Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 17(1); 2025 > Article
- Original Article Impact of postoperative nutritional status on the patients’ clinical outcomes and knee biomechanics following total knee arthroplasty in Japan: a prospective cohort study
-
Kenichi Kono1,2
 , Tetsuya Tomita3,4
, Tetsuya Tomita3,4 , Takaharu Yamazaki5
, Takaharu Yamazaki5 , Masashi Tamaki3
, Masashi Tamaki3 , Shuji Taketomi2
, Shuji Taketomi2 , Ryota Yamagami2
, Ryota Yamagami2 , Reo Inoue1
, Reo Inoue1 , Yuki Taniguchi1,2
, Yuki Taniguchi1,2 , Sakae Tanaka2
, Sakae Tanaka2 , Kazuhiko Fukatsu1
, Kazuhiko Fukatsu1
-
Annals of Clinical Nutrition and Metabolism 2025;17(1):50-57.
DOI: https://doi.org/10.15747/ACNM.24.019
Published online: April 1, 2025
1Surgical Center, The University of Tokyo Hospital, Tokyo, Japan
2Department of Orthopedic Surgery, Faculty of Medicine, The University of Tokyo, Tokyo, Japan
3Department of Orthopedic Biomaterial Science, Osaka University Graduate School of Medicine, Suita, Japan
4Master Course of Health Sciences, Graduate School of Health Sciences, Morinomiya University of Medical Sciences, Osaka, Japan
5Department of Information Systems, Faculty of Engineering, Saitama Institute of Technology, Fukaya, Japan
- Corresponding author: Kenichi Kono, email: kkouno_tki@yahoo.co.jp
© 2025 Korean Society of Surgical Metabolism and Nutrition · Korean Society for Parenteral and Enteral Nutrition · Asian Society of Surgical Metabolism and Nutrition · Japanese Society for Surgical Metabolism and Nutrition
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 172 Views
- 5 Download
Abstract
-
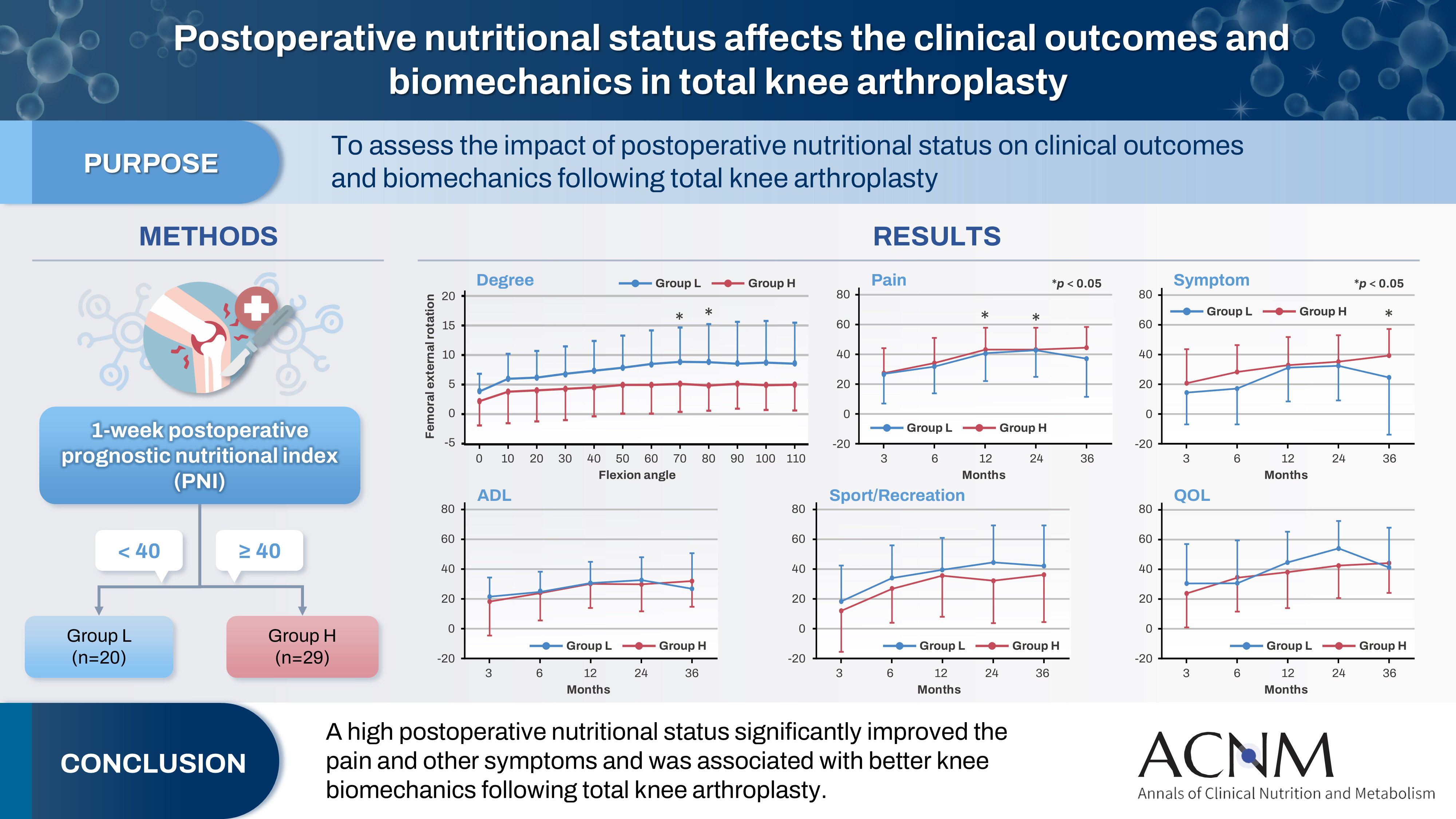
Purpose The impact of postoperative nutritional status on clinical outcomes and biomechanics following total knee arthroplasty remains largely unknown. This study aimed to assess this question using the prognostic nutritional index to evaluate the nutritional status of orthopedic participants.
