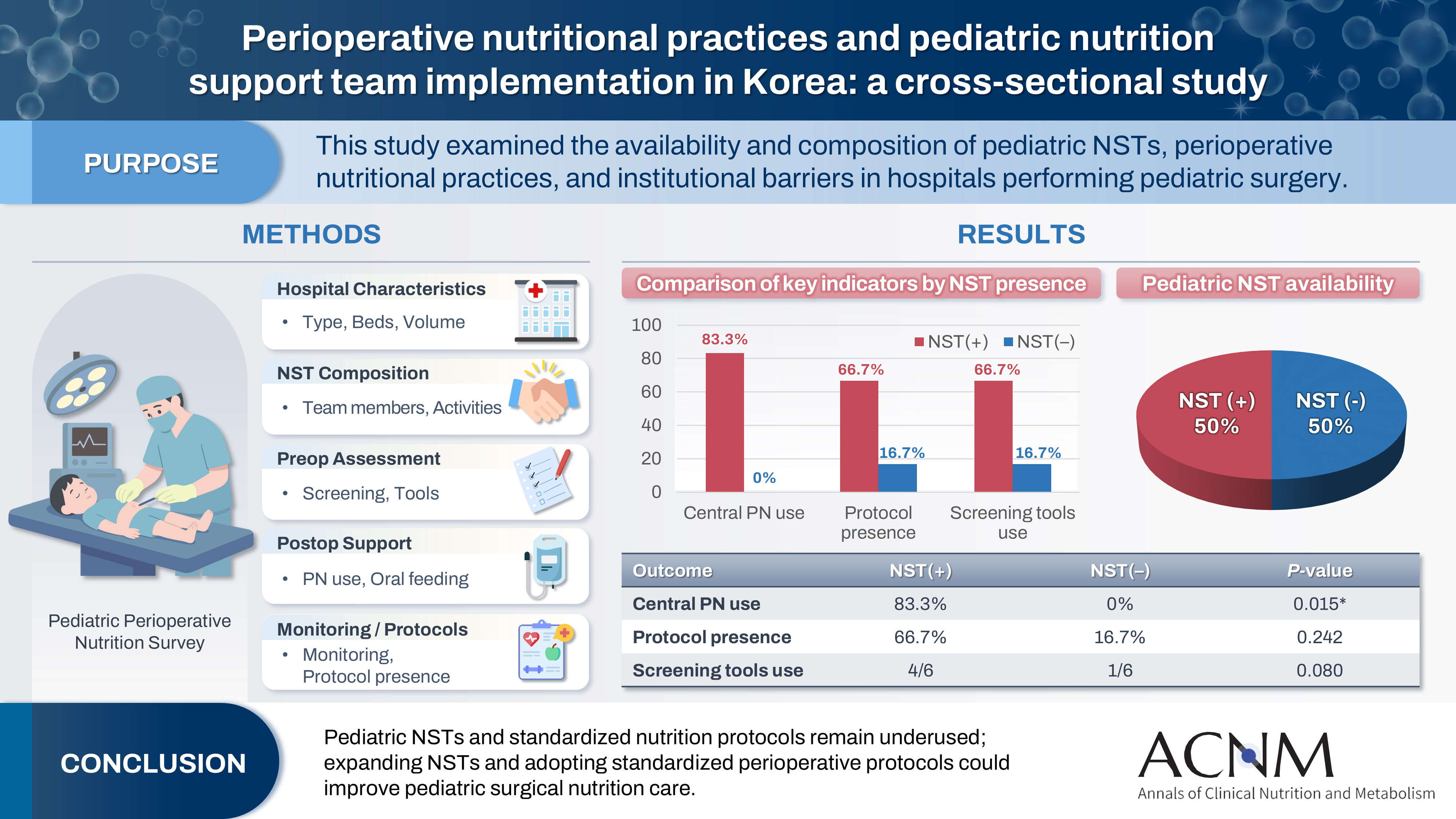
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 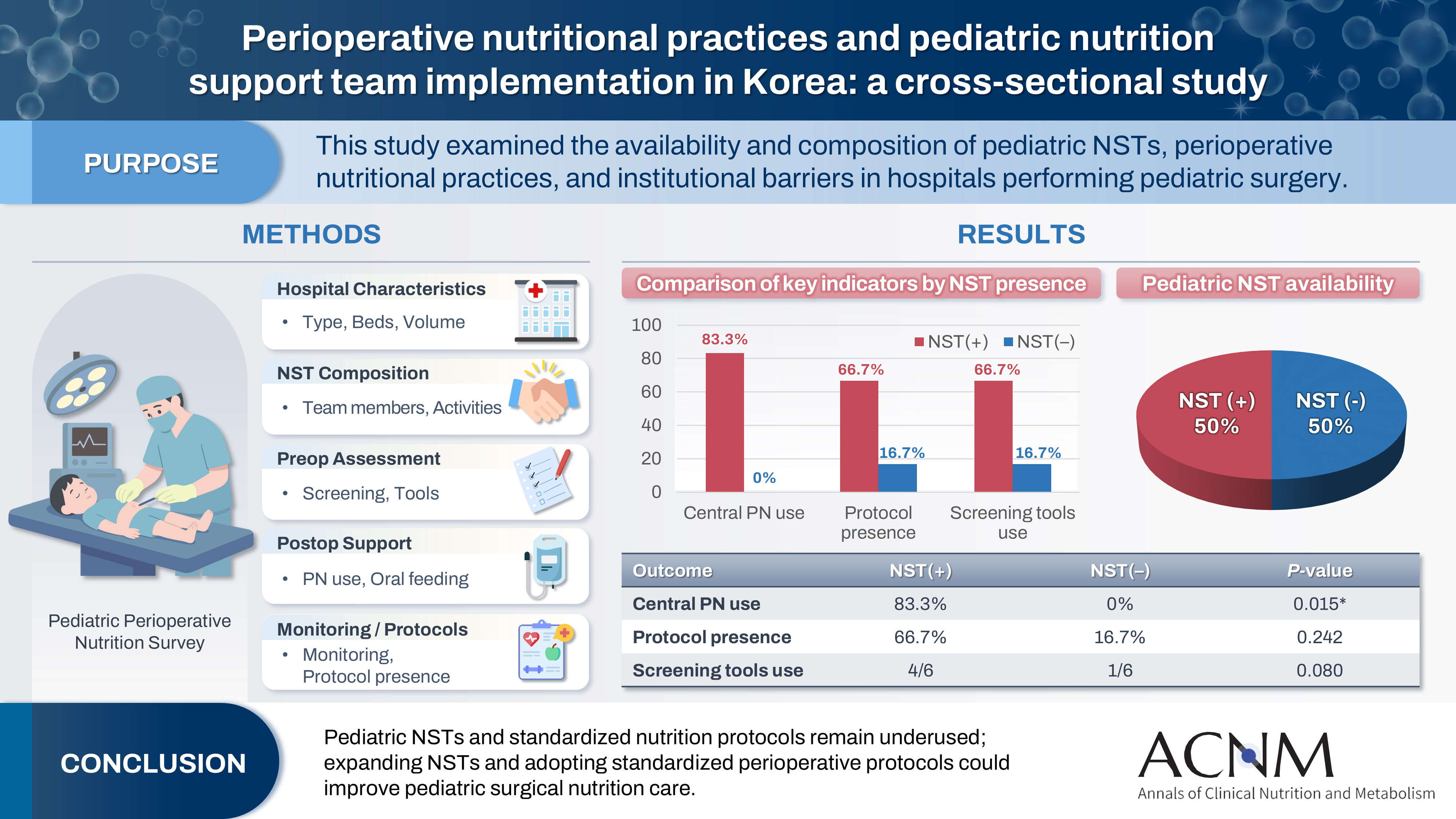
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 1,443 View
- 22 Download

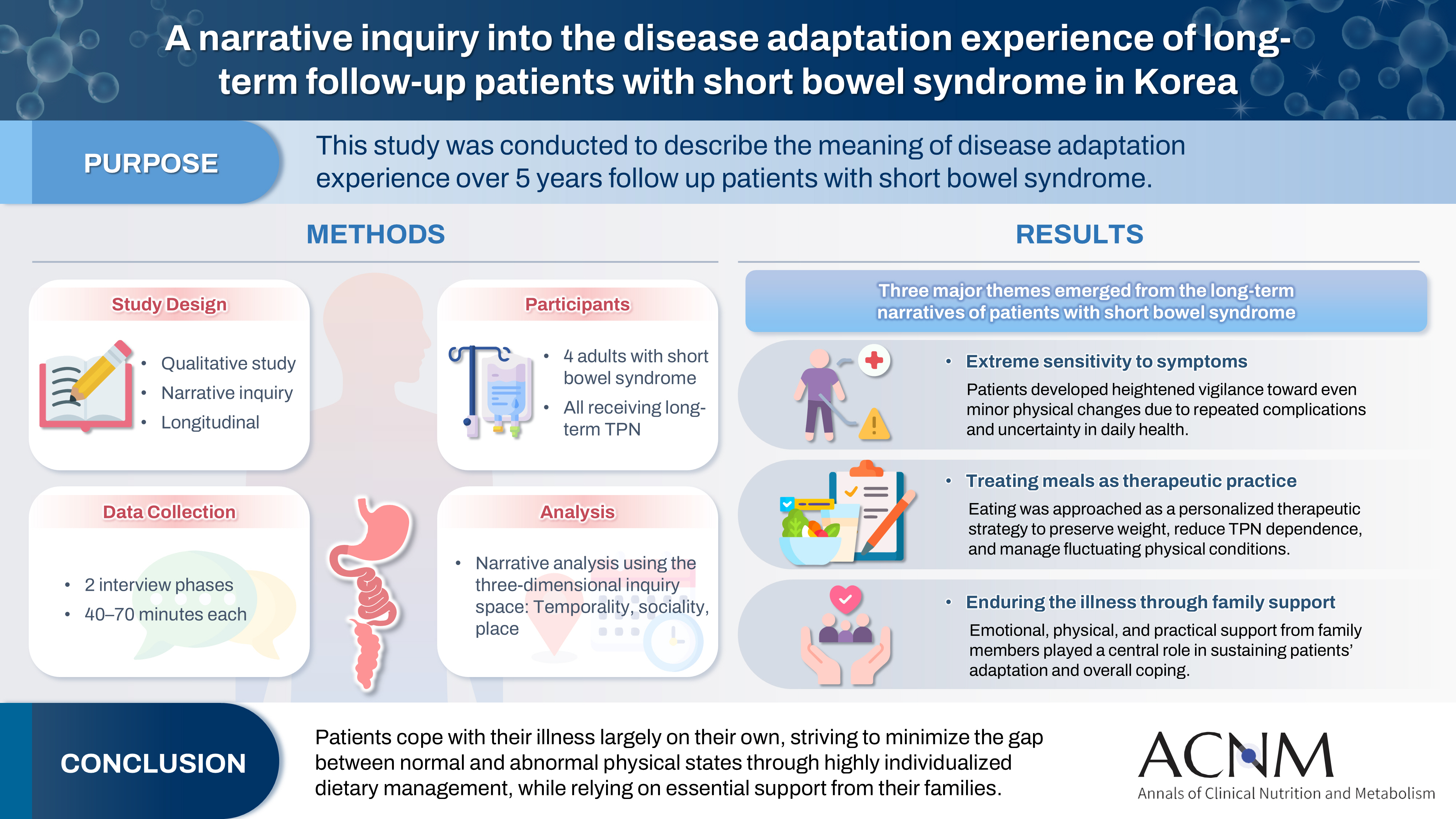
- A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
- Eun-Mi Seol, Eunjung Kim
- Ann Clin Nutr Metab 2025;17(3):188-195. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0028
