Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > J Clin Nutr > Volume 9(2); 2017 > Article
- Case Report Case Report of an Adult Patient Who Underwent a Serial Transverse Enteroplasty Procedure for Short Bowel Syndrome Following an Esophagectomy and Total Gastrectomy
- Sang-Yong Son, Long-Hai Cui, Ho-Jung Shin, Hoon Hur, Sang-Uk Han
- 식도 및 위절제 시행했던 환자에서 대량 소장절제로 발생한 단장증후군 환자에서 STEP 시행 증례 보고
- 손상용, 최룡해, 신호정, 허훈, 한상욱
-
Journal of the Korean Society for Parenteral and Enteral Nutrition 2017;9(2):68-73.
DOI: https://doi.org/10.15747/jcn.2017.9.2.68
Published online: December 31, 2017
Department of Surgery, Ajou University School of Medicine, Suwon, Korea
- Correspondence to Sang-Yong Son Department of Surgery, Ajou University School of Medicine, 164 WorldCup-ro, Yeongtong-gu, Suwon 16499, Korea Tel: +82-31-219-5200, Fax: +82-31-219-5755, E-mail: spy798@gmail.com
This case report was presented as one of the oral presentations at KSSMN 2017.
• Received: June 21, 2017 • Revised: December 10, 2017 • Accepted: December 13, 2017
Copyright: © Korean Society for Parenteral and Enteral Nutrition
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,121 Views
- 2 Download
Abstract
- Since its introduction as an alternative intestinal lengthening technique, the serial transverse enteroplasty (STEP) procedure has been used increasingly as the surgical treatment of choice for children with short bowel syndrome (SBS). On the other hand, there are few report of its efficacy in adults with SBS, particularly those who have previously undergone a gastrectomy. This case report describes a 34-year-old woman with a short bowel after an esophagectomy and total gastrectomy due to lye ingestion followed by an extensive intestinal resection due to small bowel strangulation. The STEP procedure was performed successfully and the small intestine was lengthened from 55 to 75 cm. The patient tolerated the procedure well and was weaned off total parenteral nutrition. The frequency and characteristics of diarrhea improved, and her weight remained acceptable via management with intermittent parenteral nutritional support for 6 months postoperatively. This case suggests that the STEP procedure should be considered for gastrectomized patients with SBS.
INTRODUCTION
Short bowel syndrome (SBS) is a disorder characterized by significant malnutrition and malabsorption requiring prolonged parenteral nutrition to prevent dehydration and to replace electrolytes, vitamins, and trace elements, regardless of the remaining bowel length.1 Although there have been considerable improvements in a multidisciplinary approach and intestinal transplantation to treat SBS over the past two decades, other medical and surgical alternatives remain the main treatment options. The most common surgical alternatives are intestinal lengthening procedures such as the Bianchi procedure and the serial transverse enteroplasty (STEP) procedure.2,3 Both methods increase the length of the small bowel and prolong the duration of intestinal transit, which may allow patients with SBS to depend less on total parenteral nutrition (TPN).
The STEP procedure is relatively new and technically easier to perform than the Bianchi procedure. It has become the surgical treatment of choice for children with SBS and has better outcomes, specifically, a higher incidence of TPN weaning and a lower risk of intestinal transplantation salvage, than the Bianchi procedure.4 However, there are few reports of its efficacy in adults with SBS, especially those who have previously undergone gastrectomy. Herein, we present our experience of the STEP procedure and its nutritional outcomes in an adult patient with SBS who had previously undergone esophagectomy and total gastrectomy followed by extensive intestinal resection.
