Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 13(2); 2021 > Article
- Original Article Clinical Significance of Malnutrition Risk in Severe Trauma Patients: A Single-Center Study
-
Hohyun Kim, M.D.1,2
 , Kum-Hee Hong, M.S.2,3
, Kum-Hee Hong, M.S.2,3 , Inah Choi, M.S.2,4
, Inah Choi, M.S.2,4 , Kyung-A Lee, M.S.2,5
, Kyung-A Lee, M.S.2,5 , Geun Am Song, M.D.2,6
, Geun Am Song, M.D.2,6
-
Annals of Clinical Nutrition and Metabolism 2021;13(2):68-74.
DOI: https://doi.org/10.15747/ACNM.2021.13.2.68
Published online: December 31, 2021
1Department of Trauma and Surgical Critical Care, Pusan National University Hospital, Busan, Korea
2Nutrition Support Team, Pusan National University Hospital, Busan, Korea
3Department of Nursing, Pusan National University Hospital, Busan, Korea
4Department of Pharmacy, Pusan National University Hospital, Busan, Korea
5Department of Nutrition, Pusan National University Hospital, Busan, Korea
6Department of Internal Medicine, Pusan National University Hospital, Busan, Korea
- Corresponding author: Hohyun Kim E-mail gskhh@naver.com ORCID https://orcid.org/0000-0001-9434-8654
© The Korean Society of Surgical Metabolism and Nutrition and The Korean Society for Parenteral and Enteral Nutrition
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 2,314 Views
- 26 Download
Abstract
-
Purpose A suboptimal nutritional status is often observed among hospitalized patients across all medical/surgical specialties. The objective of the present study was to (1) analyze the prevalence of malnutrition in severe trauma patients and (2) evaluate the relationship between malnutrition and select clinical outcomes.
