Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Surgical Metabolism and Nutrition > Volume 11(1); 2020 > Article
- Original Article Risk Factors for Unexpected Removal of Peripherally Inserted Central Catheters and Proper Duration of the Catheter Maintenance
- Narang Lee, M.D., Hyun-Dong Chae, M.D., In-Hwan Kim, M.D.
-
Surgical Metabolism and Nutrition 2020;11(1):27-33.
DOI: https://doi.org/10.18858/smn.2020.11.1.27
Published online: June 30, 2020
1Department of Surgery, Daegu Catholic University School of Medicine, Daegu, Korea
- Correspondence to: In-Hwan Kim, Department of Surgery, Daegu Catholic University School of Medicine, 33 Duryugongwon-ro 17-gil, Nam-gu, Daegu 42472, KoreaTel: +82-53-650-4429, Fax: +82-53-624-7185, E-mail: kih2yk@cu.ac.kr
Copyright © 2020 The Korean Society of Surgical Metabolism and Nutrition
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,653 Views
- 6 Download
Abstract
-
Purpose Despite the advantages of a peripherally inserted central catheter (PICC), many complications have led to the unexpected removal of catheters. On the other hand, there are no guidelines for the duration of PICC maintenance. This study analyzed the risk factors for the unexpected removal of PICC to suggest guidelines for the duration of catheter maintenance.
-
Materials and Methods Among 520 patients who underwent PICC insertion from January 2014 to December 2015, 407 were included. Unexpected removal was observed in 95 patients. Univariate and multivariate analyses were performed to evaluate the risk factors for unexpected removal. The changing pattern of the probability of unexpected removal was analyzed by change point analysis.
-
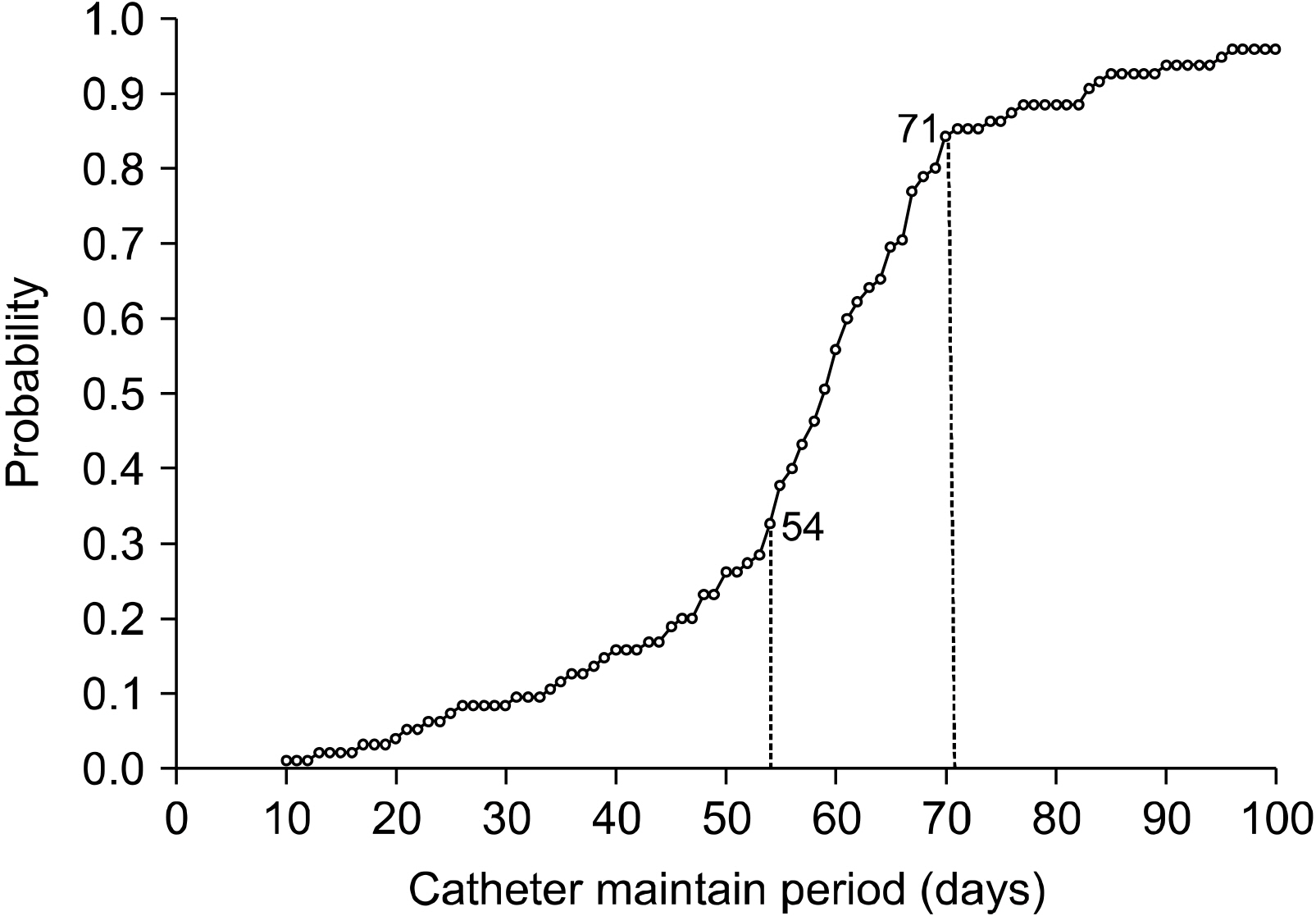
Results Malignancy (OR=4.498, 95% CI=2.49∼8.125) and ICU hospitalization (OR=4.218, 95% CI=1.694∼10.505) were significant risk factors for the unexpected removal of PICC. The left arm (OR=0.279, 95% CI=0.143∼0.544) and basilic vein (OR=0.323, 95% CI=0.192∼0.545) were associated with a lower probability of unexpected removal compared to the right arm and brachial vein, but selection bias could exist in the arm side and vein. Change-point analysis revealed a rapid increase in the probability of unexpected removal after 54 catheter days.
-