CASE REPORT
A 34-year-old woman was admitted to the emergency room due to the abrupt onset of abdominal pain. The patient was on medication for a mood disorder and had a surgical history of esophagectomy, total gastrectomy, and right hemi-colonic interposition between the esophagus and duodenum due to lye ingestion. A computed tomography (CT) scan showed mesenteric rotation of the small intestine with strangulation. An emergency operation was conducted in which massive resection of the small intestine was performed. The proximal portion of the jejunum and about 5 cm of the terminal ileum were saved, and a hand-sewn end-to-end anastomosis was performed. The patient recovered without any major complications and was discharged on the 14th day postoperatively. However, she complained of poor oral intake and postprandial abdominal pain with distension at the 4th week postoperatively. A CT scan and colonoscopy revealed stenosis of the terminal ileum and thus a covered stent was inserted. Unfortunately, it migrated 2 weeks later and another covered stent was inserted; however, it could be maintained about 1 week due to severe abdominal pain in the surrounding area. After 6 weeks, a bare stent was successfully inserted and oral intake slightly improved for a while. However, the patient again complained of severe abdominal pain after 3 weeks. A colonoscopy revealed the bare stent had caused a severe ulcer and it was therefore removed. To resolve stenosis of the terminal ileum and malnutrition, an elective operation for neo-jejunocolostomy and the STEP procedure was planned. The patient received TPN for 6 weeks prior to the operation.
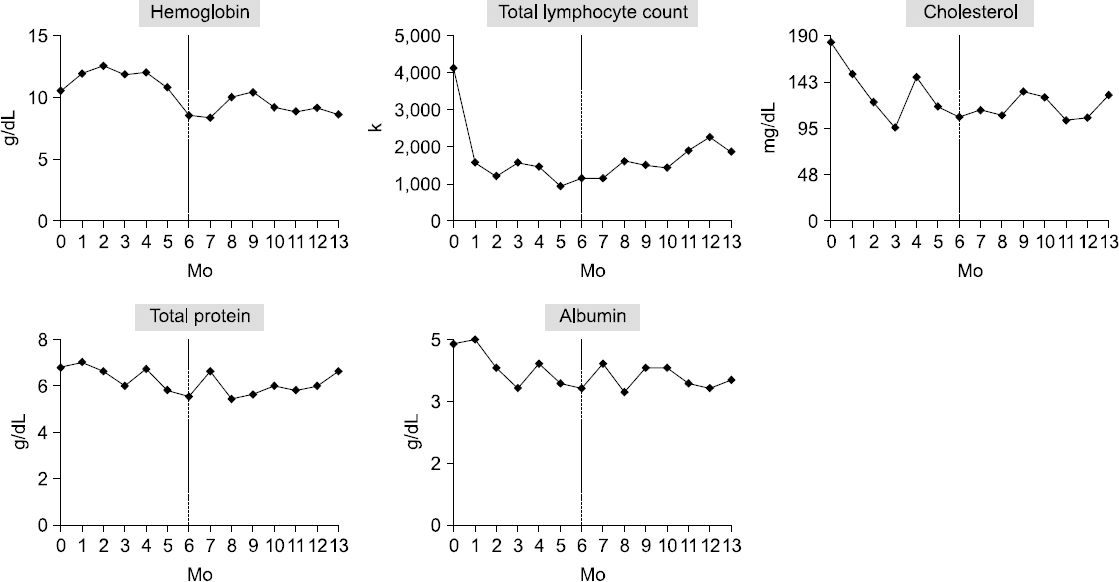
After adhesiolysis of the entire small intestine, side-to-side neo-jejunocolostomy was performed using a linear stapler in the portion proximal to the previous anastomotic site. The length of the remnant small intestine was measured with a ruler. The center of the antimesenteric side was marked with a colored marker, and then serial alternating and opposite sites for the STEP procedure were marked at a distance of 3 cm from each other (not 2 cm such as in pediatric patients because of the possibility of intestinal obstruction) (Fig. 1). Thereafter, the linear stapler (TLC75; Ethicon EndoSurgery Inc., Cincinnati, OH, USA) was applied perpendicularly and introduced to the opposite side, ensuring that the final portion was only stapled, not cut. No reinforcement suture was added on the stapled lines.