-
Methods Patients with knee osteoarthritis who underwent total knee arthroplasty (n=49) in Japan were divided into two groups based on their 1-week postoperative prognostic nutritional index. Group L patients had a prognostic nutritional index <40, whereas Group H comprised patients with a prognostic nutritional index ≥40. Postoperative improvements in Knee Injury and Osteoarthritis Outcome Score were evaluated. The patients performed squats under single-fluoroscopic surveillance in the sagittal plane for biomechanical evaluation. A two-dimensional/three-dimensional registration technique was employed to measure the tibiofemoral kinematics. The axial rotation of the femoral component relative to the tibial component and the anteroposterior translation of the medial and lateral femorotibial contact points were measured.
-
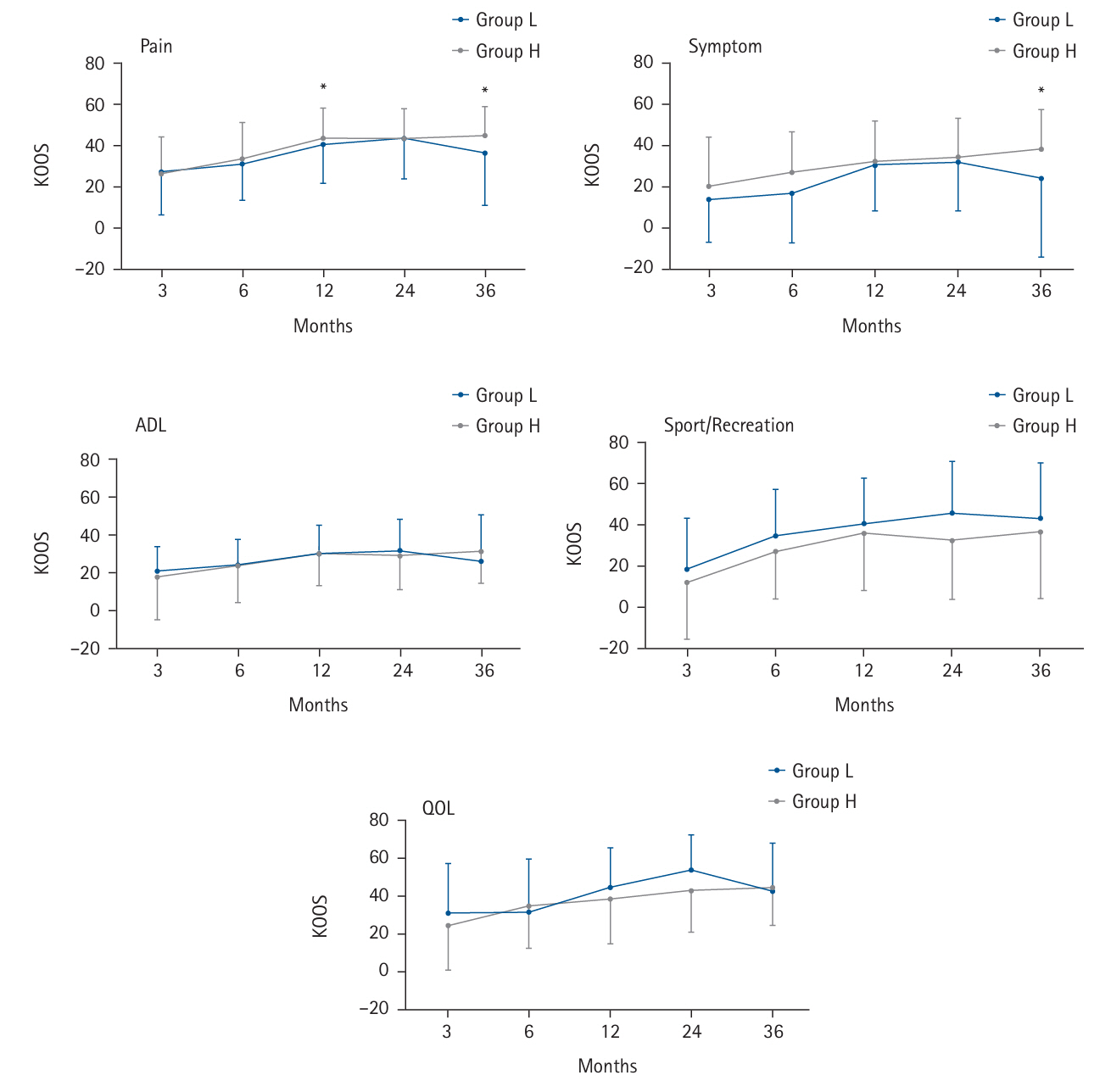
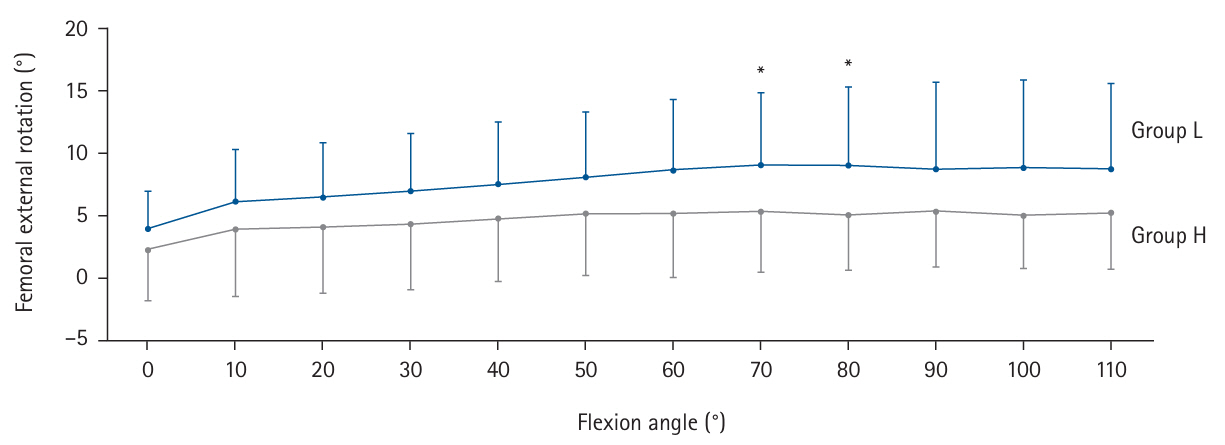
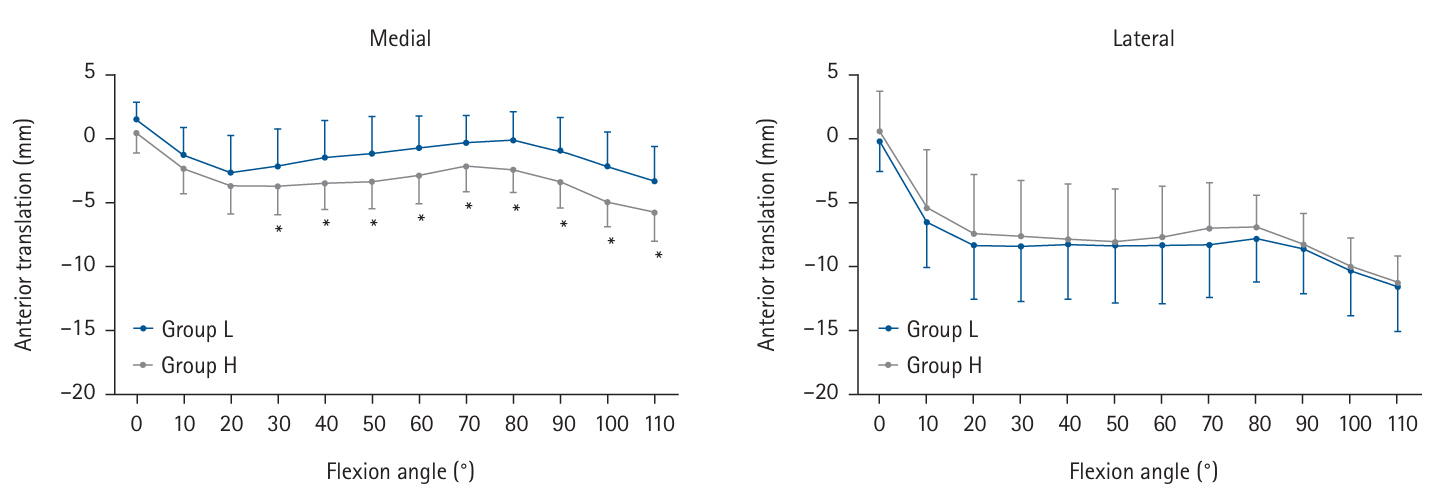
Results Group H showed significantly higher pain scores than Group L at 12 and 36 months postoperatively and a significantly higher symptom score at 36 months postoperatively. The kinematic comparison revealed that the axial external rotation in Group L was larger than that in Group H from 70° to 80° with flexion. Moreover, in the medial anteroposterior translation, Group L was more anteriorly located than Group H, with flexion beyond 30°.