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 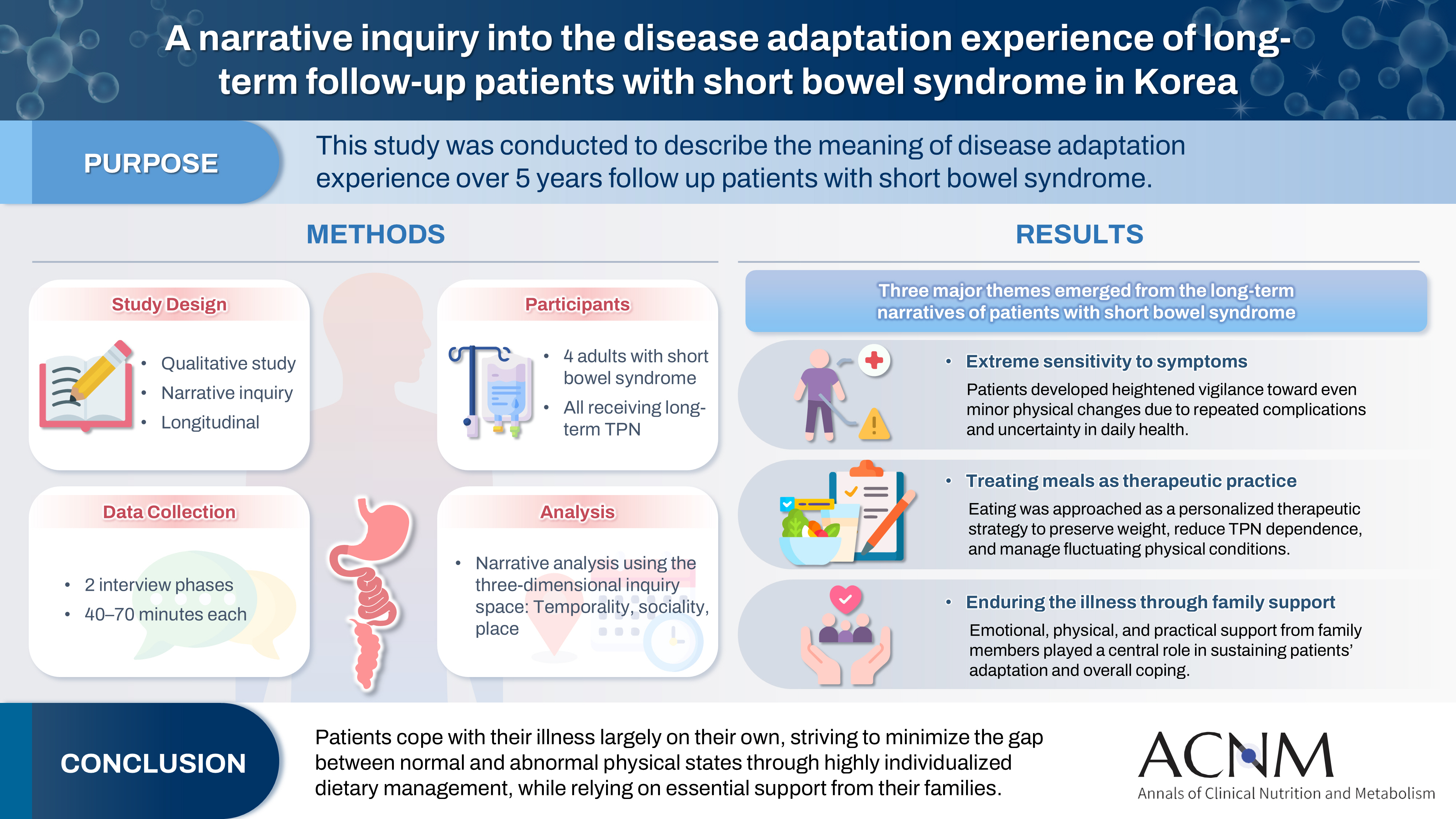
- Purpose
This study was conducted to describe the meaning of disease adaptation experience over a 5-year long-term follow-up of patients with short bowel syndrome.
Methods
Four patients were recruited from a tertiary hospital in Korea. This study was conducted through first and second interviews from January 2019 to July 2022. The transcribed data were analyzed using narrative methods.
Results
The mean age of the participants was 64 years, and the mean treatment period after small bowel resection was 100 months. The participants lost a mean of 19.3 kg body weight and all were receiving home total parenteral nutrition 2–7 days a week. The meaning of the experience of adapting to the disease for patients was found to be “extremely sensitive to the symptoms,” “considering eating food as another effective treatment method,” and “enduring the disease through family affection.”
Conclusion
Patients are struggling alone to cope with physical symptoms and adapt to their disease. For this, they are doing their best to narrow the gap between normal and abnormal physical conditions by thoroughly implementing diet therapy according to their physical characteristics. This entire process is supported by their families.