Fig. 1
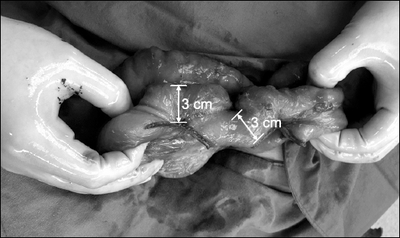
Appearance of the small intestine after the serial transverse enteroplasty procedure. Linear staplers were applied perpendicularly at a distance of 3 cm from each other. The total length of the small intestine between the Treitz ligament and the jejunocolonostomy was increased from 55 to 75 cm (an increase of 36%).
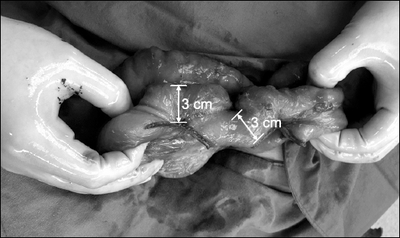
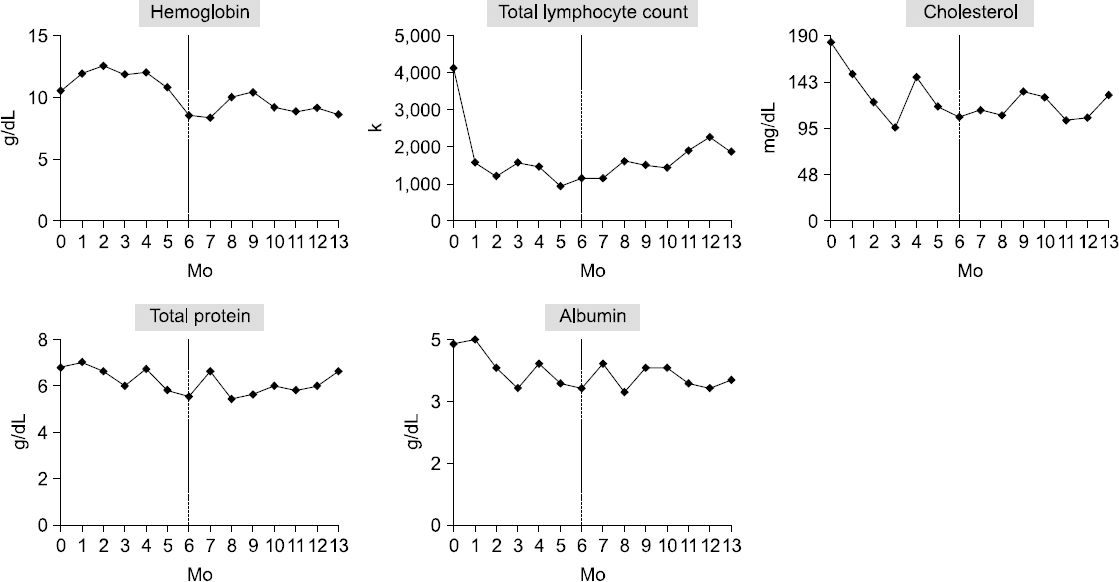
After firing the stapler 6∼7 times, a zigzag pattern was created and the length of the small intestine was measured. The STEP procedure lengthened the small intestine from 55 to 75 cm, an increase of 36%. A small bowel series at the 6th month postoperatively is shown in Fig. 2.
Fig. 2
A small bowel series at 6 months after the serial transverse enteroplasty procedure. There was no bowel dilatation or passage disturbance.
The sips of water were allowed on the second postoperative day. A semi-fluid diet was administered on the fifth postoperative day after flatus passage and a semi-blend diet on the seventh postoperative day. Food intake reached half of the normal intake after 2 weeks postoperatively (about 65% of the daily calorie requirement) and almost same as the normal intake after 3 weeks postoperatively (about 130% of the daily calorie requirement). TPN was maintained during the diet build up (about 100% of the daily calorie requirement), then it was reduced steadily after 3 weeks postoperatively. The patient was temporarily weaned off TPN after 4 weeks postoperatively and discharged at 36 days postoperatively without any complications or medical problems. At the time of discharge, the patient had to consume about two times the daily calorie requirement to maintain her weight.