Conclusion This study suggests the removal or exchange of PICC before 54 catheter days to minimize serious complications. More attention is needed for patients with malignancies and ICU stays.
INTRODUCTION
MATERIALS AND METHODS
RESULTS
DISCUSSION
ACKNOWLEDGMENTS
FIGURES AND TABLES
| Cause | (n=95) |
|---|---|
| Blood stream infection | 20 (21.1%) |
| Fever | 13 (13.7%) |
| Deep vein thrombosis | 3 (3.2%) |
| Catheter occlusion | 28 (29.5%) |
| Arm swelling | 8 (8.4%) |
| Phlebitis | 16 (16.8%) |
| Pain on insertion site | 7 (7.4%) |
| Variable | OR | 95% CI | P-value |
|---|---|---|---|
| Hypertension | 0.896 | (0.526, 1.527) | .686 |
| Diabetes | 1.356 | (0.769, 2.389) | 0.292 |
| Malignancy | 4.314 | (2.612, 7.125) | .000* |
| Chemotherapy | 1.757 | (1.002, 3.080) | .049* |
| ICU hospitalization | 4.627 | (2.311, 9.267) | .000* |
| Mechanical ventilation | 3.438 | (1.082, 10.923) | .036* |
| Major surgery | 0.917 | (0.450, 1.869) | .811 |
| Antibiotics | 1.087 | (0.662, 1.785) | .724 |
| TPN | 0.798 | (0.490, 1.298) | .363 |
| Side of arm | |||
| Right arm | 1 | Ref | Ref |
| Left arm | 0.522 | (0.283, 0.961) | .037* |
| Punctured vein | |||
| Brachial vein | 1 | Ref | Ref |
| Basilic vein | 0.346 | (0.215, 0.555) | .000* |
| Intermittent use | 1.614 | (0.705, 3.696) | .258 |
| Number of lumen | |||
| Triple lumen | 1 | Ref | Ref |
| Double lumen | 0.588 | (0.303, 1.144) | .118 |
| Variable | OR | 95% CI | P-value |
|---|---|---|---|
| Malignancy | 4.498 | (2.49, 8.125) | .000* |
| ICU hospitalization | 4.218 | (1.694, 10.505) | .002* |
| Side of arm | |||
| Right arm | 1 | Ref | Ref |
| Left arm | 0.279 | (0.143, 0.544) | .000* |
| Punctured vein | |||
| Brachial vein | 1 | Ref | Ref |
| Basilic vein | 0.323 | (0.192, 0.545) | .000* |
- 1. Pittiruti M, Malerba M, Carriero C, Tazza L, Gui D. Which is the easiest and safest technique for central venous access? A retrospective survey of more than 5,400 cases. J Vasc Access 2000;1:100.ArticlePubMedPDF
- 2. Fallouh N, McGuirk HM, Flanders SA, Chopra V. Peripherally inserted central catheter-associated deep vein thrombosis: a narrative review. Am J Med 2015;128:722-38. ArticlePubMed
- 3. Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M. ESPEN. guidelines on parenteral nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr 2009;28:365-77. PubMed
