Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 15(1); 2023 > Article
- Original article Comparison of a volume-based feeding protocol with standard feeding for trauma patients in intensive care units in Korea: a retrospective cohort study
-
Juhong Park1
 , Yesung Oh2
, Yesung Oh2 , Songhee Kwon2
, Songhee Kwon2 , Ji-hyun Lee2
, Ji-hyun Lee2 , Mihyang Kim2
, Mihyang Kim2 , Kyungjin Hwang1
, Kyungjin Hwang1 , Donghwan Choi1
, Donghwan Choi1 , Junsik Kwon1
, Junsik Kwon1
-
Annals of Clinical Nutrition and Metabolism 2023;15(1):22-29.
DOI: https://doi.org/10.15747/ACNM.2023.15.1.22
Published online: April 1, 2023
1Division of Trauma Surgery, Department of Surgery, Ajou University School of Medicine, Suwon, Korea
2Department of Food Services and Clinical Nutrition, Ajou University Hospital, Suwon, Korea
- Corresponding author: Junsik Kwon, email: aquaestel@gmail.com
© 2023 The Korean Society of Surgical Metabolism and Nutrition · The Korean Society for Parenteral and Enteral Nutrition
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,278 Views
- 42 Download
- 1 Crossref
Abstract
-
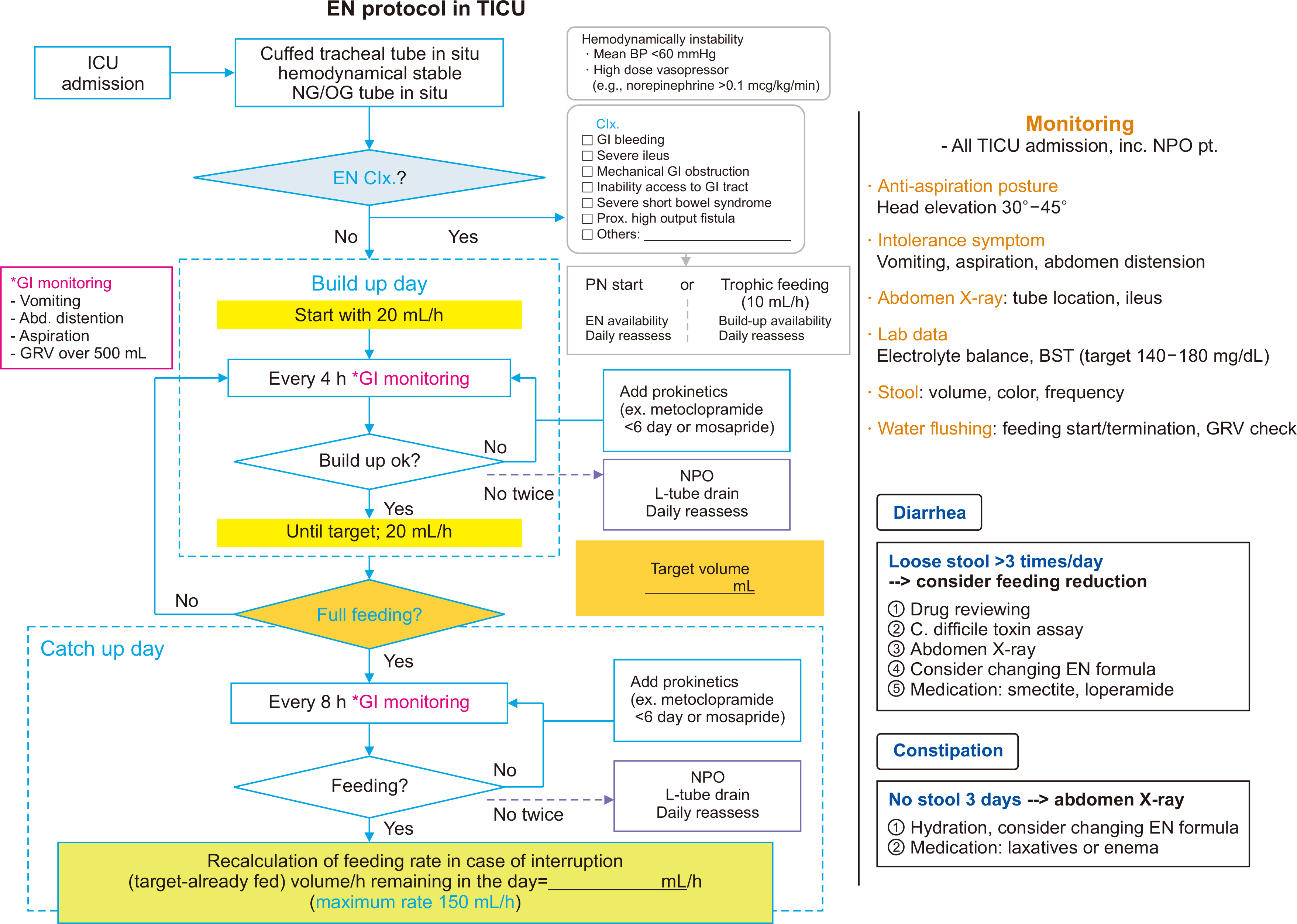