Changes in body weight and diarrhea before and after the STEP procedure are shown in Fig. 3. At the time of the operation for a strangulated small intestine, the patient weighed 45 kg. Her weight drastically decreased during the first 4 months after intestinal resection due to the failed stent insertions and poor oral intake. After planning the STEP procedure, the patient was admitted to Ajou University Hospital and received TPN for about 6 weeks, and her body weight increased to 42 kg. After the STEP procedure, her body weight was maintained relatively well around 39 kg.
Fig. 3
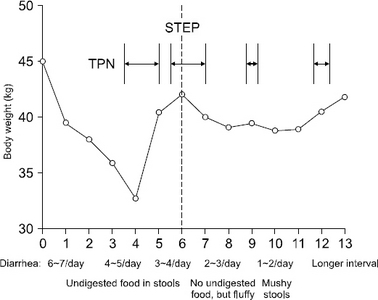
Changes in body weight and diarrhea before and after the serial transverse enteroplasty (STEP) procedure. Body weight decreased drastically during the first 4 months after intestinal resection due to failed stent insertions and poor oral intake. After the STEP procedure, body weight was well maintained and the characteristics of diarrhea improved. Total parenteral nutrition (TPN) was delivered via hospital admission in collaboration with a nutrition specialist.
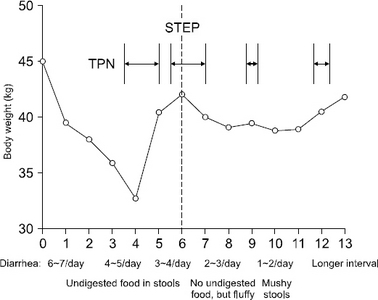
The STEP procedure remarkably improved the frequency and characteristics of diarrhea. Before the STEP procedure, the patient complained of frequent watery diarrhea (at least 3∼4 times per day) with undigested food in her stools. After the STEP procedure, the frequency of diarrhea decreased to 1∼2 times per day, and stools gradually became fluffy or mushy.
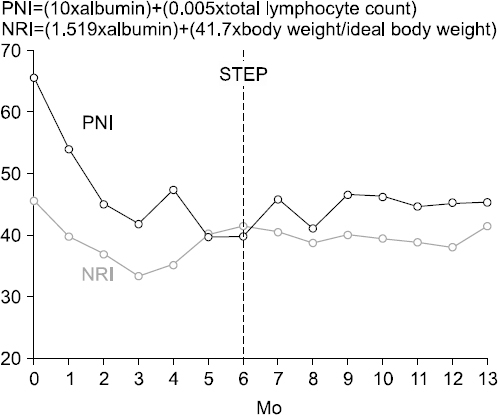
The prognostic nutritional index (PNI) has been used to assess immunological and nutritional conditions, and the nutritional risk index (NRI) has been widely used as a malnutrition screening tool. To assess the nutritional status of the patient, the PNI and NRI were evaluated (Fig. 4). These indices decreased sharply over the 3 months after intestinal resection, but stabilized after the STEP procedure. Notably, the PNI decreased to almost 40 before the STEP procedure, but remained higher than 45 afterwards.
Fig. 4
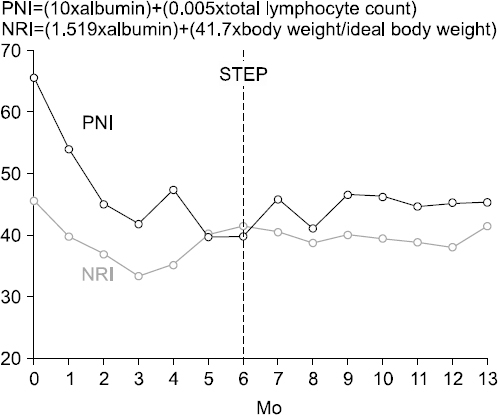
Changes in nutritional indices. The prognostic nutritional index (PNI) and nutritional risk index (NRI) were evaluated to assess the nutritional status of the patient before and after the serial transverse enteroplasty (STEP) procedure. These indices decreased sharply during the 3 months after intestinal resection, but stabilized after the STEP procedure.