- 4. Xu T, Kingsley L, DiNucci S, Messer G, Jeong JH, Morgan B, et al. Safety and utilization of peripherally inserted central catheters versus midline catheters at a large academic medical center. Am J Infect Control 2016;44:1458-61. ArticlePubMed
- 5. Sakai T, Kohda K, Konuma Y, Hiraoka Y, Ichikawa Y, Ono K, et al. A role for peripherally inserted central venous catheters in the prevention of catheter-related blood stream infections in patients with hematological malignancies. Int J Hematol 2014;100:592-8. ArticlePubMedPDF
- 6. Chopra V, O'Horo JC, Rogers MA, Maki DG, Safdar N. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 2013;34:908-18. ArticlePubMed
- 7. Chopra V, Ratz D, Kuhn L, Lopus T, Chenoweth C, Krein S. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med 2014;127:319-28. ArticlePubMed
- 8. Gunst M, Matsushima K, Vanek S, Gunst R, Shafi S, Frankel H. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surg Infect (Larchmt) 2011;12:279-82. ArticlePubMed
- 9. Meyer BM. Managing peripherally inserted central catheter thrombosis risk: a guide for clinical best practice. J Assoc Vasc Access 2011;16:144-7. ArticlePDF
- 10. Hoshal VL. Total intravenous nutrition with peripherally inserted silicone elastomer central venous catheters. Arch Surg 1975;110:644-6. ArticlePubMed
- 11. Graham DR, Keldermans MM, Klemm LW, Semenza NJ, Shafer ML. Infectious complications among patients receiving home intravenous therapy with peripheral, central, or peripherally placed central venous catheters. Am J Med 1991;91:95S-100S. Article
- 12. Merrell SW, Peatross BG, Grossman MD, Sullivan JJ, Harker WG. Peripherally inserted central venous catheters. Low-risk alternatives for ongoing venous access. West J Med 1994;160:25-30. PubMedPMC
- 13. Laurenzi L, Natoli S, Benedetti C, Marcelli ME, Tirelli W, DiEmidio L, et al. Cutaneous bacterial colonization, modalities of chemotherapeutic infusion, and catheter-related bloodstream infection in totally implanted venous access devices. Support Care Cancer 2004;12:805-9. ArticlePubMedPDF
- 14. Bashir MH, Olson LK, Walters SA. Suppression of regrowth of normal skin flora under chlorhexidine gluconate dressings applied to chlorhexidine gluconate-prepped skin. Am J Infect Control 2012;40:344-8. ArticlePubMed
- 15. Chopra V, Flanders SA, Saint S. The problem with peripherally inserted central catheters. JAMA 2012;308:1527-8. ArticlePubMed
