Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
Original Articles
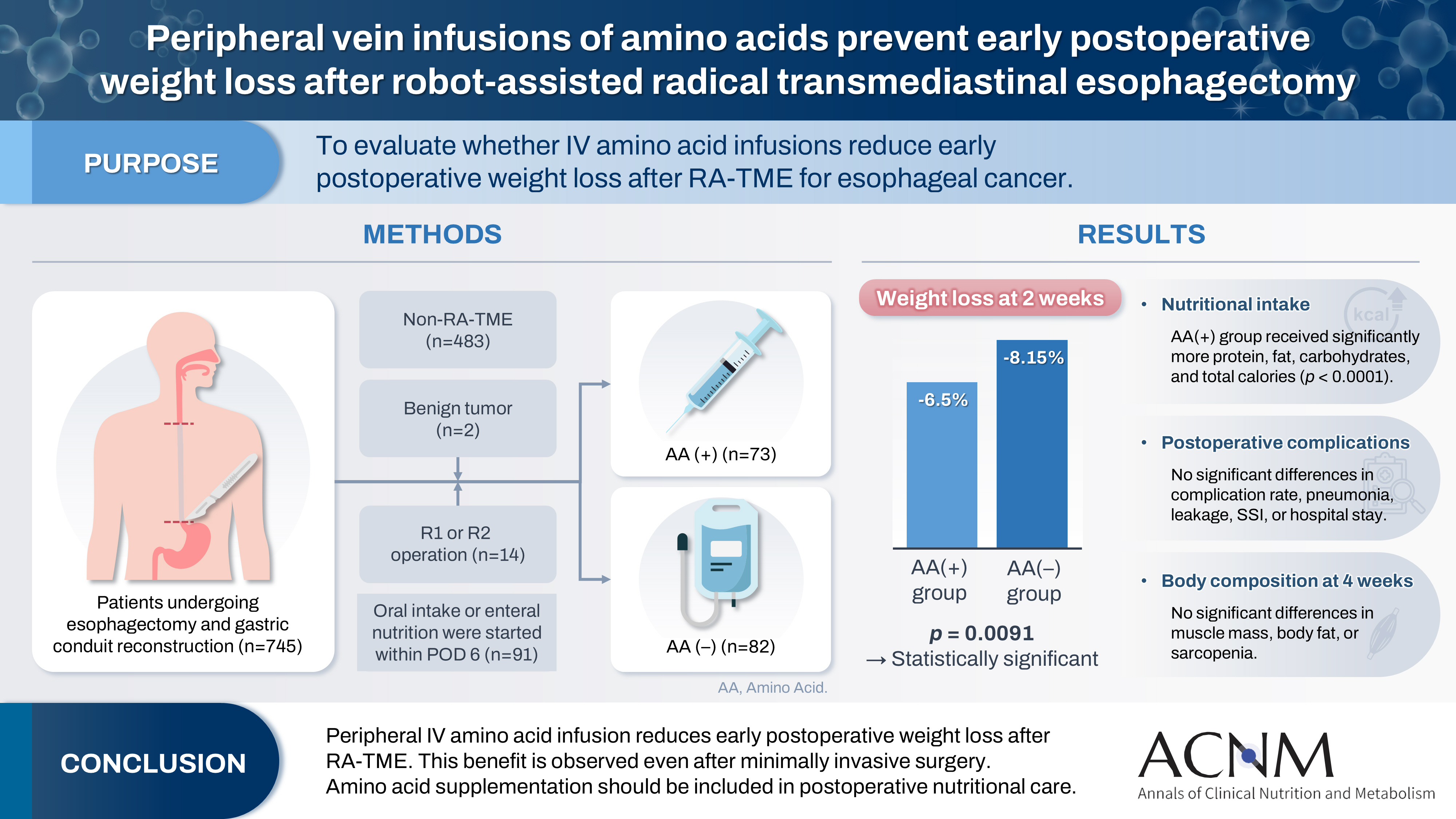
- Peripheral vein infusions of amino acids prevent early postoperative weight loss after robot-assisted radical transmediastinal esophagectomy: a retrospective study in Japan
- Tomonori Narita, Kazuhiko Fukatsu, Satoshi Murakoshi, Reo Inoue, Kenichi Kono, Midori Noguchi, Nana Matsumoto, Shoh Yajima, Koichi Yagi, Yoshifumi Baba
- Ann Clin Nutr Metab 2025;17(2):149-155. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0012
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 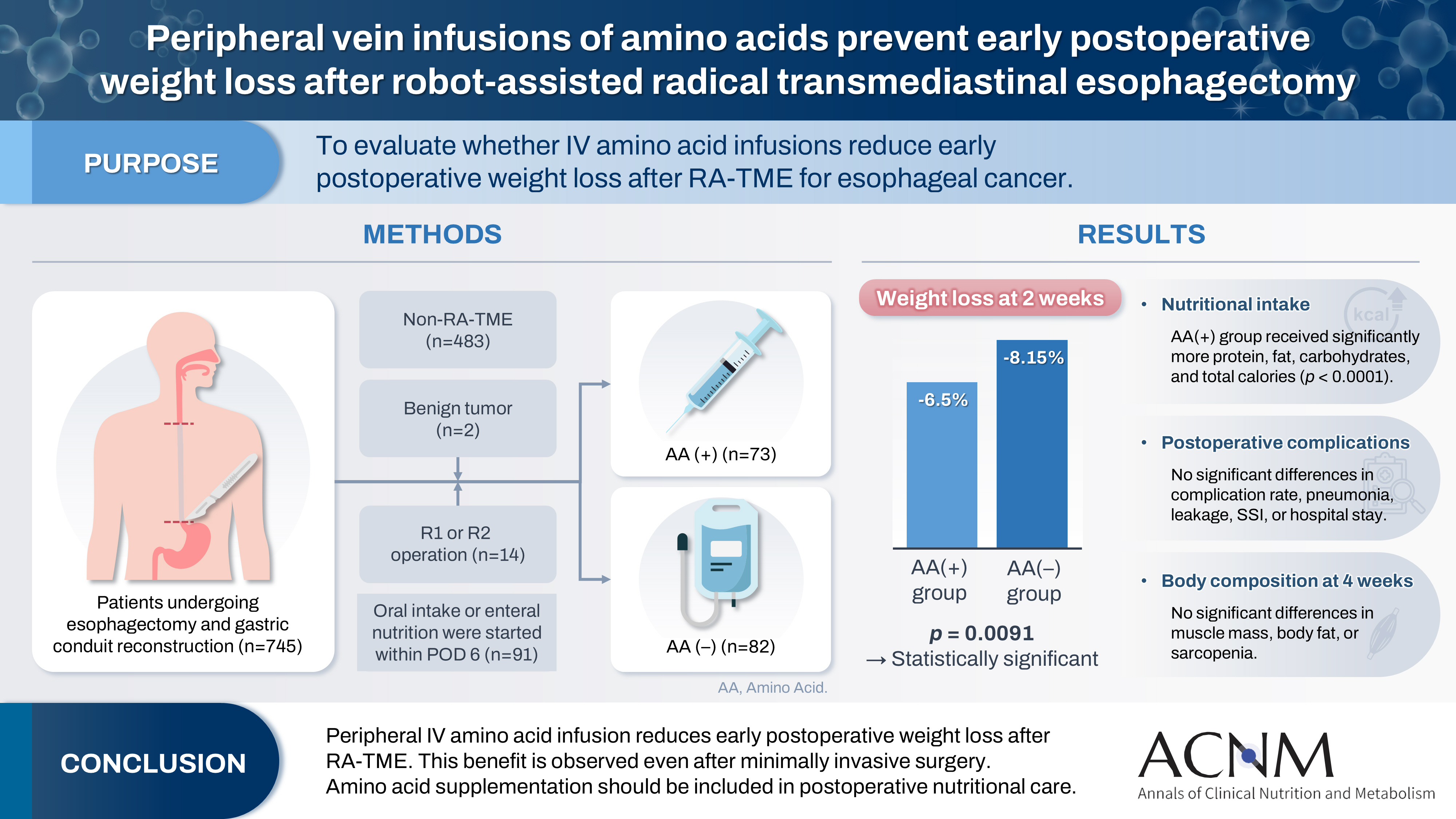
- Purpose
Postoperative body weight loss (PBWL) is linked to poor long-term outcomes following esophagectomy for esophageal cancer, making perioperative nutrition critically important. Although minimally invasive procedures such as robot-assisted radical transmediastinal esophagectomy (RA-TME) have become more prevalent, less attention has been paid to perioperative nutritional management. This study evaluates the impact of intravenous (IV) amino acid infusions on PBWL in patients undergoing RA-TME.
Methods
We retrospectively analyzed 155 patients who underwent RA-TME for esophageal or esophagogastric junction cancer at our hospital between 2011 and 2022. Patients were divided into two groups: AA(+) (n=73, received IV amino acids between postoperative days 1–6) and AA(–) (n=82, did not receive IV amino acids). Oral or enteral nutrition was withheld until postoperative day 6. We compared nutrient intake, postoperative outcomes, and nutritional status between groups.
Results
Patient backgrounds, surgical outcomes, and complication rates were similar in both groups. However, the AA(+) group received significantly greater energy and nutrient intake. PBWL at 2 weeks post-surgery was significantly lower in the AA(+) group than in the AA(–) group (6.50% vs. 8.15%, P=0.0091).