-
Materials and Methods This retrospective study was conducted between October 2015 and March 2017 at the Pusan National University Hospital Trauma Center. Of a total of 3,560 patients, 945 were enrolled in this study. Patients were checked for malnutrition using a nutrition assessment tool by the hospital nutrition support team. The parameters assessed included serum albumin, the ratio of actual body weight to ideal body weight (%), total lymphocyte count, appetite, and gastrointestinal problems. Clinical outcomes under consideration included 1) mortality, 2) length of hospitalization, and 3) length of stay in the intensive care unit (ICU).
-
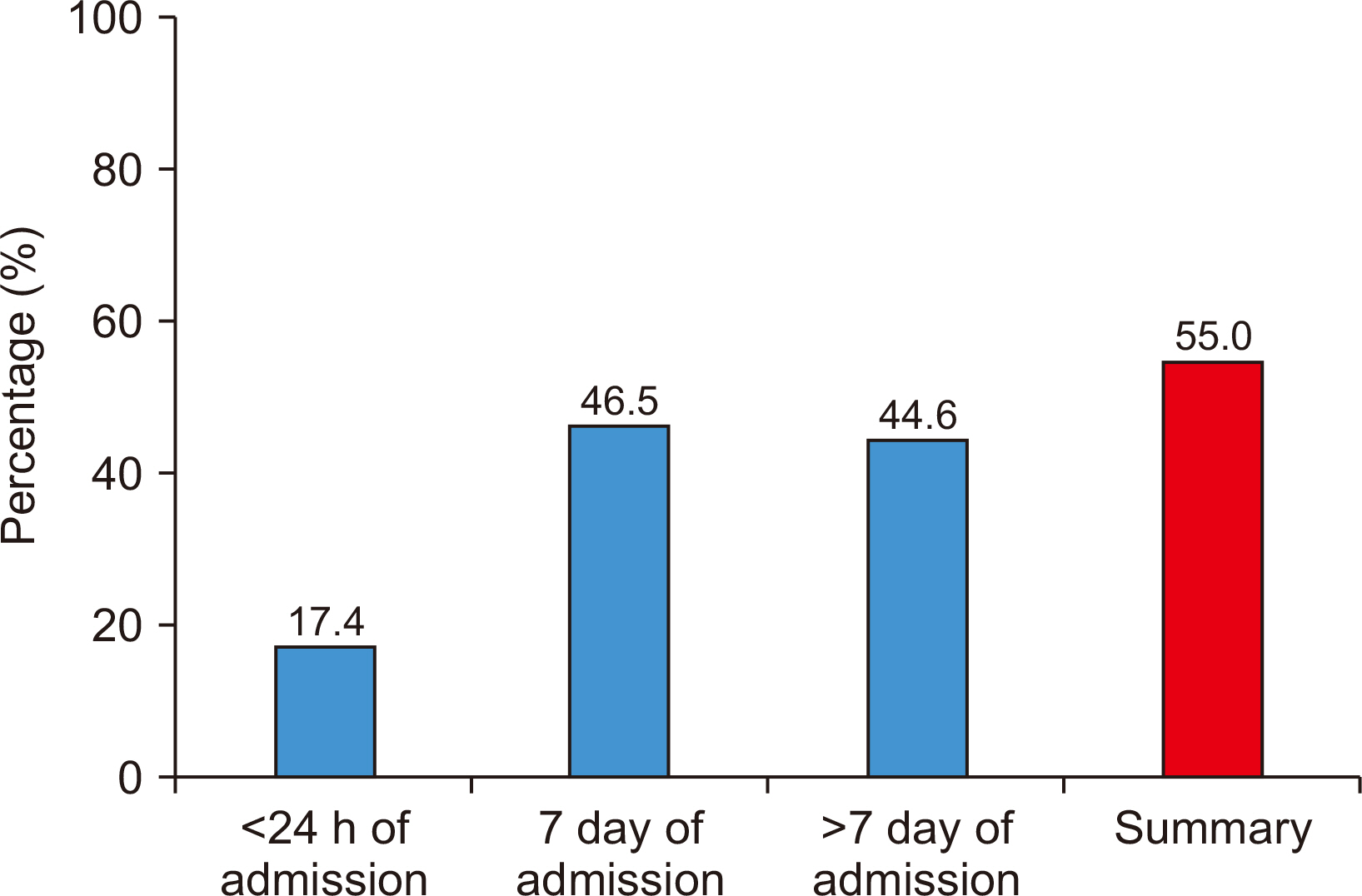
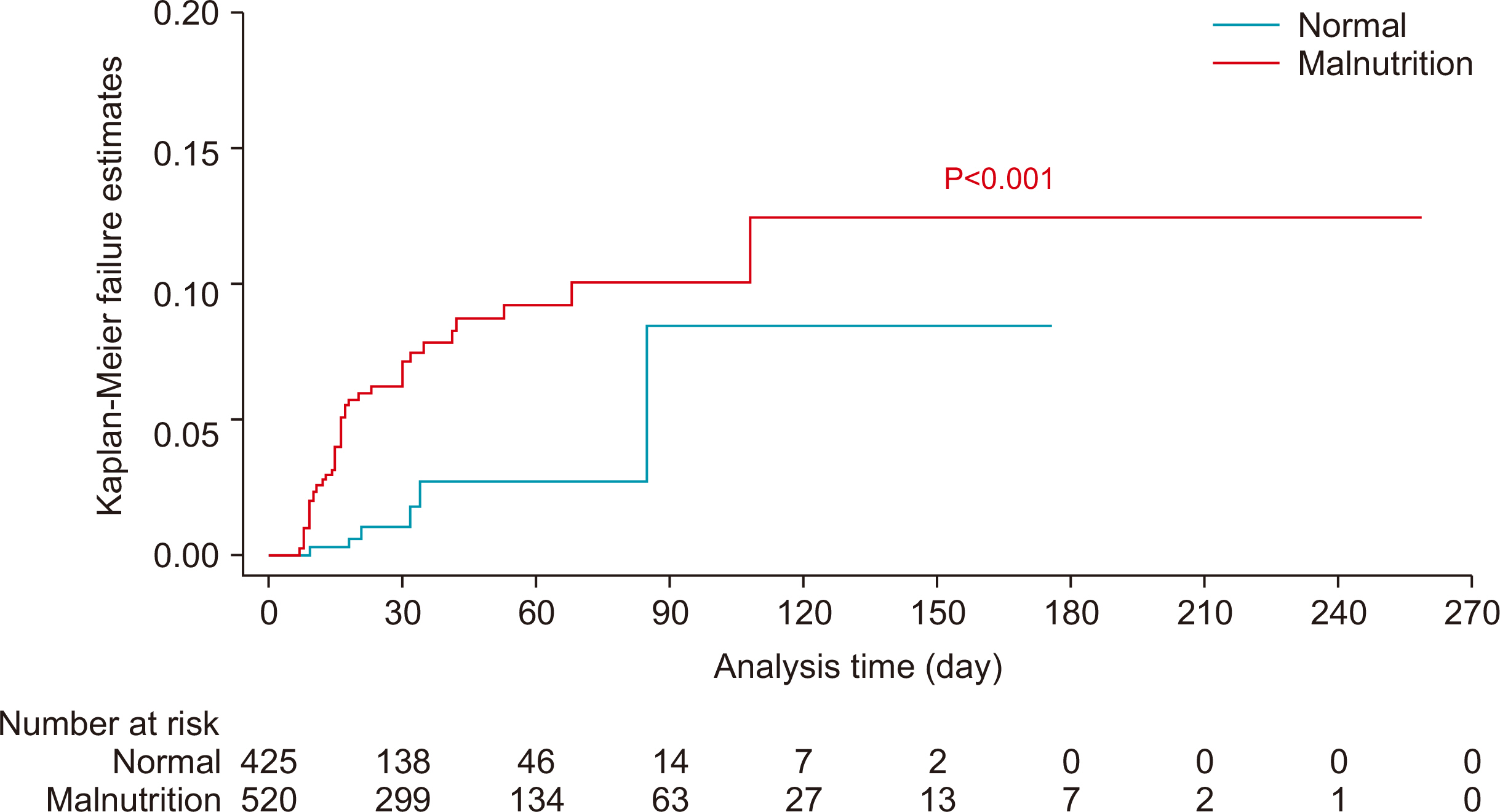
Results The total prevalence of malnutrition in hospitalized trauma patients was 55.0% (n=520). Malnutrition risk was the independent prognostic factor of mortality in severe trauma patients (adjusted odds ratio [OR]=3.440; 95% confidence interval [CI]=1.401~8.447, P=0.007). Risk factors of malnutrition were age over 65 years (adjusted OR=2.393; 95% CI=1.699~3.370, P<0.001), injury severity score (adjusted OR=1.034, 95% CI=1.012~1.056, P=0.002), length of hospitalization (adjusted OR=1.104; 95% CI=1.007~1.020, P<0.001), and length of stay in the ICU (adjusted OR=1.050; 95% CI=1.029~1.072, P<0.001).