- 1,206 View
- 22 Download

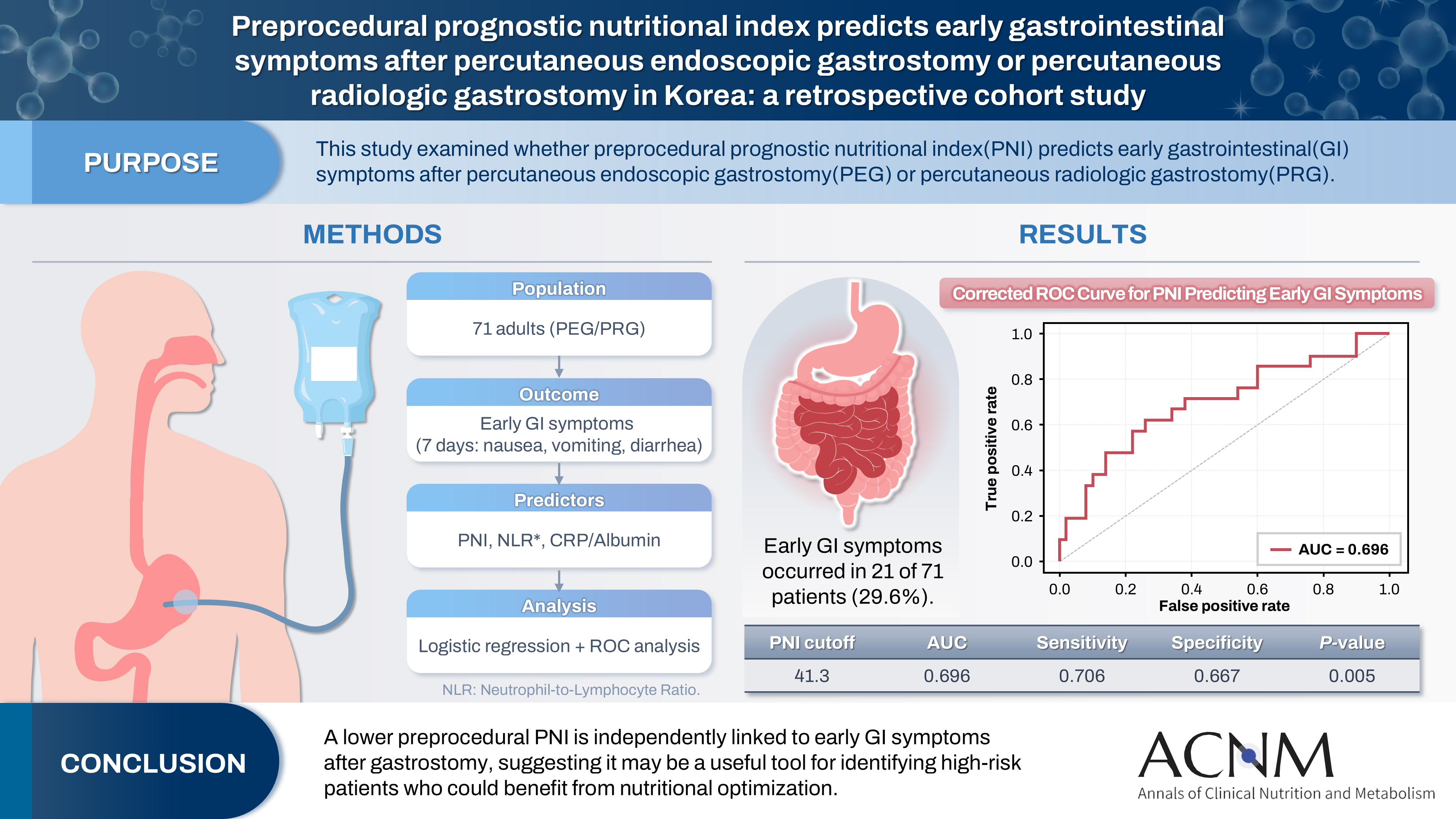
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
- Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0032
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 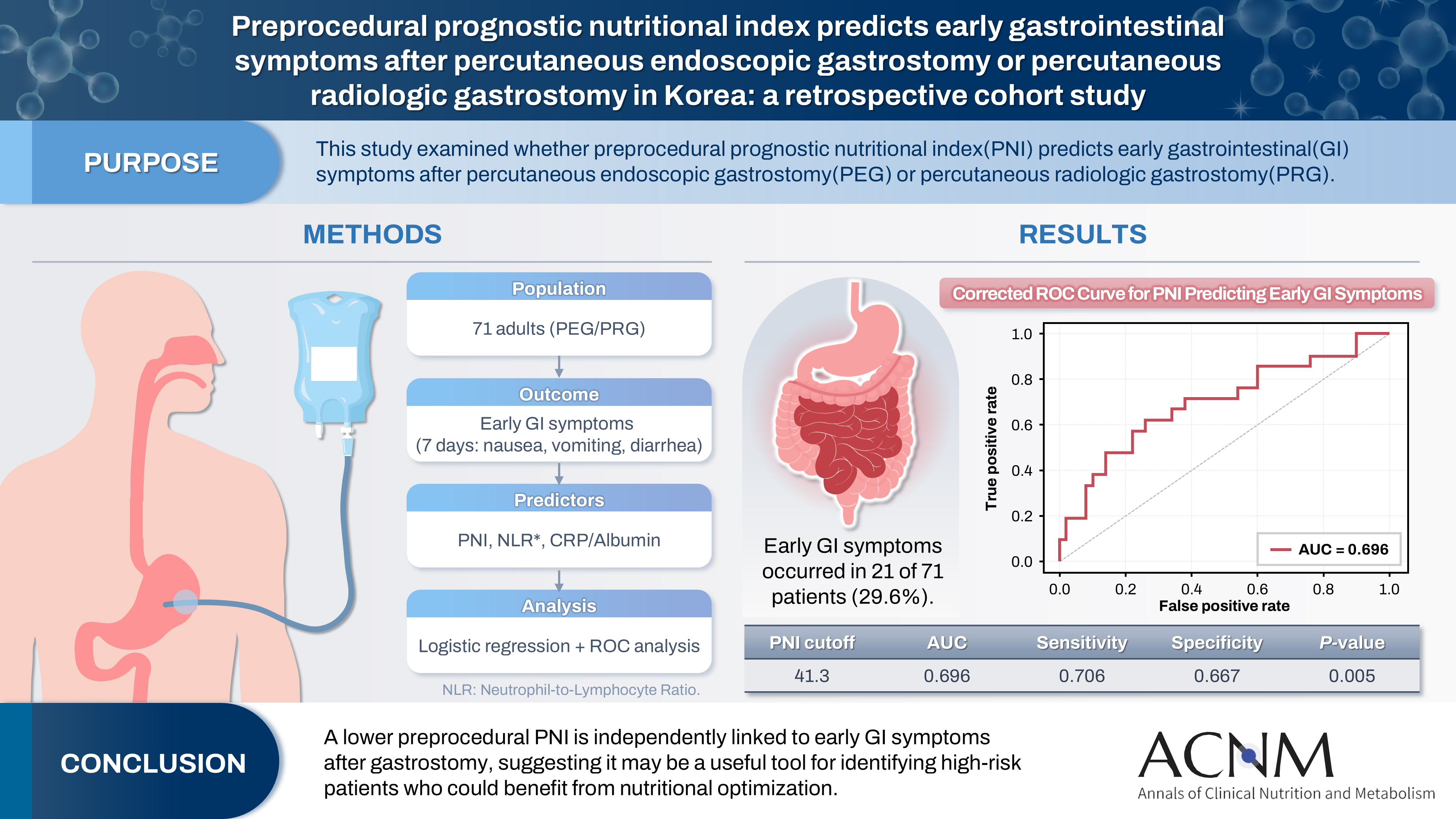
- Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
- 866 View
- 19 Download

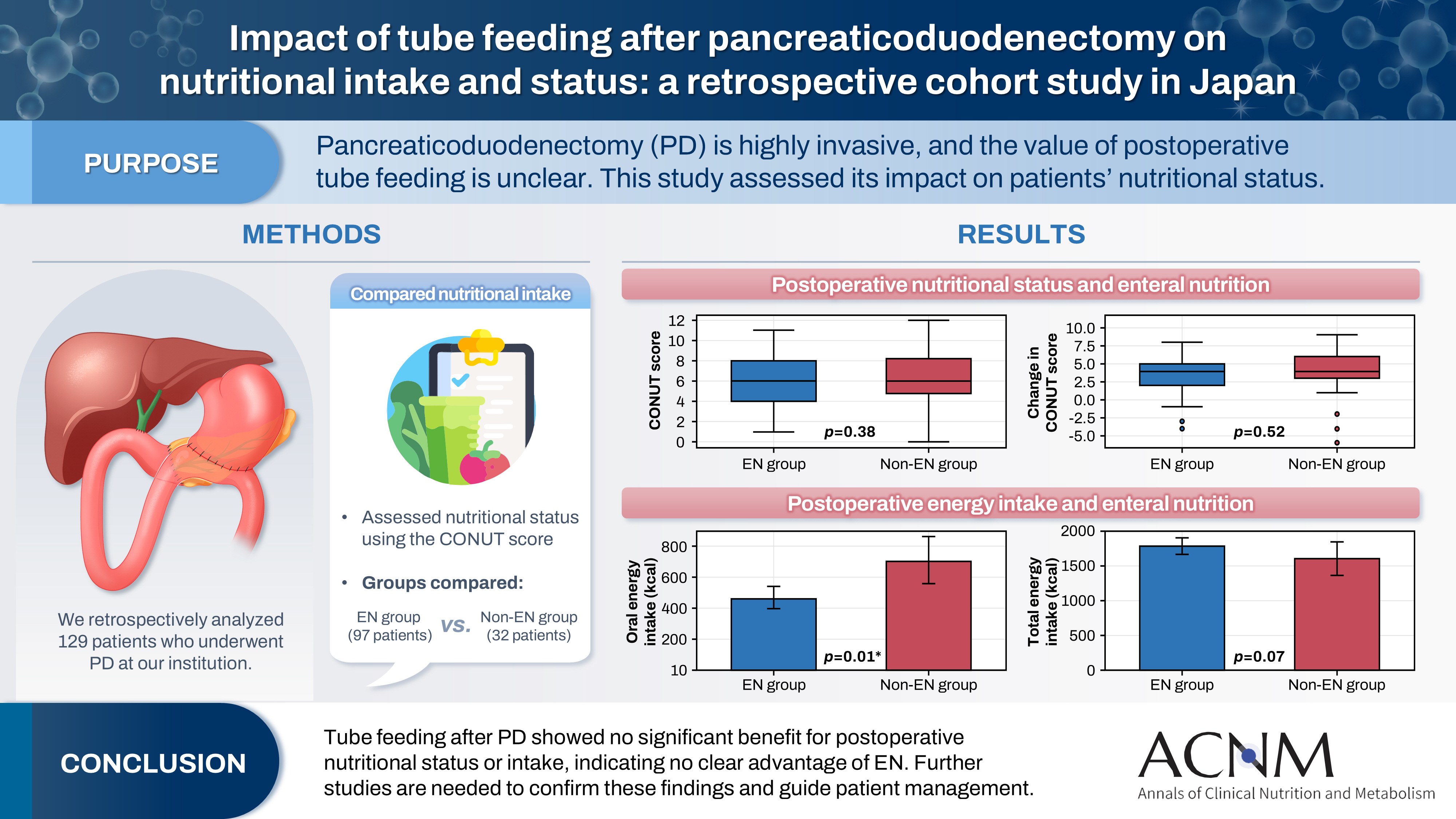
- Impact of tube feeding after pancreaticoduodenectomy on nutritional intake and status: a retrospective cohort study in Japan
- Masaharu Ishida, Masahiro Iseki, Shuichiro Hayashi, Aya Noguchi, Hideaki Sato, Shingo Yoshimachi, Akiko Kusaka, Mitsuhiro Shimura, Shuichi Aoki, Daisuke Douchi, Takayuki Miura, Shimpei Maeda, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(3):203-209. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0020