Biochemical analysis of hemoglobin, the total lymphocyte count, serum cholesterol, serum total protein, and albumin was reviewed retrospectively to assess the patient’s nutritional status (Fig. 5). The hemoglobin level showed a slightly decreasing trend even after the STEP procedure due to pernicious anemia, despite blood transfusion and hematologic management. The total lymphocyte count decreased sharply after the massive bowel resection, but recovered slightly over time after the STEP procedure. However, the other biochemical data showed no definite trend of changes before and after STEP procedure.
Fig. 5
Biochemical changes before and after the serial transverse enteroplasty (STEP) procedure. The hemoglobin level showed a slightly decreasing trend even after the STEP procedure due to pernicious anemia. The total lymphocyte count recovered slightly over time after the STEP procedure.
To follow-up the changes in body composition of the patient, multi-frequency bioelectric impedance analysis was performed using an InBody S10 analyzer (Biospace, Seoul, Korea) every 2 months after the STEP procedure (Table 1). Skeletal muscle mass and protein and mineral levels were well maintained, and basal metabolic rates were therefore stable at about 1,100 kcal. However, the percentage of body fat and the visceral fat area decreased until the 3rd month postoperatively and increased to the preoperative level at the 7th month postoperatively. The phase angle, which is a measure of reactance and resistance determined via bioelectrical impedance analysis, showed a decreasing trend for all extremities compared with the preoperative values.
Table 1
Multi-frequency bioelectric impedance analysis of changes in body composition
DISCUSSION
Patients with SBS are commonly categorized into three subtypes according to the extent of the resection and the remnant bowel: jejunoileal anastomosis, jejunocolic anastomosis, and jejunostomy.5 Each type is associated with a different range and severity of symptoms due to the altered anatomy and associated pathophysiology. In general, the ileum has a greater adaptive potential than the jejunum; therefore, patients with jejunoileal anastomoses rarely exhibit major nutrient or electrolyte imbalances and often maintain proper hydration. By contrast, ileal resection, such as jejunocolic anastomosis, typically results in more severe disease than jejunoileal anastomosis. Patients whose remnant intestine is shorter than 60∼65 cm have the greatest risk of parenteral nutrition dependence, are likely to experience diarrhea due to decreased water reabsorption, and their diarrhea is often further exacerbated following partial resection of the colon. In a recent matched-case control study, patients in the ileum predominated group had lower Bristol stool scale scores than those in the jejunum predominated group, and presence of the ileum was an independent factor associated with parenteral nutrition weaning in multivariate analysis.6 Thus, not only the length of the remnant bowel but also the subtype of SBS should be considered when planning the long-term nutritional support strategy in patients with SBS.
The initial strategy for SBS is to maximize enteral tolerance through feeding and gut adaptation. However, alternative surgical treatment is often required when patients show no further progression with enteral tolerance, a persistent need for parenteral nutrition, dilated small bowel loops via imaging, and symptoms of bacterial overgrowth that do not respond to antibiotics.7 Two intestinal lengthening procedures are commonly preferred prior to the consideration of intestinal transplantation: the Bianchi procedure and the STEP procedure.
The STEP procedure was introduced in 2003 and is becoming a standard procedure for SBS because it is technically easier to perform than the Bianchi procedure. A great deal of experience is required to identify appropriate candidates for the latter procedure. The STEP procedure involves simple, consecutive, incomplete bowel resections using linear staplers by alternating from the mesenteric to the antimesenteric edge or side-to-side as the modified method.3 It remains controversial over which method is superior, but a few recent studies favor the STEP procedure. A systematic review (seven case series involving 86 children) reported that 87% of children who underwent the STEP procedure had improved enteral tolerance, and the mean percentage tolerance increased from 35.1% to 69.5%.8 The international STEP data registry revealed that the overall survival rate of patients following the STEP procedure was 89%, with 47% of patients attaining enteral autonomy.9 However, these results might be influenced by selection bias. Thus, definitive evidence for the superiority of the STEP method over the Bianchi method, or vice versa, is still lacking.