Purpose Although early enteral nutrition for critically ill patients is essential, it is difficult to provide enteral nutrition to trauma patients in early hospitalization stages due to frequent surgeries and examinations. We aimed to identify the effect of achieving early enteral nutrition goals and improving outcomes through a volume-based feeding (VBF) protocol for trauma patients.
-
Methods Patients who were admitted to the trauma intensive care units (TICUs) of the Ajou University Hospital from January 2020 to September 2021 and received enteral tube feeding for at least 7 days were studied. An institution-specific VBF protocol was developed, and nurses were trained in its execution. We retrospectively compared outcomes, such as in-hospital mortality and initial nutritional goal achievement, between the new and standard protocols.
-
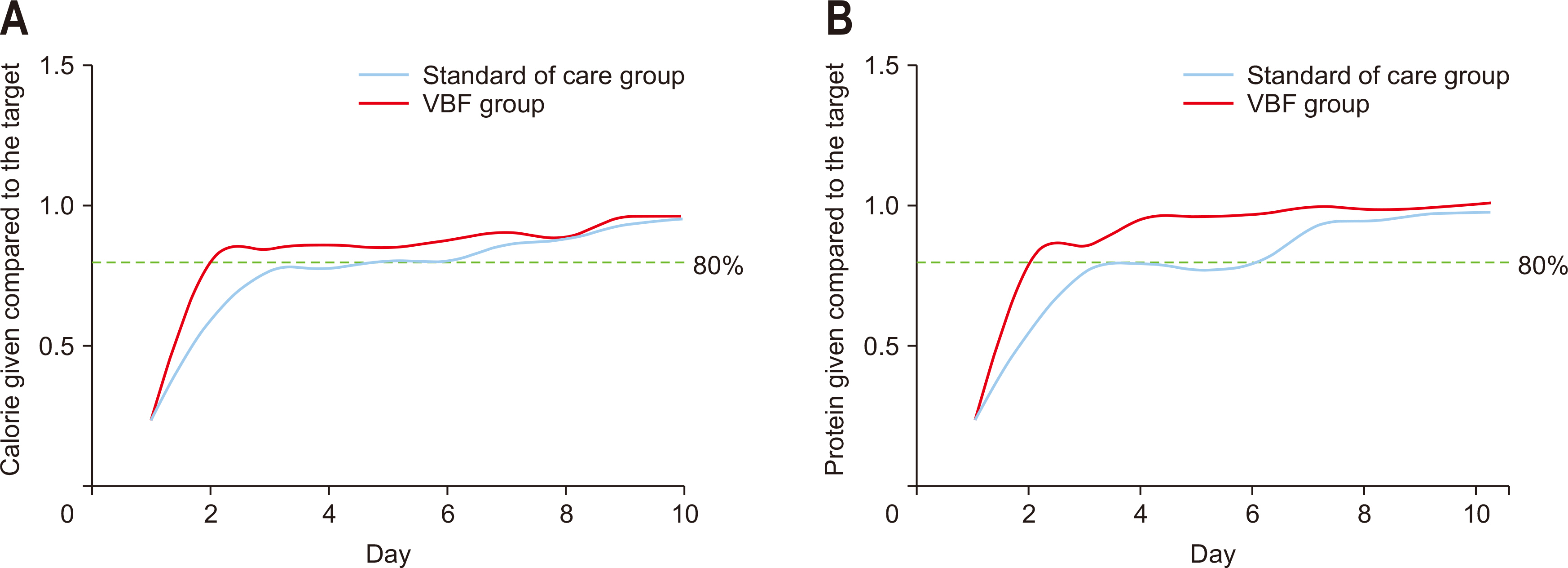
Results Among 2,935 patients, 109 met the inclusion criteria. Of these, 64 patients received nutrition through VBF, with no feeding intolerance symptoms. The VBF group started enteral nutrition approximately 16.9 hours earlier and group achieved 80% of the target calorie and protein intake approximately one day faster than the control group (n=45). The average calorie supply per body weight per day was 4.9 kcal/kg/day more in the VBF group. An increase of 0.2 g/kg/day was also observed in protein uptake. However, mortality and adverse hospital events did not differ between the groups.