-
Conclusion Malnutrition is widespread in hospitalized patients with severe trauma and results in suboptimal clinical outcomes. Thus, patients at high risk of malnutrition should be monitored carefully during hospitalization.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
CONCLUSION
AUTHOR CONTRIBUTIONS
Conceptualization: HK, KHH. Data curation: KHH. Formal analysis: HK. Investigation: HK. Methodology: KHH, IC, KAL. Project administration: HK, GAS. Resources: KHH, IC, KAL. Supervision: GAS. Validation: KHH, KAL. Visualization: HK. Writing – original draft: HK. Writing – review & editing: KHH, IC, KAL, GAS.
CONFLICTS OF INTEREST
The authors of this manuscript have no conflicts of interest to disclose.
| Variable | Total group (n=945) | P-value | |
|---|---|---|---|
|
|
|||
| Survivor group (n=899) | Non-survivor group (n=46) | ||
| Malnutrition risk | |||
| <24 h of admission | 149 (16.6) | 15 (32.6) | 0.005 |
| 7 day of admission | 404 (44.9) | 35 (76.1) | <0.001 |
| >7 day of admissiona | 162 (41.8) | 22 (88.0) | <0.001 |
| Totalb | 480 (53.4) | 40 (87.0) | <0.001 |
| Age (≥65 yr) | 213 (23.7) | 23 (50.0) | <0.001 |
| Sex (male:female) | 704:195 | 36:10 | 0.994 |
| ISS | 24 (19~29) | 29 (25~34) | <0.001 |
| Head AIS | 3 (0~4) | 4 (3~5) | <0.001 |
| Abdomen AIS | 0 (0~2) | 0 (0~2) | 0.281 |
| GCS | 15 (12~15) | 9 (5~14) | <0.001 |
| Length of hospitalization (day) | 28 (18~51) | 16 (10~30) | <0.001 |
| Length of stay in ICU (day) | 5 (2~14) | 16 (11~30) | <0.001 |
Values are presented as number (%) or median (interquartile range).
ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.
aSurvivor group (n=388), non-survivor group (n=25), Total (n=413).