-
Conclusion The results suggest that a high postoperative nutritional status significantly improved pain and other symptoms and was associated with better knee biomechanics following total knee arthroplasty.
Graphical abstract
Introduction
Methods
Results
Discussion
Authors’ contribution
Conceptualization: KK. Methodology: TT, TY, MT, Shuji Taketomi, RI, YT, Sakae Tanaka, KF. Formal analysis/validation: KK, RY. Project administration: KK. Funding acquisition: Not applicable. Writing – original draft: KK. Writing – review & editing: all authors. All authors read and approved the final manuscript.
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Funding
None.
Data availability
Research data are available from the corresponding author upon reasonable request.
Acknowledgments
We thank Dr. Yuhei Saito and Dr. Hiroshi Okawa, Surgical Center, The University of Tokyo Hospital, Tokyo, Japan; Shoji Konda, Department of Health and Sport Sciences, Osaka University Graduate School of Medicine, Osaka, Japan; Teruya Ishibashi, Department of Orthopaedic Biomaterial Science, Osaka University Graduate School of Medicine, Osaka, Japan; and Tomofumi Kage and Takahiro Arakawa, Department of Orthopaedic Surgery, Faculty of Medicine The University of Tokyo, Tokyo, Japan for providing advice on the kinematic data.
Supplementary materials
- 1. Kim HK, Suzuki T, Saito K, Yoshida H, Kobayashi H, Kato H, et al. Effects of exercise and amino acid supplementation on body composition and physical function in community-dwelling elderly Japanese sarcopenic women: a randomized controlled trial. J Am Geriatr Soc 2012;60:16-23. ArticlePubMed
- 2. Papadopoulou SK, Papadimitriou K, Voulgaridou G, Georgaki E, Tsotidou E, Zantidou O, et al. Exercise and nutrition impact on osteoporosis and sarcopenia: the incidence of osteosarcopenia: a narrative review. Nutrients 2021;13:4499.ArticlePubMedPMC