-
Conclusion The VBF protocol for patients admitted to the TICU increased the initial nutrient supply without risk of feeding intolerance, but there was no improvement in major clinical outcomes, including mortality and adverse hospital events.
Introduction
Methods
Results
Discussion
Acknowledgments
Authors’ contribution
Conceptualization: JL, MK, JK. Data curation: YO, SK, JL, MK, JK. Formal analysis: MK, JK. Funding acquisition: JK. Investigation: YO, SK, MK, JK. Methodology: MK, JL, DC, JK. Project administration: JK. Resources: JP, YO, SK, JL, MK, DC, JK. Software: KH, JK. Supervision: JK. Validation: JP, JL, DC, JK. Visualization: KH, JP, JK. Writing – original draft: JP, JK. Writing – review & editing: JP, JK.
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Funding
This work was supported by the Korean Society for Parenteral and Enteral Nutrition.
Data availability
Contact the corresponding author for data availability.
Supplementary materials
None.
| Outcome |
VBF (n=64) |
Standard of care (n=45) |
P-value |
|---|---|---|---|
| Primary outcomes | |||
| Mortality | 6 (9.4) | 2 (4.4) | 0.47 |
| ICU LOS (day) | 16.5 (12.0–25.5) | 19 (11–30) | 0.71 |
| Hospital LOS (day) | 31.5 (22.8–46.0) | 39 (20–51) | 0.40 |
| Total ventilator days (day) | 10.5 (6.0–15.5) | 12 (8–22) | 0.28 |
| Sepsis | 6 (9.4) | 2 (4.4) | 0.47 |
| Pneumonia | 25 (39.1) | 16 (35.6) | 0.71 |
| ARDS | 7 (10.9) | 6 (13.3) | 0.70 |
| AKI | 4 (6.3) | 4 (8.9) | 0.72 |
| UTI | 3 (4.7) | 2 (4.4) | >0.99 |
| Delirium | 23 (35.9) | 18 (40.0) | 0.67 |