bNutritional screening showed the positive malnutrition risk on <24 hours and/or 7 days and/or >7 days of admission.
| Variable | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Age (≥65 yr) | 3.221 (1.771~5.857) | <0.001 | 3.634 (1.842~7.170) | <0.001 |
| ISS | 1.049 (1.021~1.078) | 0.001 | ||
| Head AIS | 1.452 (1.207~1.747) | <0.001 | ||
| GCS | 0.818 (0.762~0.878) | <0.001 | 0.812 (0.752~0.877) | <0.001 |
| Malnutrition riska | 5.819 (2.443~13.863) | <0.001 | 3.440 (1.401~8.447) | 0.007 |
- 1. Thomas MN, Kufeldt J, Kisser U, Hornung HM, Hoffmann J, Andraschko M, et al. Effects of malnutrition on complication rates, length of hospital stay, and revenue in elective surgical patients in the G-DRG-system. Nutrition 2016;32:249-54. ArticlePubMed
- 2. Geurden B, Franck E, Weyler J, Ysebaert D. The risk of malnutrition in community-living elderly on admission to hospital for major surgery. Acta Chir Belg 2015;115:341-7. ArticlePubMed
- 3. Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr 2006;25:563-72. ArticlePubMed
- 4. Hertlein L, Kirschenhofer A, Fürst S, Beer D, Göβ C, Lenhard M, et al. Malnutrition and clinical outcome in gynecologic patients. Eur J Obstet Gynecol Reprod Biol 2014;174:137-40. ArticlePubMed
- 5. Karl A, Staehler M, Bauer R, Tritschler S, Hocaoglu Y, Buchner A, et al. Malnutrition and clinical outcome in urological patients. Eur J Med Res 2011;16:469-72. ArticlePubMedPMC
- 6. Felder S, Lechtenboehmer C, Bally M, Fehr R, Deiss M, Faessler L, et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition 2015;31:1385-93. ArticlePubMed
- 7. Ihle C, Freude T, Bahrs C, Zehendner E, Braunsberger J, Biesalski HK, et al. Malnutrition - an underestimated factor in the inpatient treatment of traumatology and orthopedic patients: a prospective evaluation of 1055 patients. Injury 2017;48:628-36. ArticlePubMed