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 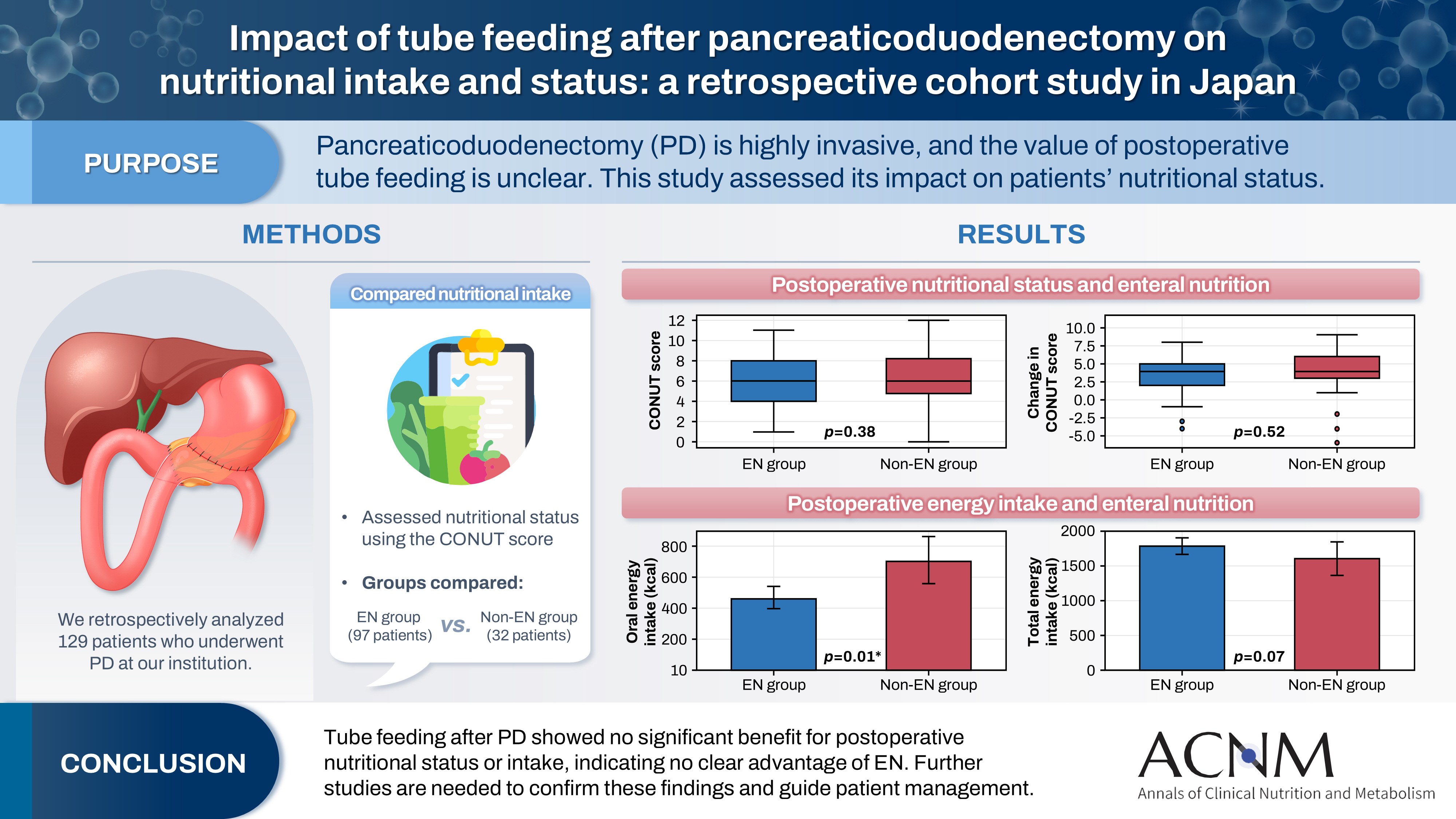
- Purpose
Pancreaticoduodenectomy (PD) is one of the most invasive procedures in gastrointestinal surgery. However, the clinical significance of postoperative tube feeding remains unclear. This study investigated the impact of enteral nutrition (EN) on the postoperative nutritional status of patients undergoing PD.
Methods
We retrospectively analyzed 129 patients who underwent PD at Tohoku University Hospital. Nutritional intake and status, evaluated using the Controlling Nutritional Status score, were compared between two groups: an EN group (97 patients) and a non-EN group (32 patients).
Results