Conclusion
IV amino acid infusion may help mitigate early PBWL after RA-TME.
- 1,335 View
- 17 Download

- Insulinotropic action of L-carnitine and branched-chain amino acids following energy intake in healthy, young Japanese women: a non-randomized controlled trial
- Yoichi Sakurai, Hideyuki Namba, Satoshi Odo
- Ann Clin Nutr Metab 2025;17(2):139-148. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0011
-
 Abstract
Abstract
 PDF
PDF - Purpose
The present study uses healthy human volunteers to examine the insulinotropic action of L-carnitine and branched-chain amino acids (BCAAs) after energy intake.
Methods
A total of 39 young, healthy human volunteers were assigned to receive oral doses of either L-carnitine alone (L group, n=10) or L-carnitine combined with a single or long-term continuous dose of BCAAs. Controls (C group, n=16) received none of these. L-carnitine was administered orally at 1,000 mg/d for 14 days, and BCAA was administered orally either once just before exercise (L+SB group, n=6), or every day for 14 days (L+CB group, n=7) until 2 days before the experiment. After overnight fasting, 200 kcal of glucose and oral nutritional supplement were administered to prevent hypoglycemia. Blood glucose, free-fatty acid, and serum insulin levels were measured to examine the insulinotropic action before and after exercise.
Results
Blood glucose and serum insulin levels in the L group were significantly lower than those in the C group. While the serum insulin levels were higher after energy administration than those in the fasting state in all groups, these were significantly higher in the L+SB group and in the L+CB group compared with those in the L group. The insulinotropic action after energy intake remained even after the repeated administration of BCAA discontinued 2 days before the experi¬ment and even after serum BCAA levels remained the same.
Conclusion
While the insulinotropic action appeared after a single dose of BCAA, it was also potentiated by long-term repeated oral administration of BCAA.
- 1,215 View
- 13 Download

Review Article
- Muscle Protein Metabolism in Critically Illness
- Min Chang Kang
- Surg Metab Nutr 2020;11(2):35-39. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.35
-
 Abstract
Abstract
 PDF
PDF - Most patients experience a considerable amount of muscle wasting during critical care. A decrease in muscle mass causes weakness which inevitably leads to delayed recovery. Since muscle also plays an important role in protein metabolism, metabolic instability increases as muscle mass decreases. Accordingly, various treatments have been attempted to maintain muscle mass and function in critically ill patients; however, it is still difficult to prevent muscle loss. It is known that muscle wasting in critical illness is primarily due to increased muscle protein breakdown rather than a decrease in muscle protein synthesis. Nutritional therapy and rehabilitation are fundamentally important, but additional anabolic agents may be needed to overcome anabolic resistance. In this review, we will learn about muscle protein metabolism in critically ill patients and how various treatments affect muscle protein metabolism.
-
Citations
Citations to this article as recorded by- Combined intravenous bolus amino acid supplementation and mobilization on early muscle loss in critically ill adults: A randomized controlled trial
Lizl Veldsman, Guy A. Richards, Daniel Nel, Tertius A. Kohn, Renée Blaauw
Journal of Parenteral and Enteral Nutrition.2026; 50(2): 170. CrossRef - Low protein content of plant-derived nutrition limits the protein transition in hospitalized patients: Results from an observational study
M.A. van Bree, B.C. Schouten, E.S. Wolters, M.R. Soeters, H.M. Kruizenga
Clinical Nutrition ESPEN.2025; 69: 311. CrossRef - Combined Protein, Probiotics, and Exercise Therapy for Sarcopenia: A Comprehensive Review
Ryuk Jun Kwon, Mohammad Al Mijan, Soo Min Son, Wanho Yoo, Taehwa Kim
Cells.2025; 14(17): 1375. CrossRef - Double-Edge Effects of Leucine on Cancer Cells
Burkitkan Akbay, Zhannur Omarova, Alexander Trofimov, Bayan Sailike, Orynbassar Karapina, Ferdinand Molnár, Tursonjan Tokay
Biomolecules.2024; 14(11): 1401. CrossRef - Compartmental analysis: a new approach to estimate protein breakdown and meal response in health and critical illness
Nicolaas E. P. Deutz, Mariëlle P. K. J. Engelen
Frontiers in Nutrition.2024;[Epub] CrossRef - Amino acid kinetics in the critically ill
Nicolaas E.P. Deutz, Krista L. Haines, Paul E. Wischmeier, Mariëlle P.K.J. Engelen
Current Opinion in Clinical Nutrition & Metabolic Care.2024; 27(1): 61. CrossRef
- Combined intravenous bolus amino acid supplementation and mobilization on early muscle loss in critically ill adults: A randomized controlled trial
- 4,771 View
- 34 Download
- 6 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