- 8. Mogensen KM, Robinson MK, Casey JD, Gunasekera NS, Moromizato T, Rawn JD, et al. Nutritional status and mortality in the critically ill. Crit Care Med 2015;43:2605-15. ArticlePubMed
- 9. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr 2003;22:235-9. ArticlePubMed
- 10. Amaral TF, Matos LC, Tavares MM, Subtil A, Martins R, Nazaré M, et al. The economic impact of disease-related malnutrition at hospital admission. Clin Nutr 2007;26:778-84. ArticlePubMed
- 11. Clendenen N, Nunns GR, Moore EE, Reisz JA, Gonzalez E, Peltz E, et al. Hemorrhagic shock and tissue injury drive distinct plasma metabolome derangements in swine. J Trauma Acute Care Surg 2017;83:635-42. ArticlePubMedPMC
- 12. Goiburu ME, Goiburu MM, Bianco H, Díaz JR, Alderete F, Palacios MC, et al. The impact of malnutrition on morbidity, mortality and length of hospital stay in trauma patients. Nutr Hosp 2006;21:604-10. ArticlePubMed
- 13. Rogobete AF, Sandesc D, Papurica M, Stoicescu ER, Popovici SE, Bratu LM, et al. The influence of metabolic imbalances and oxidative stress on the outcome of critically ill polytrauma patients: a review. Burns Trauma 2017;5:8.ArticlePubMedPMCPDF
- 14. Wilson JM, Lunati MP, Grabel ZJ, Staley CA, Schwartz AM, Schenker ML. Hypoalbuminemia is an independent risk factor for 30-day mortality, postoperative complications, readmission, and reoperation in the operative lower extremity orthopaedic trauma patient. J Orthop Trauma 2019;33:284-91. ArticlePubMed
- 15. Mueller C, Compher C, Ellen DM. American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr 2011;35:16-24. ArticlePubMed