- 3. Christensen JC, Mizner RL, Foreman KB, Marcus RL, Pelt CE, LaStayo PC. Quadriceps weakness preferentially predicts detrimental gait compensations among common impairments after total knee arthroplasty. J Orthop Res 2018;36:2355-63. ArticlePubMedPDF
- 4. Greene KA, Schurman JR. Quadriceps muscle function in primary total knee arthroplasty. J Arthroplasty 2008;23(7 Suppl):15-9. Article
- 5. Van Onsem S, Verstraete M, Van Eenoo W, Van Der Straeten C, Victor J. Are TKA kinematics during closed kinetic chain exercises associated with patient-reported outcomes? A preliminary analysis. Clin Orthop Relat Res 2020;478:255-63. ArticlePubMedPMC
- 6. Kono K, Inui H, Tomita T, Yamazaki T, Taketomi S, Yamagami R, et al. The higher patient-reported outcome measure group had smaller external rotation of the femur in bicruciate-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2022;30:1292-9. ArticlePubMedPDF
- 7. Banks SA, Catani F, Deckard ER, Mahoney OM, Matsuda S, Meneghini RM, et al. Total knee arthroplasty kinematics predict patient-reported outcome measures: implications for clinical kinematic examinations. J Arthroplasty 2024;39(8S1):S224-9. Article
- 8. Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 1984;85:1001-5. PubMed
- 9. Cederholm T, Jensen GL, Correia MI, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. Clin Nutr 2019;38:1-9. ArticlePubMed
- 10. Cederholm T, Jensen GL, Correia MI, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle 2019;10:207-17. ArticlePubMedPMCPDF
- 11. Jensen GL, Cederholm T, Correia MI, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: a consensus report from the global clinical nutrition community. JPEN J Parenter Enteral Nutr 2019;43:32-40. ArticlePubMed
- 12. Tanemura A, Mizuno S, Hayasaki A, Gyoten K, Fujii T, Iizawa Y, et al. Onodera's prognostic nutritional index is a strong prognostic indicator for patients with hepatocellular carcinoma after initial hepatectomy, especially patients with preserved liver function. BMC Surg 2020;20:261.ArticlePubMedPMCPDF