| Secondary outcomes | |||
| Time to EN initiation (h) | 24.6 (18.7–41.1) | 41.5 (22.0–58.1) | <0.01* |
| Target calorie (kcal/day) | 1,730.5 (1,581–1,860) | 1,725 (1,473–1,905) | 0.49 |
| Target 80% of calories achieved | 59 (92.2) | 37 (82.2) | 0.11 |
| Day on which 80% was achieved (day) | 2 (2–3) | 3 (2–5) | <0.01* |
| Calorie per body weight (kcal/kg/day) | 20.5 (16.0–24.7) | 15.6 (12.8–18.6) | <0.01* |
| Target protein (g/day) | 82 (74.5–88.6) | 77.7 (68.0–87.4) | 0.15 |
| Target 80% of calories achieved | 57 (89.1) | 37 (82.2) | 0.31 |
| Day when 80% protein was achieved (day) | 2 (2–3) | 3 (2–4) | 0.04* |
| Protein per body weight (g/kg/day) | 1.0 (0.8–1.2) | 0.8 (0.6–0.9) | <0.01* |
- 1. Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 2009;35:1728-37; Erratum in: Intensive Care Med 2009;35:1821. ArticlePubMedPDF
- 2. Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux RNMC, Delarue J, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502-9. ArticlePubMed
- 3. Yeh DD, Fuentes E, Quraishi SA, Cropano C, Kaafarani H, Lee J, et al. Adequate nutrition may get you home: effect of caloric/protein deficits on the discharge destination of critically ill surgical patients. JPEN J Parenter Enteral Nutr 2016;40:37-44. ArticlePubMed
- 4. Barr J, Hecht M, Flavin KE, Khorana A, Gould MK. Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest 2004;125:1446-57. ArticlePubMed
- 5. Doig GS, Simpson F, Finfer S, Delaney A, Davies AR, Mitchell I, et al. Nutrition Guidelines Investigators of the ANZICS Clinical Trials Group. Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial. JAMA 2008;300:2731-41. ArticlePubMed