- 16. Lochs H, Allison SP, Meier R, Pirlich M, Kondrup J, Schneider S, et al. Introductory to the ESPEN guidelines on enteral nutrition: terminology, definitions and general topics. Clin Nutr 2006;25:180-6. ArticlePubMed
- 17. Müller FS, Meyer OW, Chocano-Bedoya P, Schietzel S, Gagesch M, Freystaetter G, et al. Impaired nutritional status in geriatric trauma patients. Eur J Clin Nutr 2017;71:602-6. ArticlePubMedPDF
- 18. Goisser S, Schrader E, Singler K, Bertsch T, Gefeller O, Biber R, et al. Malnutrition according to mini nutritional assessment is associated with severe functional impairment in geriatric patients before and up to 6 months after hip fracture. J Am Med Dir Assoc 2015;16:661-7. ArticlePubMed
- 19. Chakravarty C, Hazarika B, Goswami L, Ramasubban S. Prevalence of malnutrition in a tertiary care hospital in India. Indian J Crit Care Med 2013;17:170-3. ArticlePubMedPMC
- 20. Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr 2008;27:5-15. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

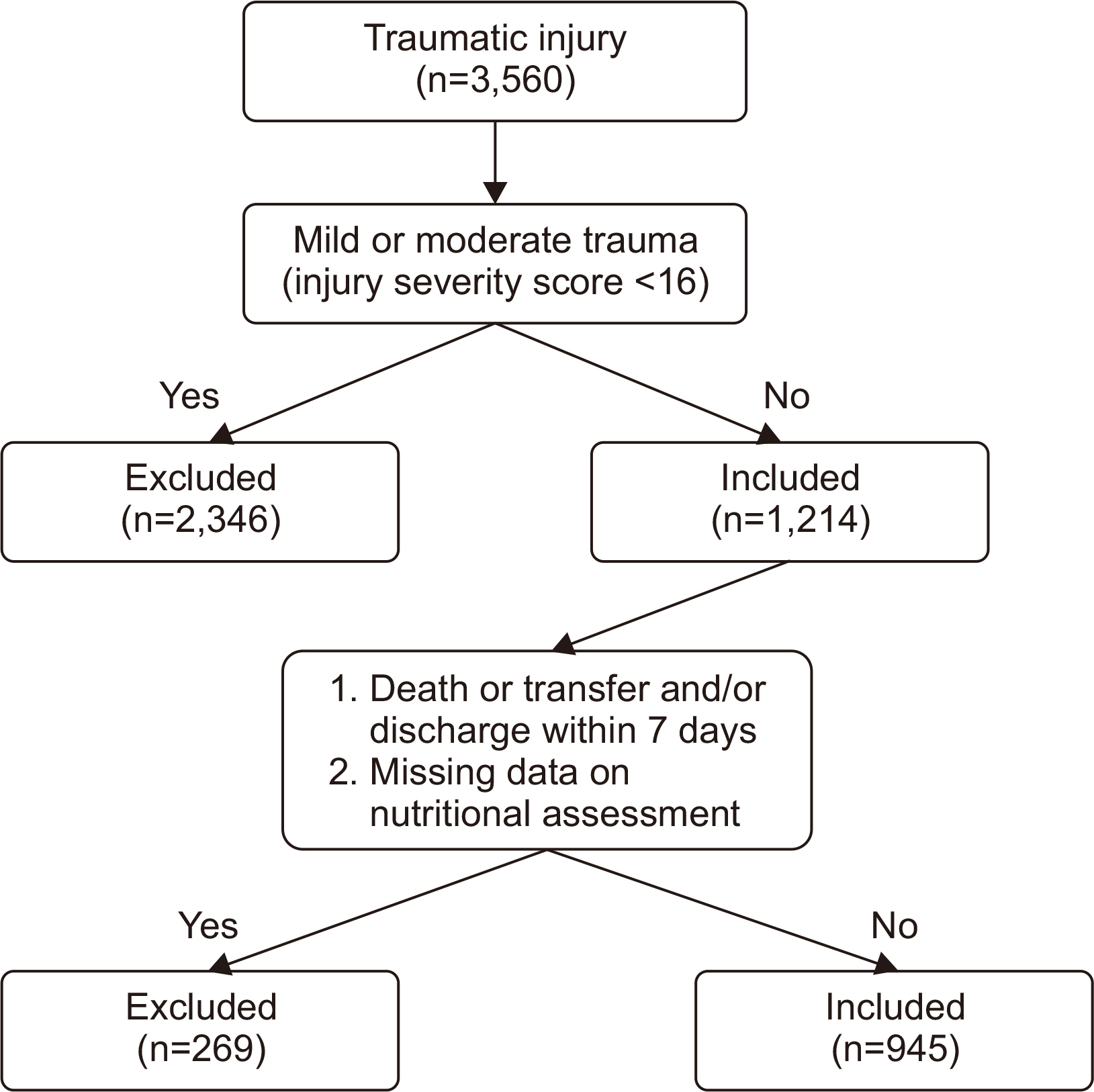
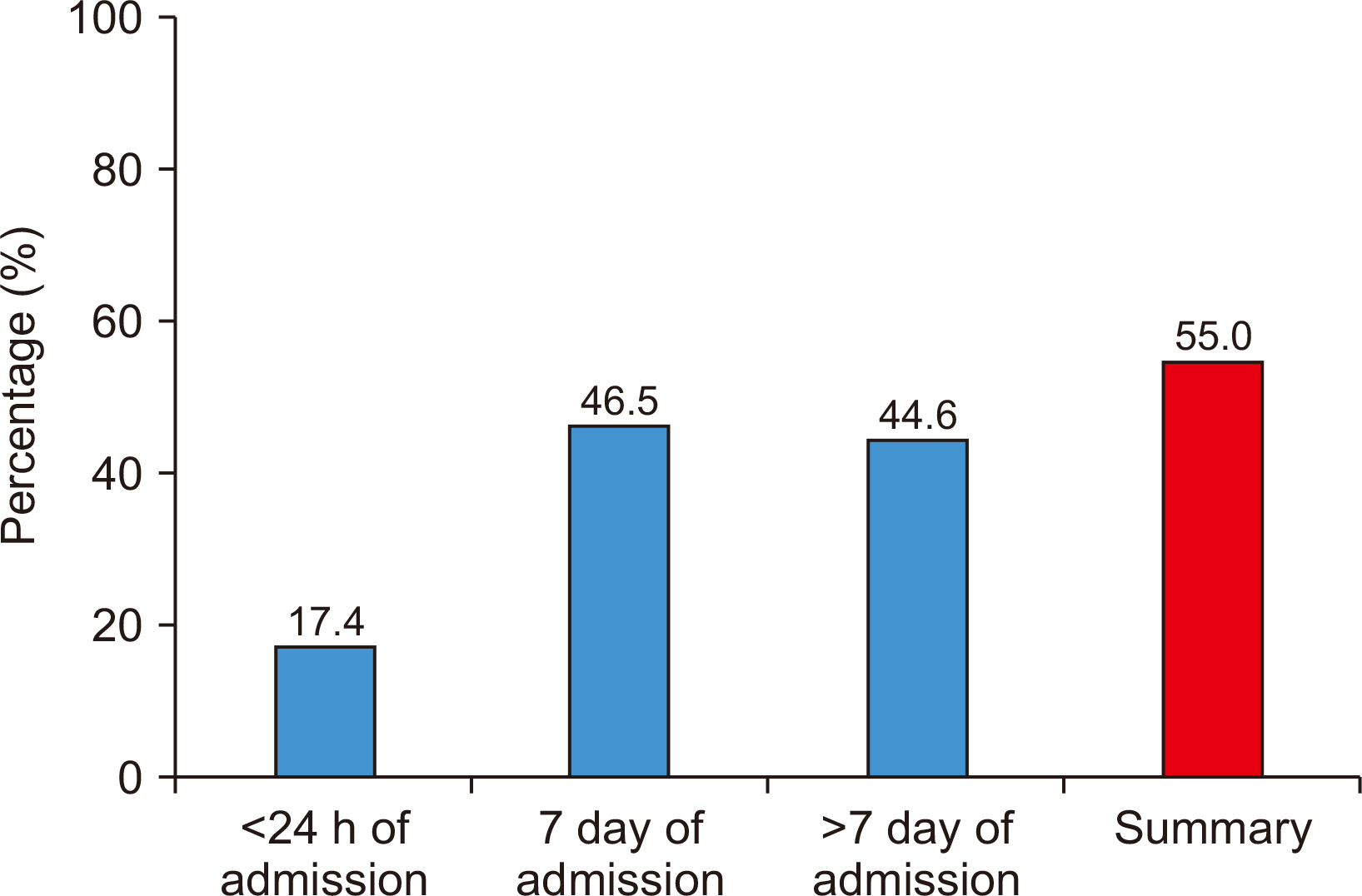
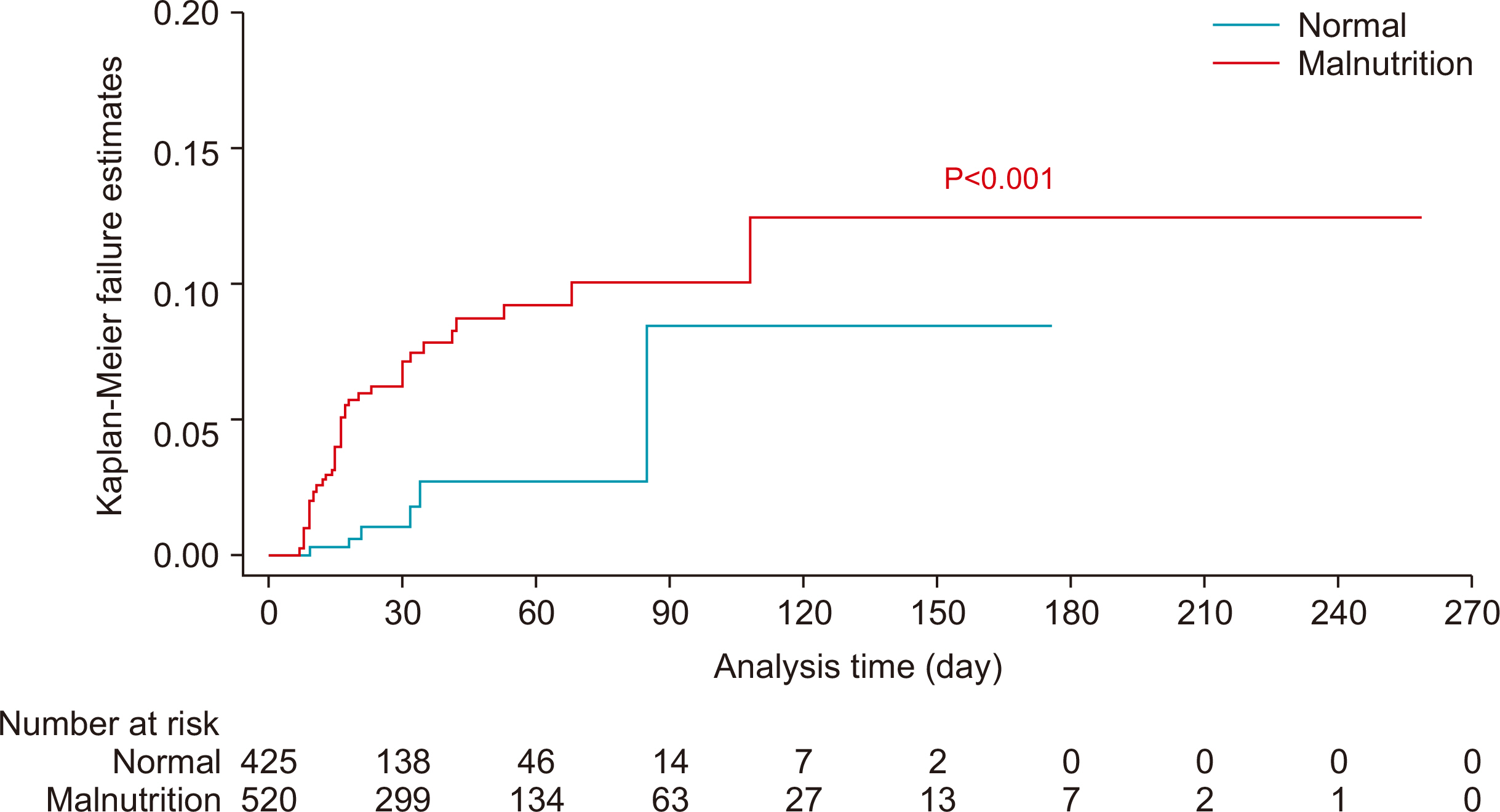
Fig. 1
Fig. 2
Fig. 3
Nutrition assessment tool in Pusan National University Hospital nutrition support team
| Variable | Degree of malnutrition | Note | |||
|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | ||
| Albumin (g/dL) | >3.2 | 3.2~2.8 | 2.7~2.1 | <2.1 | N/A |
| Score | 0 | 2 | 4 | 6 | 0 |
| IBW (%) | ≥90 | 89.9~80 | 79.9~70 | <70 | N/A |
| Score | 0 | 1 | 2 | 3 | 3 |
| TLC (cell/mm3) | >1,500 | 1,200~1,500 | 800~1,199.9 | <800 | N/A |
| Score | 0 | 1 | 2 | 0 | |
| Appetite | Good or usual | Bad | N/A | ||
| Score | 0 | 2 | 0 | ||
| Number of GI problem | None | 1~2 | 3 | N/A | |
| Score | 0 | 1 | 2 | 0 | |
Positive malnutrition risk: ≥4 points.