- 13. Ren W, Wang H, Xiang T, Liu G. Prognostic role of preoperative Onodera's Prognostic Nutritional Index (OPNI) in gastrointestinal stromal tumors: a systematic review and meta-analysis. J Gastrointest Cancer 2023;54:731-8. ArticlePubMedPDF
- 14. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol 2005;91:181-4. ArticlePubMed
- 15. Inui H, Taketomi S, Nakamura K, Sanada T, Tanaka S, Nakagawa T. An additional reference axis improves femoral rotation alignment in image-free computer navigation assisted total knee arthroplasty. J Arthroplasty 2013;28:766-71. ArticlePubMed
- 16. Kawaguchi K, Inui H, Yamagami R, Kenichi K, Sameshima S, Kage T, et al. A new technique for determining the rotational alignment of the tibial component during total knee arthroplasty. Knee 2021;29:323-31. ArticlePubMed
- 17. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003;1:64.ArticlePubMedPMC
- 18. Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Yoshikawa H, et al. Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans Med Imaging 2004;23:602-12. ArticlePubMed
- 19. Yamazaki T, Watanabe T, Nakajima Y, Sugamoto K, Tomita T, Maeda D, et al. Visualization of femorotibial contact in total knee arthroplasty using X-ray fluoroscopy. Eur J Radiol 2005;53:84-9. ArticlePubMed
- 20. Shimizu N, Tomita T, Yamazaki T, Yoshikawa H, Sugamoto K. The effect of weight-bearing condition on kinematics of a high-flexion, posterior-stabilized knee prosthesis. J Arthroplasty 2011;26:1031-7. ArticlePubMed
- 21. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 1983;105:136-44. ArticlePubMedPDF
- 22. Kang H. Sample size determination for repeated measures design using G Power software. Anesth Pain Med 2015;10:6-15. Article
- 23. Tick H. Nutrition and pain. Phys Med Rehabil Clin N Am 2015;26:309-20. ArticlePubMed