- 16. Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 2006;81:1159-71. ArticlePubMed
- 17. Ajenjo MC, Morley JC, Russo AJ, McMullen KM, Robinson C, Williams RC, et al. Peripherally inserted central venous catheter-associated bloodstream infections in hospitalized adult patients. Infect Control Hosp Epidemiol 2011;32:125-30. ArticlePubMed
- 18. Safdar N, Maki DG. Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest 2005;128:489-95. ArticlePubMed
- 19. Periard D, Monney P, Waeber G, Zurkinden C, Mazzolai L, Hayoz D, et al. Randomized controlled trial of peripherally inserted central catheters vs. peripheral catheters for middle duration in-hospital intravenous therapy. J Thromb Haemost 2008;6:1281-8. ArticlePubMed
- 20. Al Raiy B, Fakih MG, Bryan-Nomides N, Hopfner D, Riegel E, Nenninger T, et al. Peripherally inserted central venous catheters in the acute care setting: a safe alternative to high-risk short-term central venous catheters. Am J Infect Control 2010;38:149-53. ArticlePubMed
- 21. Chemaly RF, de Parres JB, Rehm SJ, Adal KA, Lisgaris MV, Katz-Scott DS, et al. Venous thrombosis associated with peripherally inserted central catheters: a retrospective analysis of the Cleveland Clinic experience. Clin Infect Dis 2002;34:1179-83. ArticlePubMed
- 22. Worth LJ, Seymour JF, Slavin MA. Infective and thrombotic complications of central venous catheters in patients with hematological malignancy: prospective evaluation of nontunneled devices. Support Care Cancer 2009;17:811-8. ArticlePubMedPDF
- 23. Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol 2002;20:3276-81. ArticlePubMed
- 24. Sperry BW, Roskos M, Oskoui R. The effect of laterality on venous thromboembolism formation after peripherally inserted central catheter placement. J Vasc Access 2012;13:91-5. ArticlePubMedPDF
- 25. Liem TK, Yanit KE, Moseley SE, Landry GJ, Deloughery TG, Rumwell CA, et al. Peripherally inserted central catheter usage patterns and associated symptomatic upper extremity venous thrombosis. J Vasc Surg 2012;55:761-7. ArticlePubMed
- 26. Chopra V, Anand S, Krein SL, Chenoweth C, Saint S. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med 2012;125:733-41. ArticlePubMed