N/A = non-applicable; IBW = ideal body weight; TLC = total lymphocyte count; GI = gastrointestinal.
Clinical characteristics of patients with severe trauma
| Variable | Total group (n=945) | P-value | |
|---|---|---|---|
| Survivor group (n=899) | Non-survivor group (n=46) | ||
| Malnutrition risk | |||
| <24 h of admission | 149 (16.6) | 15 (32.6) | 0.005 |
| 7 day of admission | 404 (44.9) | 35 (76.1) | <0.001 |
| >7 day of admission |
162 (41.8) | 22 (88.0) | <0.001 |
| Total |
480 (53.4) | 40 (87.0) | <0.001 |
| Age (≥65 yr) | 213 (23.7) | 23 (50.0) | <0.001 |
| Sex (male:female) | 704:195 | 36:10 | 0.994 |
| ISS | 24 (19~29) | 29 (25~34) | <0.001 |
| Head AIS | 3 (0~4) | 4 (3~5) | <0.001 |
| Abdomen AIS | 0 (0~2) | 0 (0~2) | 0.281 |
| GCS | 15 (12~15) | 9 (5~14) | <0.001 |
| Length of hospitalization (day) | 28 (18~51) | 16 (10~30) | <0.001 |
| Length of stay in ICU (day) | 5 (2~14) | 16 (11~30) | <0.001 |
Values are presented as number (%) or median (interquartile range).
ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.
aSurvivor group (n=388), non-survivor group (n=25), Total (n=413).
bNutritional screening showed the positive malnutrition risk on <24 hours and/or 7 days and/or >7 days of admission.
Univariable and multiple logistic regression analysis for mortality (n=945)
| Variable | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Age (≥65 yr) | 3.221 (1.771~5.857) | <0.001 | 3.634 (1.842~7.170) | <0.001 |
| ISS | 1.049 (1.021~1.078) | 0.001 | ||
| Head AIS | 1.452 (1.207~1.747) | <0.001 | ||
| GCS | 0.818 (0.762~0.878) | <0.001 | 0.812 (0.752~0.877) | <0.001 |
| Malnutrition risk |
5.819 (2.443~13.863) | <0.001 | 3.440 (1.401~8.447) | 0.007 |
OR = odds ratio; CI = confidence interval; ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale.
aNutritional screening showed the positive malnutrition risk on <24 hours and/or 7 days and/or >7 days of admission.
Demographics of patients with severe trauma according to malnutrition risk
| Variables | Total group (n=945) | P-value | |
|---|---|---|---|
| Normal group (n=425) | Malnutrition risk group (n=520) | ||
| Age (≥65 yr) | 72 (16.9) | 164 (31.5) | <0.001 |
| Sex (male:female) | 347:78 | 393:127 | 0.024 |
| ISS | 22 (17~27) | 25 (22~29) | <0.001 |
| Head AIS | 3 (0~4) | 3 (0~4) | 0.653 |
| Abdomen AIS | 0 (0~2) | 2 (0~2) | 0.005 |
| GCS | 15 (13~15) | 15 (9~15) | <0.001 |
| Length of hospitalization (day) | 22 (15~34) | 35 (20~61) | <0.001 |
| Length of stay in ICU (day) | 3 (2~8) | 10 (4~20) | <0.001 |
Values are presented as number (%) or median (interquartile range).
ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.
Univariable and multiple logistic regression analyses for malnutrition risk (n=945)
| Variables | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value |
|---|---|---|---|---|
| Age (≥65 yr) | 2.259 (1.650~3.091) | <0.001 | 2.393 (1.699~3.370) | <0.001 |
| Male | 0.696 (0.507~0.955) | 0.025 | ||
| ISS | 1.056 (1.036~1.076) | <0.001 | 1.034 (1.012~1.056) | 0.002 |
| Abdomen AIS | 1.135 (1.039~1.240) | 0.005 | ||
| GCS | 0.917 (0.882~0.953) | <0.001 | ||
| Length of hospitalization | 1.019 (1.014~1.025) | <0.001 | 1.014 (1.007~1.020) | <0.001 |
| Length of stay in ICU | 1.066 (1.050~1.083) | <0.001 | 1.050 (1.029~1.072) | <0.001 |
OR = odds ratio; CI = confidence interval; ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.