- 24. Messina OD, Vidal Wilman M, Vidal Neira LF. Nutrition, osteoarthritis and cartilage metabolism. Aging Clin Exp Res 2019;31:807-13. ArticlePubMedPDF
- 25. Luyckx L, Luyckx T, Bellemans J, Victor J. Iliotibial band traction syndrome in guided motion TKA: a new clinical entity after TKA. Acta Orthop Belg 2010;76:507-12. PubMed
- 26. Yoshida T, Ebiko J, Sasaki K, Uchiyama E, Kura H. Recovery process of the muscle activities during walking with efficient early quadriceps training and gait exercises after total knee arthroplasty. J Bodyw Mov Ther 2022;29:49-53. ArticlePubMed
- 27. Armstrong R, Baltzopoulos V, Langan-Evans C, Clark D, Jarvis J, Stewart C, et al. An investigation of movement dynamics and muscle activity during traditional and accentuated-eccentric squatting. PLoS One 2022;17:e0276096.ArticlePubMedPMC
- 28. Kvarda P, Nuesch C, Egloff C, Appenzeller-Herzog C, Mundermann A, Ismailidis P. Hip abductor muscle strength in patients after total or unicompartmental knee arthroplasty for knee osteoarthritis or avascular necrosis: a systematic review and meta-analysis protocol. BMJ Open 2020;10:e038770.ArticlePubMedPMC
- 29. Arnout N, Victor J, Chevalier A, Bellemans J, Verstraete MA. Muscle loaded stability reflects ligament-based stability in TKA: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 2022;30:612-20. ArticlePubMedPDF
- 30. Kao DD, Ferrandino RM, Roof SA, Marshall DC, Khan MN, Chai RL, et al. Neutrophil-to-lymphocyte ratio as a predictor of surgical outcomes in head and neck cancer. Head Neck 2023;45:1903-12. ArticlePubMedPMC
- 31. Perry LA, Liu Z, Loth J, Penny-Dimri JC, Plummer M, Segal R, et al. Perioperative neutrophil-lymphocyte ratio predicts mortality after cardiac surgery: systematic review and meta-analysis. J Cardiothorac Vasc Anesth 2022;36:1296-303. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