- 27. Lee AY, Levine MN, Butler G, Webb C, Costantini L, Gu C, et al. Incidence, risk factors, and outcomes of catheter-related thrombosis in adult patients with cancer. J Clin Oncol 2006;24:1404-8. ArticlePubMed
- 28. Vesely TM. Central venous catheter tip position: a continuing controversy. J Vasc Interv Radiol 2003;14:527-34. ArticlePubMed
- 29. Scott EC, Hudson KS, Trerotola S, Smith H, Porter D, Sood SL. Risk factors for venous thromboembolism in hospitalized cancer patients with central catheters. Blood 2010;116:810.ArticlePDF
- 30. Bouzad C, Duron S, Bousquet A, Arnaud FX, Valbousquet L, Weber-Donat G, et al. Peripherally inserted central catheter-related infections in a cohort of hospitalized adult patients. Cardiovasc Intervent Radiol 2016;39:385-93. ArticlePubMedPDF
References
Figure & Data
REFERENCES
Citations

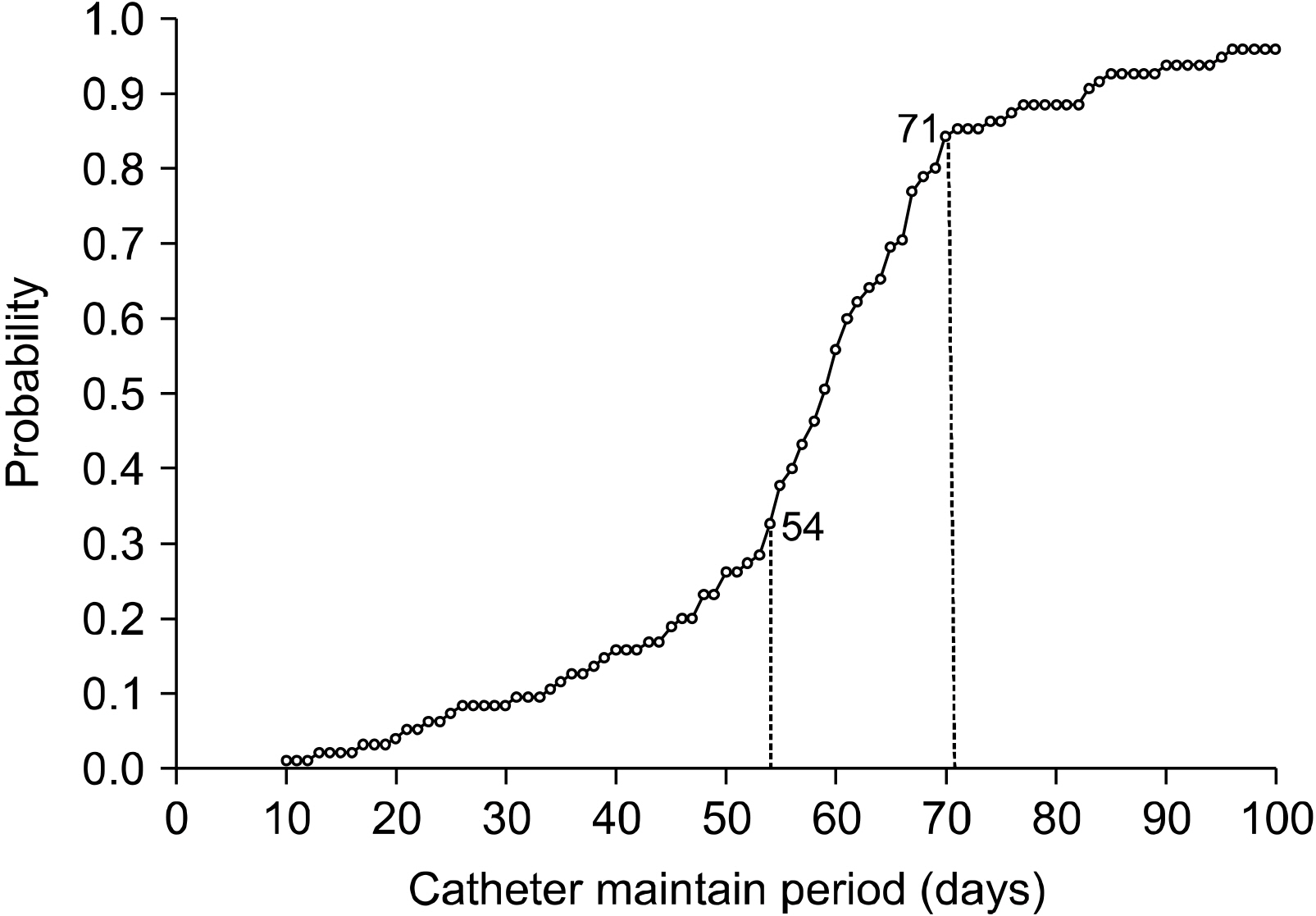
Fig. 1
Baseline characteristics of patients with PICC
| Group | |||
|---|---|---|---|
| Unexpected removal (n=95) | Success to maintain (n=312) | Total (n=407) | |
| Age, mean/(SD) | 67.1 (11.8) | 66.1 (14.4) | 66.3 (13.7) |
| Sex | |||
| Male | 52 (54.7%) | 161 (51.6%) | 213 (52.3%) |
| Female | 43 (45.3%) | 151 (48.4%) | 194 (47.7%) |
| Disease and condition | |||
| Hypertension | 23 (24.1%) | 82 (26.3%) | 105 (25.8%) |
| Diabetes | 21 (22.1%) | 54 (17.3%) | 75 (18.4%) |
| Malignancy | 68 (71.6%) | 115 (36.9%) | 183 (45.0%) |
| ICU hospitalization | 20 (21.1%) | 17 (5.5%) | 37 (9.1%) |
| Mechanical ventilation | 6 (6.3%) | 6 (1.9%) | 12 (3.0%) |
| Use of PICC | |||
| Chemotherapy | 23 (24.2%) | 48 (15.4%) | 71 (17.4%) |
| Antibiotics | 30 (31.6%) | 93 (29.8%) | 123 (30.2%) |
| TPN | 62 (65.3%) | 219 (70.2%) | 281 (69.0%) |
| Intermittent use | 9 (9.5%) | 19 (6.1%) | 28 (6.9%) |
| Characteristics of PICC | |||
| Side of arm | |||
| Left arm | 76 (80.0%) | 276 (88.5%) | 352 (86.5%) |
| Right arm | 19 (20.0%) | 36 (11.5%) | 55 (13.5%) |
| Punctured vein | |||
| Basilic vein | 46 (48.4%) | 228 (73.1%) | 274 (67.3%) |
| Brachial vein | 49 (51.6%) | 84 (26.9%) | 133 (32.7%) |
| Number of lumen | |||
| Double lumen | 80 (84.2%) | 281 (90.1%) | 361 (88.7%) |
| Triple lumen | 15 (15.8%) | 31 (9.9%) | 46 (11.3%) |
| Catheter days, mean (day)/(SD) | 58.6 (19.1) | 81.5 (51.2) | 76.2 (49.8) |
PICC = peripherally inserted central catheter; SD = standard deviation; ICU = intensive care unit; TPN = total parenteral nutrition.