- 6. Heyland DK, Cahill NE, Dhaliwal R, Sun X, Day AG, McClave SA. Impact of enteral feeding protocols on enteral nutrition delivery: results of a multicenter observational study. JPEN J Parenter Enteral Nutr 2010;34:675-84. ArticlePubMed
- 7. Taylor SJ, Fettes SB, Jewkes C, Nelson RJ. Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med 1999;27:2525-31. ArticlePubMed
- 8. Haskins IN, Baginsky M, Gamsky N, Sedghi K, Yi S, Amdur RL, et al. Volume-based enteral nutrition support regimen improves caloric delivery but may not affect clinical outcomes in critically ill patients. JPEN J Parenter Enteral Nutr 2017;41:607-11. ArticlePubMedPDF
- 9. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. American Society for Parenteral and Enteral Nutrition. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159-211; Erratum in: JPEN J Parenter Enteral Nutr 2016;40:1200. ArticlePubMed
- 10. Heyland DK, Murch L, Cahill N, McCall M, Muscedere J, Stelfox HT, et al. Enhanced protein-energy provision via the enteral route feeding protocol in critically ill patients: results of a cluster randomized trial. Crit Care Med 2013;41:2743-53. ArticlePubMed
- 11. Krebs ED, O'Donnell K, Berry A, Guidry CA, Hassinger TE, Sawyer RG. Volume-based feeding improves nutritional adequacy in surgical patients. Am J Surg 2018;216:1155-9. ArticlePubMed