Recently, efforts were made to improve the outcome of the STEP procedure in patients with SBS by restoring ileocecal valve function for intestinal adaptation.10 A Brooke-type neovalve was created by anastomosing the jejunum to the cecum in two patients who underwent the STEP procedure for SBS. After 1 year, they had a stable nutritional status, with a weight gain of 14∼16 kg. However, this technical challenge has been reported in a few case reports; therefore, its efficacy in lengthening procedures should be further evaluated in the future.
The jejunum was extremely short in the patient presented here with partially resected colon because she had undergone esophagectomy, total gastrectomy, and right hemi-colonic interposition between the esophagus and duodenum before massive resection of the small bowel. Although the STEP procedure was planned in combination with neo-jejunocolostomy due to anastomotic stenosis, it was successfully performed without leakage or intestinal obstruction and lengthened the remnant intestine from 55 to 75 cm. Diarrhea and body weight remarkably improved after the STEP procedure, and laboratory findings, nutrition assessment indices, and bioelectric impedance analysis also indicated that the nutritional status of the patient was stable in short-term follow-up. However, the observation period was relatively short (7 months after the STEP procedure); thus studies including similar cases with a longer follow-up are required to objectively assess the success of this method in gastrectomized patients with SBS.
In conclusion, the surgical strategy for patients with SBS should be chosen with consideration of the length of the remnant small bowel, its subtype, and responsiveness to the multidisciplinary medical approach. The STEP procedure is an easy and effective method to safely lengthen the remnant bowel and increase the small intestinal transit duration, even in adult patients with SBS.
- 1. Höllwarth ME. Surgical strategies in short bowel syndrome. Pediatr Surg Int 2017;33(4):413-9. ArticlePubMedPDF
- 2. Bianchi A. Intestinal loop lengthening--a technique for increasing small intestinal length. J Pediatr Surg 1980;15(2):145-51. ArticlePubMed
- 3. Kim HB, Lee PW, Garza J, Duggan C, Fauza D, Jaksic T. Serial transverse enteroplasty for short bowel syndrome: a case report. J Pediatr Surg 2003;38(6):881-5. ArticlePubMed