There were no significant differences between the two groups in age, sex, body mass index, underlying diseases, operative duration, blood loss, postoperative pancreatic fistula, postoperative complications, delayed gastric emptying, or length of hospital stay. Although the EN group showed improvements in nutritional status both at discharge and compared with preoperative values, none of these changes reached statistical significance. Oral caloric intake was significantly higher in the non-EN group (P=0.01). In contrast, total energy intake was higher in the EN group, but this difference did not reach statistical significance (P=0.07).
Conclusion
Tube feeding after PD did not significantly influence postoperative nutritional status or overall nutritional intake. These findings suggest that EN offers no clear advantage over other approaches; however, further research is warranted to validate these results, refine existing guidelines, and optimize postoperative patient management.
- 643 View
- 12 Download

Interesting image
- Penetration of a nasogastric tube by a stylet during insertion
- Akihide Takami, Haruka Tsuji, Kazuya Omura
- Ann Clin Nutr Metab 2025;17(3):210-211. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0029
- 352 View
- 8 Download

Correction
- Correction: article type revision
- Editorial Office, Annals of Clinical Nutrition and Metabolism
- Ann Clin Nutr Metab 2025;17(3):212-212. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0033
- Corrects: Ann Clin Nutr Metab 2025;17(1):3
- 336 View
- 9 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN

 First
First Prev
Prev