- 12. Roberts S, Brody R, Rawal S, Byham-Gray L. Volume-based vs rate-based enteral nutrition in the intensive care unit: impact on nutrition delivery and glycemic control. JPEN J Parenter Enteral Nutr 2019;43:365-75. ArticlePubMedPDF
- 13. Lee JC, Williams GW, Kozar RA, Kao LS, Mueck KM, Emerald AD, et al. Multitargeted feeding strategies improve nutrition outcome and are associated with reduced pneumonia in a level 1 trauma intensive care unit. JPEN J Parenter Enteral Nutr 2018;42:529-37. ArticlePubMedPDF
- 14. Elia M, Normand C, Norman K, Laviano A. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr 2016;35:370-80. ArticlePubMed
- 15. Stratton RJ, Hébuterne X, Elia M. A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev 2013;12:884-97. ArticlePubMed
- 16. Wischmeyer PE, Carli F, Evans DC, Guilbert S, Kozar R, Pryor A, et al. Perioperative Quality Initiative (POQI) 2 Workgroup. American Society for Enhanced Recovery and Perioperative Quality Initiative joint consensus statement on nutrition screening and therapy within a surgical enhanced recovery pathway. Anesth Analg 2018;126:1883-95; Erratum in: Anesth Analg 2018;127:e95. ArticlePubMed
- 17. Yeh DD, Ortiz LA, Lee JM, Chan J, McKenzie K, Young B, et al. PEP uP (enhanced protein-energy provision via the enteral route feeding protocol) in surgical patients-a multicenter pilot randomized controlled trial. JPEN J Parenter Enteral Nutr 2020;44:197-204. ArticlePubMedPDF
- 18. Sachdev G, Backes K, Thomas BW, Sing RF, Huynh T. Volume-based protocol improves delivery of enteral nutrition in critically ill trauma patients. JPEN J Parenter Enteral Nutr 2020;44:874-9. ArticlePubMedPDF