- 4. Sudan D, Thompson J, Botha J, Grant W, Antonson D, Raynor S, et al. Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg 2007;246(4):593-601. ArticlePubMed
- 5. Tappenden KA. Pathophysiology of short bowel syndrome: considerations of resected and residual anatomy. JPEN J Parenter Enteral Nutr 2014;38(1 Suppl):14S-22S. ArticlePubMed
- 6. Kong W, Wang J, Ying R, Li Y, Jin H, Mao Q, et al. A potential anatomic subtype of short bowel syndrome: a matched case-control study. BMC Gastroenterol 2016;16:12.ArticlePubMedPMC
- 7. Yannam GR, Sudan DL, Grant W, Botha J, Langnas A, Thompson JS. Intestinal lengthening in adult patients with short bowel syndrome. J Gastrointest Surg 2010;14(12):1931-6. ArticlePubMedPDF
- 8. Fernandes MA, Usatin D, Allen IE, Rhee S, Vu L. Improved enteral tolerance following step procedure: systematic literature review and meta-analysis. Pediatr Surg Int 2016;32(10):921-6. ArticlePubMedPDF
- 9. Jones BA, Hull MA, Potanos KM, Zurakowski D, Fitzgibbons SC, Ching YA, et al. Report of 111 consecutive patients enrolled in the International Serial Transverse Enteroplasty (STEP) Data Registry: a retrospective observational study. J Am Coll Surg 2013;216(3):438-46. ArticlePubMedPMC
- 10. Botey M, Alastrué A, Haetta H, Fernández-Llamazares J, Clavell A, Moreno P. Long-term results of serial transverse enteroplasty with neovalve creation for extreme short bowel syndrome: report of two cases. Case Rep Gastroenterol 2017;11(1):229-40. ArticlePubMedPMCPDF
References
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

Case Report of an Adult Patient Who Underwent a Serial Transverse Enteroplasty Procedure for Short Bowel Syndrome Following an Esophagectomy and Total Gastrectomy
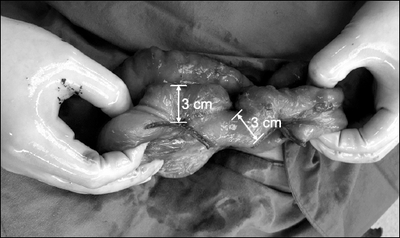
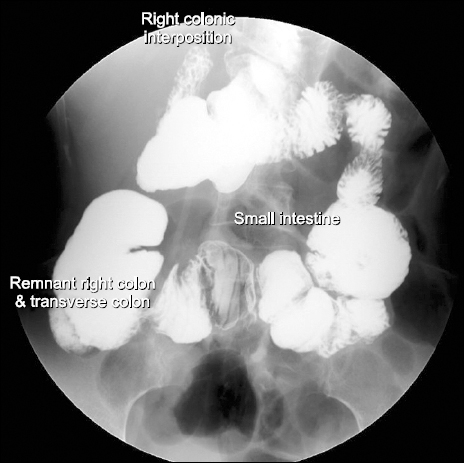
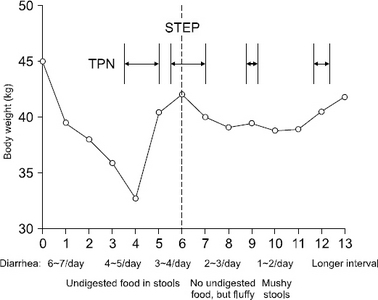
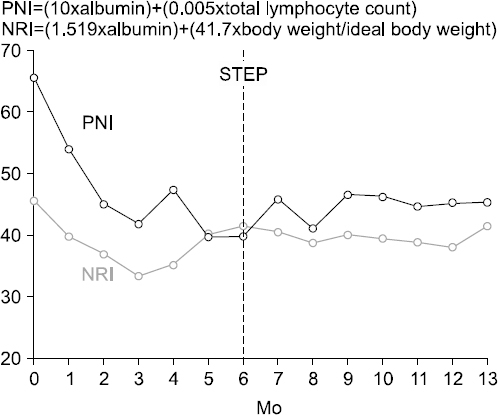
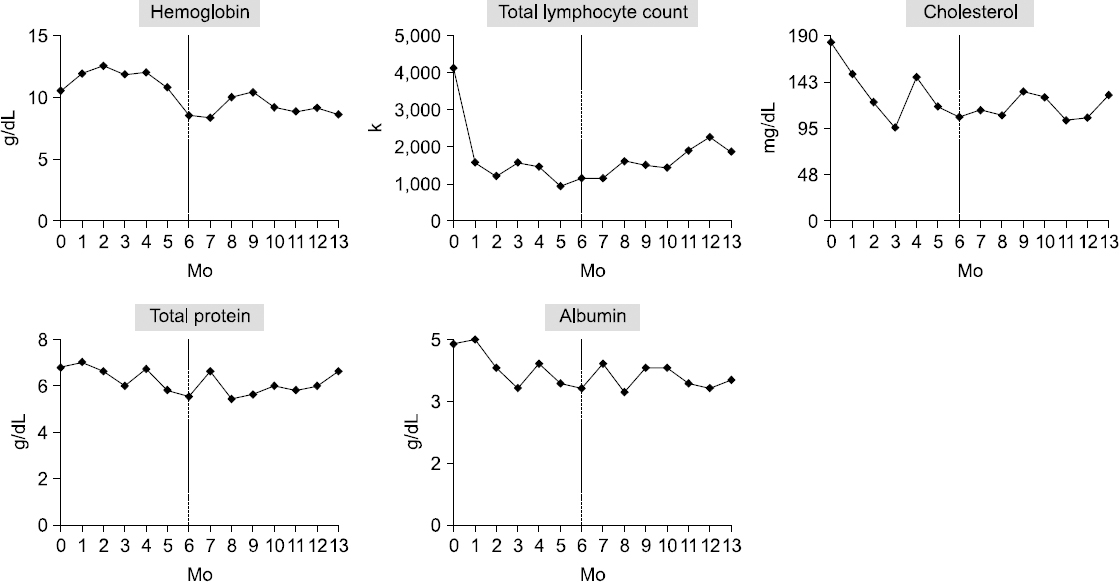
Fig. 1
Appearance of the small intestine after the serial transverse enteroplasty procedure. Linear staplers were applied perpendicularly at a distance of 3 cm from each other. The total length of the small intestine between the Treitz ligament and the jejunocolonostomy was increased from 55 to 75 cm (an increase of 36%).