Causes of unexpected removal
| Cause | (n=95) |
|---|---|
| Blood stream infection | 20 (21.1%) |
| Fever | 13 (13.7%) |
| Deep vein thrombosis | 3 (3.2%) |
| Catheter occlusion | 28 (29.5%) |
| Arm swelling | 8 (8.4%) |
| Phlebitis | 16 (16.8%) |
| Pain on insertion site | 7 (7.4%) |
Univariate analysis for the risk factor of unexpected removal of PICC
| Variable | OR | 95% CI | P-value |
|---|---|---|---|
| Hypertension | 0.896 | (0.526, 1.527) | .686 |
| Diabetes | 1.356 | (0.769, 2.389) | 0.292 |
| Malignancy | 4.314 | (2.612, 7.125) | .000 |
| Chemotherapy | 1.757 | (1.002, 3.080) | .049 |
| ICU hospitalization | 4.627 | (2.311, 9.267) | .000 |
| Mechanical ventilation | 3.438 | (1.082, 10.923) | .036 |
| Major surgery | 0.917 | (0.450, 1.869) | .811 |
| Antibiotics | 1.087 | (0.662, 1.785) | .724 |
| TPN | 0.798 | (0.490, 1.298) | .363 |
| Side of arm | |||
| Right arm | 1 | Ref | Ref |
| Left arm | 0.522 | (0.283, 0.961) | .037 |
| Punctured vein | |||
| Brachial vein | 1 | Ref | Ref |
| Basilic vein | 0.346 | (0.215, 0.555) | .000 |
| Intermittent use | 1.614 | (0.705, 3.696) | .258 |
| Number of lumen | |||
| Triple lumen | 1 | Ref | Ref |
| Double lumen | 0.588 | (0.303, 1.144) | .118 |
*Statistically significant with P<0.05.
PICC = peripherally inserted central catheter; CI = confidence interval; ICU = intensive care unit; TPN = total parenteral nutrition.
Multivariate analysis for the risk factor of unexpected removal of PICC
| Variable | OR | 95% CI | P-value |
|---|---|---|---|
| Malignancy | 4.498 | (2.49, 8.125) | .000 |
| ICU hospitalization | 4.218 | (1.694, 10.505) | .002 |
| Side of arm | |||
| Right arm | 1 | Ref | Ref |
| Left arm | 0.279 | (0.143, 0.544) | .000 |
| Punctured vein | |||
| Brachial vein | 1 | Ref | Ref |
| Basilic vein | 0.323 | (0.192, 0.545) | .000 |
*Statistically significant with P<0.05.
PICC = peripherally inserted central catheter; CI = confidence interval; ICU = intensive care unit.
PICC = peripherally inserted central catheter; SD = standard deviation; ICU = intensive care unit; TPN = total parenteral nutrition.
*Statistically significant with P<0.05. PICC = peripherally inserted central catheter; CI = confidence interval; ICU = intensive care unit; TPN = total parenteral nutrition.
*Statistically significant with P<0.05. PICC = peripherally inserted central catheter; CI = confidence interval; ICU = intensive care unit.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN Cite
Cite