References
Figure & Data
REFERENCES
Citations

- Early initiation of gastric tube feeding: ultrasound assessment. A prospective interventional study
Islam M. Elbardan, Ahmed A. Alla Ossman, Nada El Kayal, Assem A. ElRazek Abd-Rabih
Research and Opinion in Anesthesia & Intensive Care.2024; 11(4): 270. CrossRef
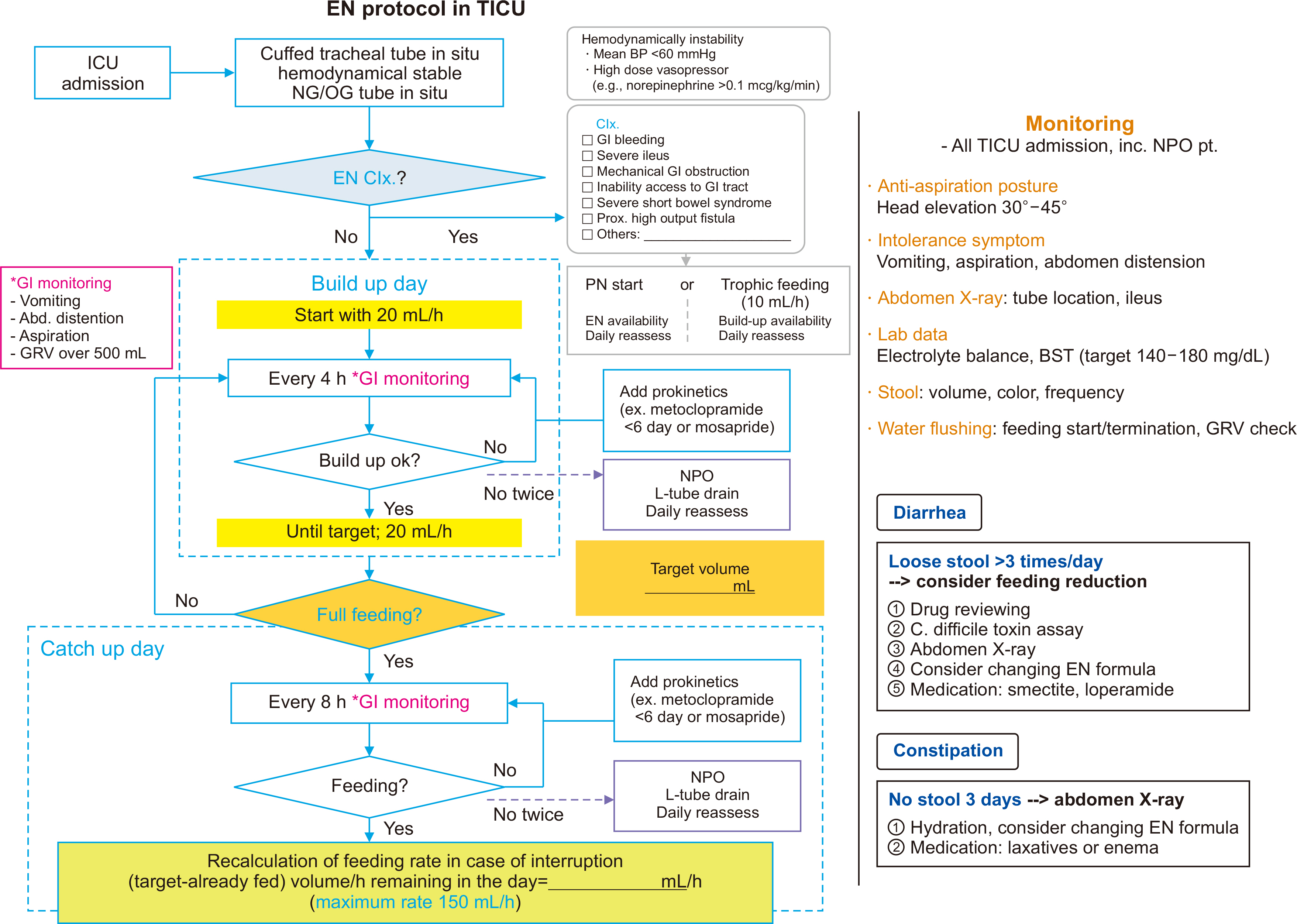
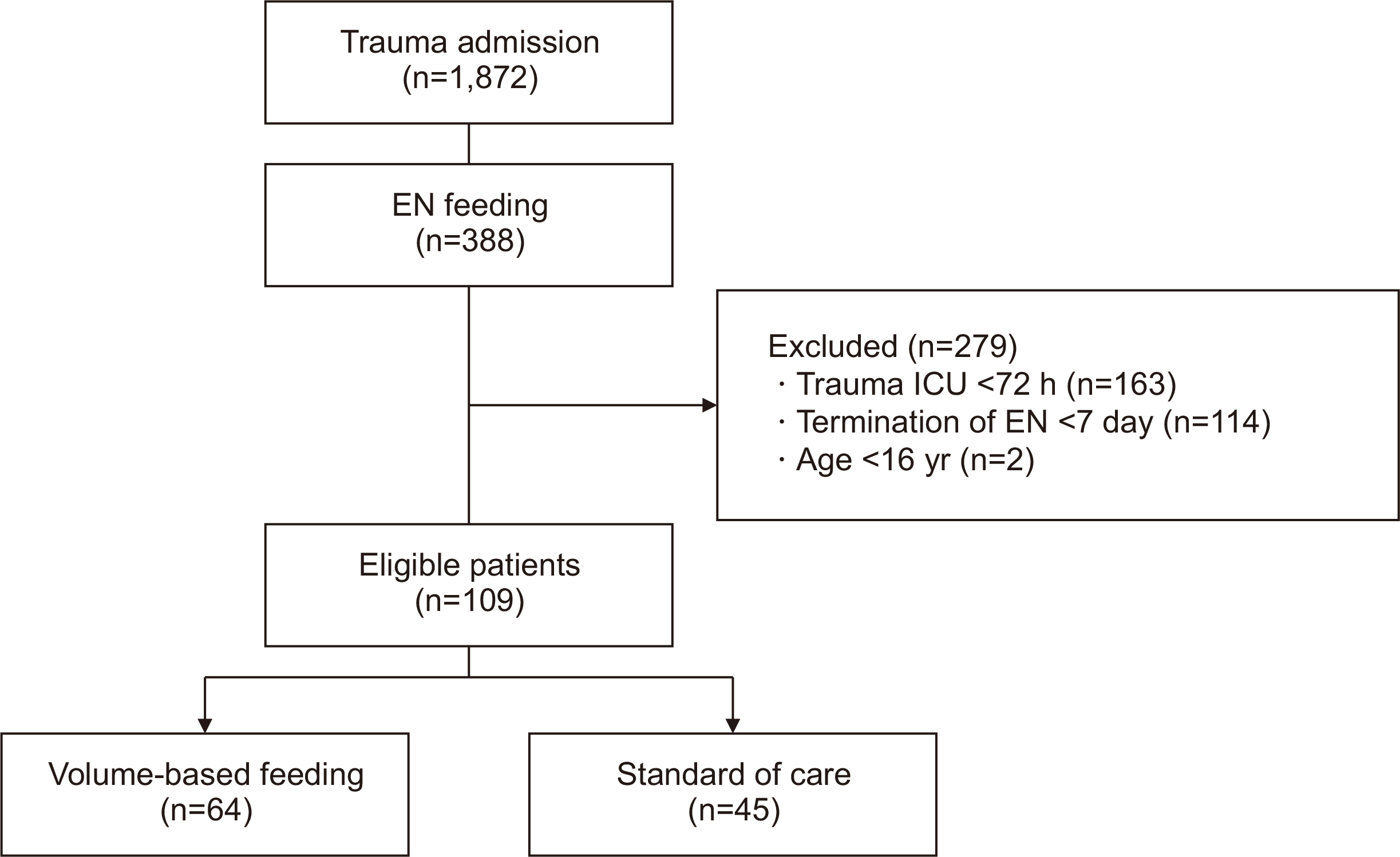
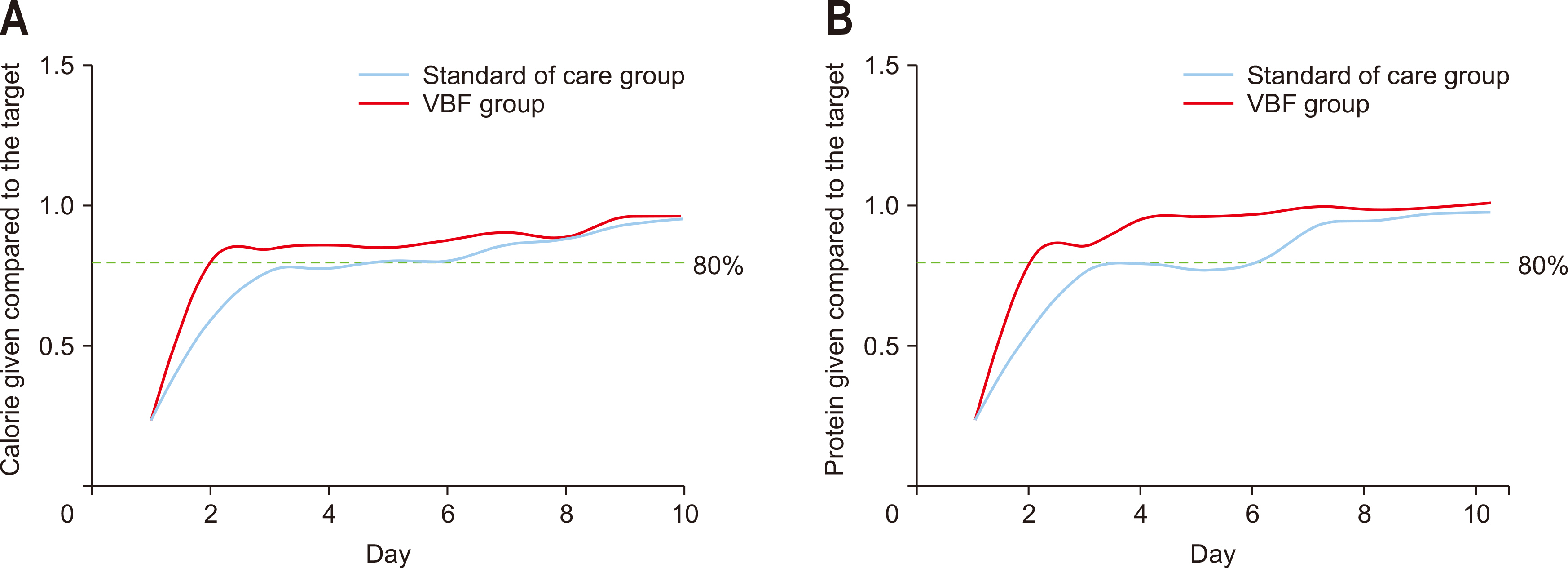
Fig. 1
Fig. 2
Fig. 3
Patient demographics and enteral nutrition tolerances
| Variable | VBF (n=64) |
Standard of care (n=45) |
P-value |
|---|---|---|---|
| Age (yr) | 61 (46–72) | 60 (41–69) | 0.52 |
| Sex, male | 56 (87.5) | 34 (75.6) | 0.11 |
| Weight (kg) | 68.1 (54.2–75.4) | 67.1 (56.4–78.5) | 0.76 |
| Body mass index (kg/m2) | 23.7 (20.8–26.1) | 24.6 (22.0–26.0) | 0.64 |
| Injury Severity Score | 33 (23.5–43.0) | 29 (19–43) | 0.30 |
| TRISS | 0.87 (0.66–0.91) | 0.91 (0.68–0.95) | 0.30 |
| Glasgow Coma Scale | 11 (8–14) | 13 (7–15) | 0.43 |
| Mechanism | 0.79 | ||
| Blunt | 59 (92.2) | 45 (100) | |
| Penetration | 1 (1.6) | 0 | |
| Others | 4 (6.3) | 0 | |
| Red blood cell/24 h | 4 (2.0–10.5) | 4 (2.0–12.3) | 0.79 |
| Operation | 49 (76.6) | 36 (80.0) | 0.67 |
| Laparotomy | 11 (17.2) | 7 (15.6) | 0.82 |
| Ileus | 4 (6.3) | 2 (4.4) | >0.99 |
| Vomiting | 4 (6.3) | 3 (6.7) | >0.99 |
| Constipation | 8 (12.5) | 6 (13.3) | 0.90 |
| Diarrhea | 7 (10.9) | 4 (8.9) | >0.99 |
| Abdominal distension | 7 (10.9) | 4 (8.9) | >0.99 |
Values are presented as median (IQR) or number (%).