Fig. 2
A small bowel series at 6 months after the serial transverse enteroplasty procedure. There was no bowel dilatation or passage disturbance.
Fig. 3
Changes in body weight and diarrhea before and after the serial transverse enteroplasty (STEP) procedure. Body weight decreased drastically during the first 4 months after intestinal resection due to failed stent insertions and poor oral intake. After the STEP procedure, body weight was well maintained and the characteristics of diarrhea improved. Total parenteral nutrition (TPN) was delivered via hospital admission in collaboration with a nutrition specialist.
Fig. 4
Changes in nutritional indices. The prognostic nutritional index (PNI) and nutritional risk index (NRI) were evaluated to assess the nutritional status of the patient before and after the serial transverse enteroplasty (STEP) procedure. These indices decreased sharply during the 3 months after intestinal resection, but stabilized after the STEP procedure.
Fig. 5
Biochemical changes before and after the serial transverse enteroplasty (STEP) procedure. The hemoglobin level showed a slightly decreasing trend even after the STEP procedure due to pernicious anemia. The total lymphocyte count recovered slightly over time after the STEP procedure.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Case Report of an Adult Patient Who Underwent a Serial Transverse Enteroplasty Procedure for Short Bowel Syndrome Following an Esophagectomy and Total Gastrectomy
Multi-frequency bioelectric impedance analysis of changes in body composition
| Variable | Preoperative | 1 month postoperative | 3 months postoperative | 5 months postoperative | 7 months postoperative |
|---|---|---|---|---|---|
| Body weight (kg) | 40.4 | 40.1 | 38.2 | 38.1 | 41.8 |
| Skeletal muscle mass (kg) | 17.4 | 17.7 | 17.6 | 16.6 | 18.5 |
| Protein (kg) | 6.4 | 6.5 | 6.5 | 6.1 | 6.8 |
| Mineral (kg) | 2.5 | 2.5 | 2.5 | 2.4 | 2.7 |
| Percentage of body fat (%) | 15.7 | 15.1 | 10.5 | 13.9 | 13.2 |
| Visceral fat area (cm2) | 39.2 | 34.9 | 28.9 | 39.3 | 40.5 |
| Basal metabolic rate (kcal) | 1,105 | 1,105 | 1,108 | 1,079 | 1,154 |
| TBW/FFM (%) | 73.7 | 73.4 | 73.6 | 74.0 | 73.8 |
| Phase angle at 50 kHz (ϕ) | |||||
| Trunk | 3.8 | 5 | 3.8 | 3.4 | 3 |
| Right arm | 4.2 | 4.4 | 3.4 | 3.5 | 3.3 |
| Left arm | 4.1 | 4.7 | 3.9 | 3.7 | 3.6 |
| Right lower extremity | 3.4 | 4.1 | 3.9 | 2.7 | 3 |
| Left lower extremity | 3.2 | 4.4 | 3.8 | 2.6 | 3 |
TBW = total body weight; FFM = fat-free mass.
Table 1 Multi-frequency bioelectric impedance analysis of changes in body composition
TBW = total body weight; FFM = fat-free mass.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN Cite
Cite