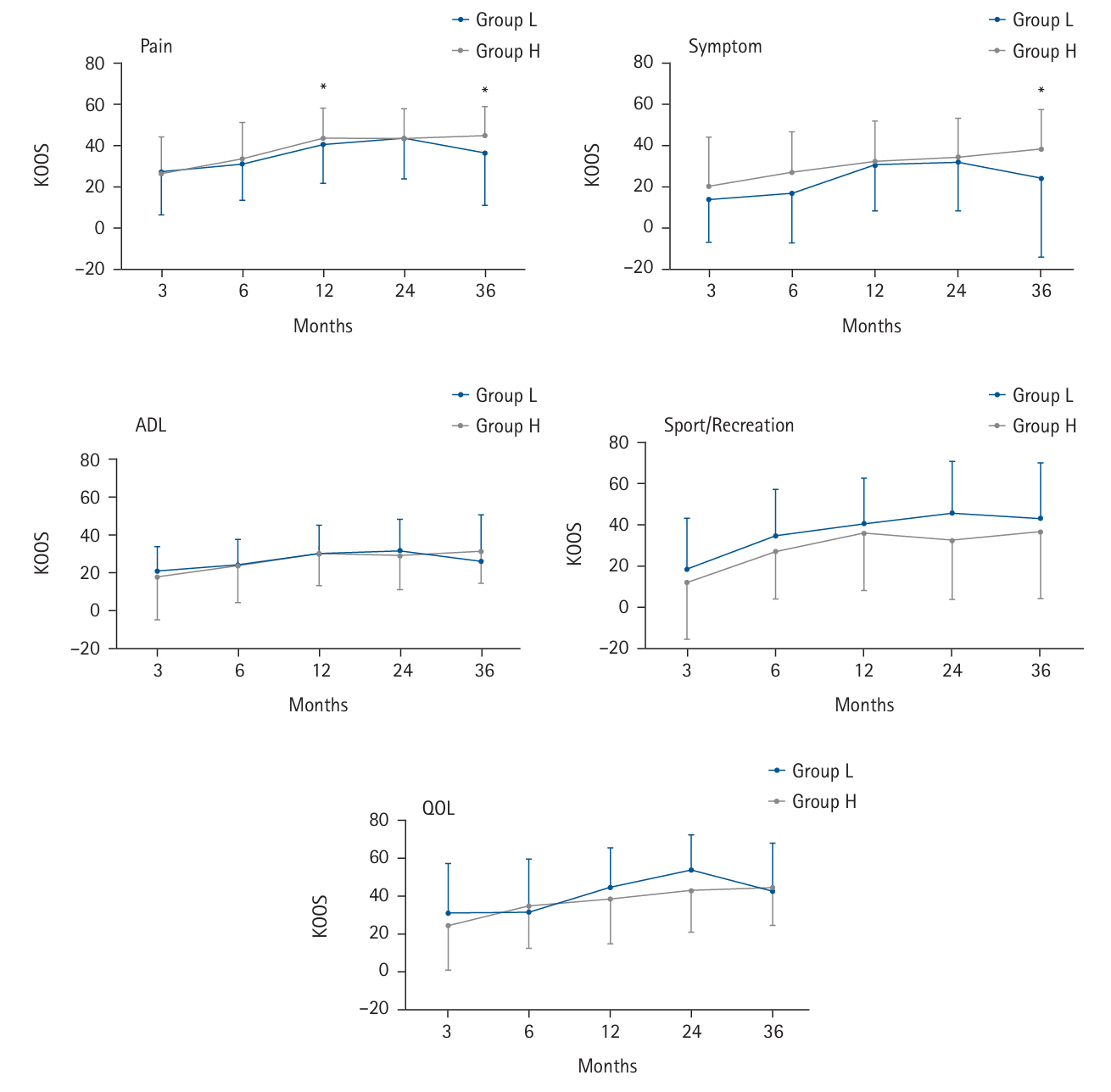
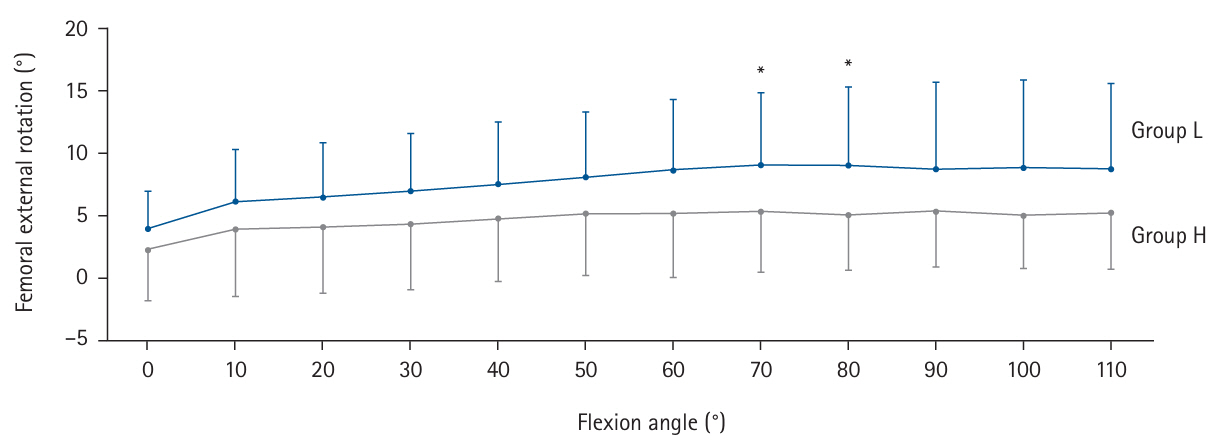
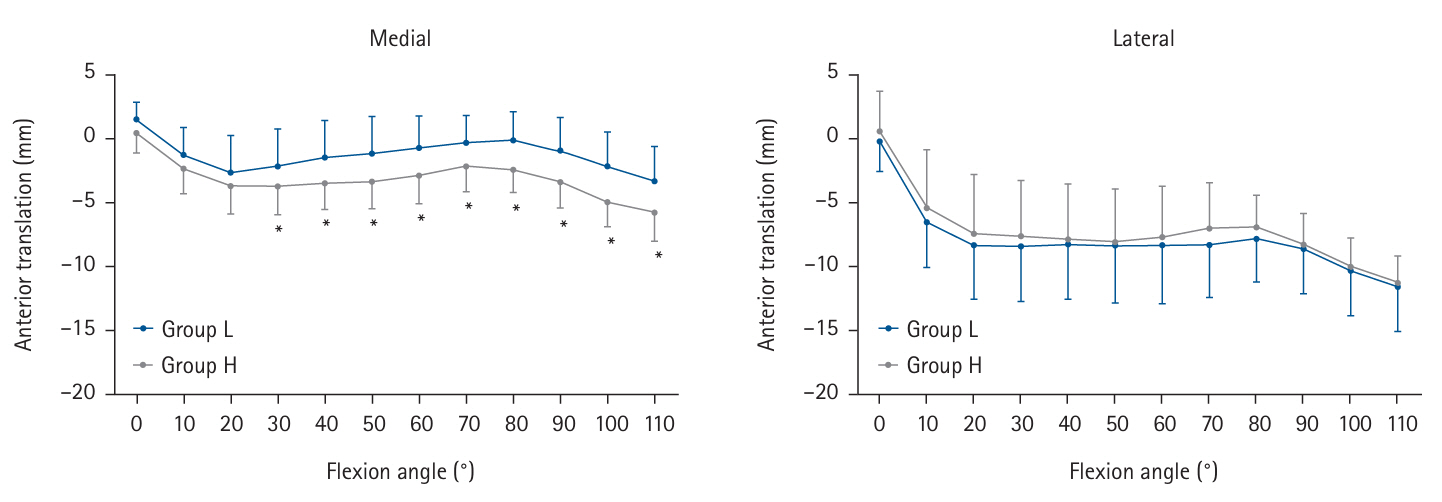
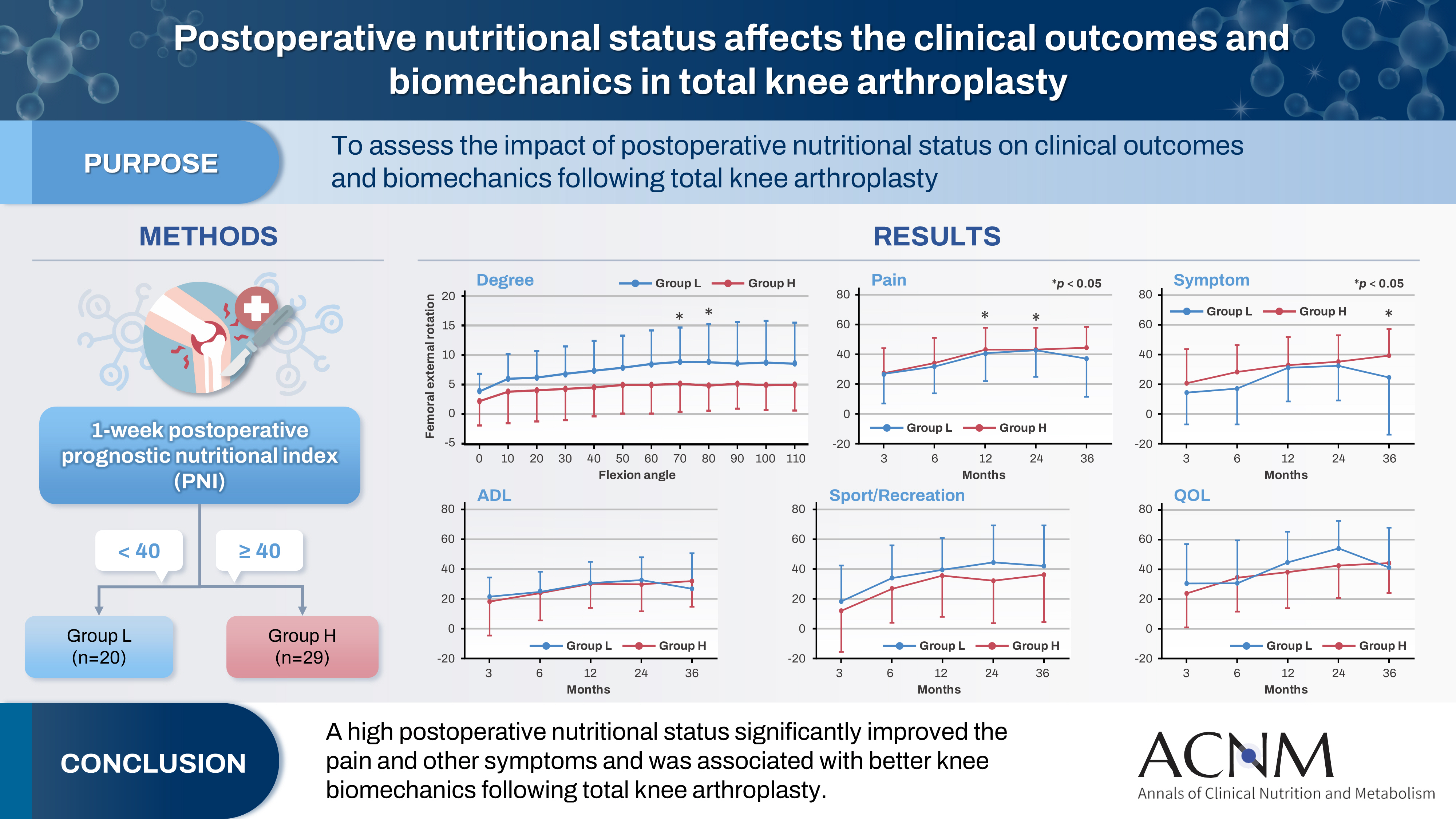
Fig. 1.
Fig. 2.
Fig. 3.
Fig. 4.
Graphical abstract
| Detailed information |
|---|
| The KOOS uses data on five knee-specific patient-centered outcomes: |
| (1) Pain |
| (2) Other symptoms such as swelling, restricted range of motion, and mechanical symptoms |
| (3) Disability at the level of activities of daily living (ADL) |
| (4) Disability at a level physically more demanding than ADL |
| (5) Mental and social aspects such as awareness and lifestyle changes |
| The KOOS is self-administered and filled out by the patient: |
| (1) The five patient-relevant subscales of KOOS are scored separately: Pain (9 items); Symptoms (7 items); ADL (17 items); Sport and Recreation (5 items); Quality of Life (4 items). |
| (2) A Likert scale is used, and all items have five possible answers scored from 0 (no problems) to 4 (extreme problems); each of the five scores is calculated as the sum of the items included. Scores are transformed to a 0–100 scale, with zero representing extreme knee problems and 100 representing no knee problems. |
| Variable | Group L (n=20) | Group H (n=29) | P-value |
|---|---|---|---|
| Age (yr) | 76.6±6.2 | 74.6±6.4 | 0.27 |
| Body mass index (kg/m2) | 26.7±3.4 | 26.7±4.3 | 0.81 |
| Fluoroscopic follow-up time (mo) | 15.0±7.8 | 12.4±7.5 | 0.06 |
| Sex (female:male) | 16:4 | 25:4 | 0.71 |
| WBC (/μL) | 6,830±1,661 | 6,424±1,367 | 0.42 |
| CRP (mg/L) | 5.7±3.2 | 3.8±3.7 | 0.01 |
| NLR | 4.3±2.1 | 2.7±1.1 | <0.01 |
Values are presented as mean ±standard deviation. Group L had a prognostic nutritional index (PNI) <40, while Group H had a PNI ≥40. WBC, white blood cell count; CRP, C-reactive protein; NLR, neutrophil-to-lymphocyte ratio.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 Cite
Cite