Positive malnutrition risk: ≥4 points. N/A = non-applicable; IBW = ideal body weight; TLC = total lymphocyte count; GI = gastrointestinal.
Values are presented as number (%) or median (interquartile range). ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit. aSurvivor group (n=388), non-survivor group (n=25), Total (n=413). bNutritional screening showed the positive malnutrition risk on <24 hours and/or 7 days and/or >7 days of admission.
OR = odds ratio; CI = confidence interval; ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale. aNutritional screening showed the positive malnutrition risk on <24 hours and/or 7 days and/or >7 days of admission.
Values are presented as number (%) or median (interquartile range). ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.
OR = odds ratio; CI = confidence interval; ISS = injury severity score; AIS = abbreviated injury scale; GCS = Glasgow coma scale; ICU = intensive care unit.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN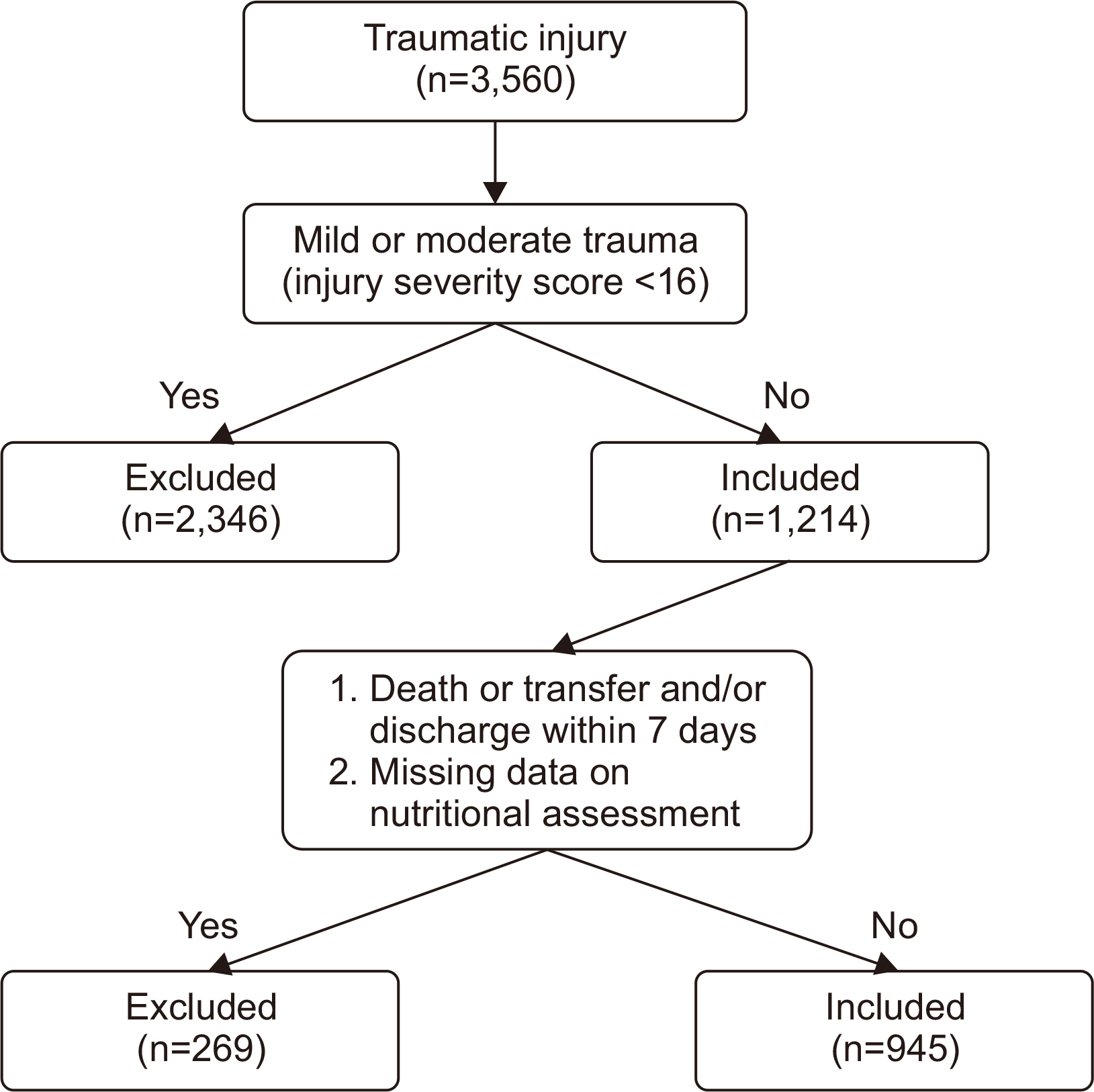
 Cite
Cite