VBF = volume-based feeding; TRISS = Trauma and Injury Severity Score.
Enteral nutrition status at the end of follow-up
| EN status | VBF (n=64) |
Standard of care (n=45) |
|---|---|---|
| No cessation of EN | 28 (43.8) | 19 (42.2) |
| Transition to oral feeding | 32 (50.0) | 19 (42.2) |
| Deceased | 1 (1.6) | 0 |
| Terminated due to feeding intolerance |
3 (4.7) | 7 (15.6) |
Values are presented as number (%).
EN = enteral nutrition; VBF = volume-based feeding.
Primary and secondary outcomes of patients
| Outcome | VBF (n=64) |
Standard of care (n=45) |
P-value |
|---|---|---|---|
| Primary outcomes | |||
| Mortality | 6 (9.4) | 2 (4.4) | 0.47 |
| ICU LOS (day) | 16.5 (12.0–25.5) | 19 (11–30) | 0.71 |
| Hospital LOS (day) | 31.5 (22.8–46.0) | 39 (20–51) | 0.40 |
| Total ventilator days (day) | 10.5 (6.0–15.5) | 12 (8–22) | 0.28 |
| Sepsis | 6 (9.4) | 2 (4.4) | 0.47 |
| Pneumonia | 25 (39.1) | 16 (35.6) | 0.71 |
| ARDS | 7 (10.9) | 6 (13.3) | 0.70 |
| AKI | 4 (6.3) | 4 (8.9) | 0.72 |
| UTI | 3 (4.7) | 2 (4.4) | >0.99 |
| Delirium | 23 (35.9) | 18 (40.0) | 0.67 |
| Secondary outcomes | |||
| Time to EN initiation (h) | 24.6 (18.7–41.1) | 41.5 (22.0–58.1) | <0.01 |
| Target calorie (kcal/day) | 1,730.5 (1,581–1,860) | 1,725 (1,473–1,905) | 0.49 |
| Target 80% of calories achieved | 59 (92.2) | 37 (82.2) | 0.11 |
| Day on which 80% was achieved (day) | 2 (2–3) | 3 (2–5) | <0.01 |
| Calorie per body weight (kcal/kg/day) | 20.5 (16.0–24.7) | 15.6 (12.8–18.6) | <0.01 |
| Target protein (g/day) | 82 (74.5–88.6) | 77.7 (68.0–87.4) | 0.15 |
| Target 80% of calories achieved | 57 (89.1) | 37 (82.2) | 0.31 |
| Day when 80% protein was achieved (day) | 2 (2–3) | 3 (2–4) | 0.04 |
| Protein per body weight (g/kg/day) | 1.0 (0.8–1.2) | 0.8 (0.6–0.9) | <0.01 |
Values are presented as number (%) or median (IQR).
VBF = volume-based feeding; ICU = intensive care unit; LOS = length of stay; ARDS = acute respiratory distress syndrome; AKI = acute kidney injury; UTI = urinary tract infection; EN = enteral nutrition.
*p<0.05.
Values are presented as median (IQR) or number (%). VBF = volume-based feeding; TRISS = Trauma and Injury Severity Score.
Values are presented as number (%). EN = enteral nutrition; VBF = volume-based feeding.
Values are presented as number (%) or median (IQR). VBF = volume-based feeding; ICU = intensive care unit; LOS = length of stay; ARDS = acute respiratory distress syndrome; AKI = acute kidney injury; UTI = urinary tract infection; EN = enteral nutrition. *p<0.05.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN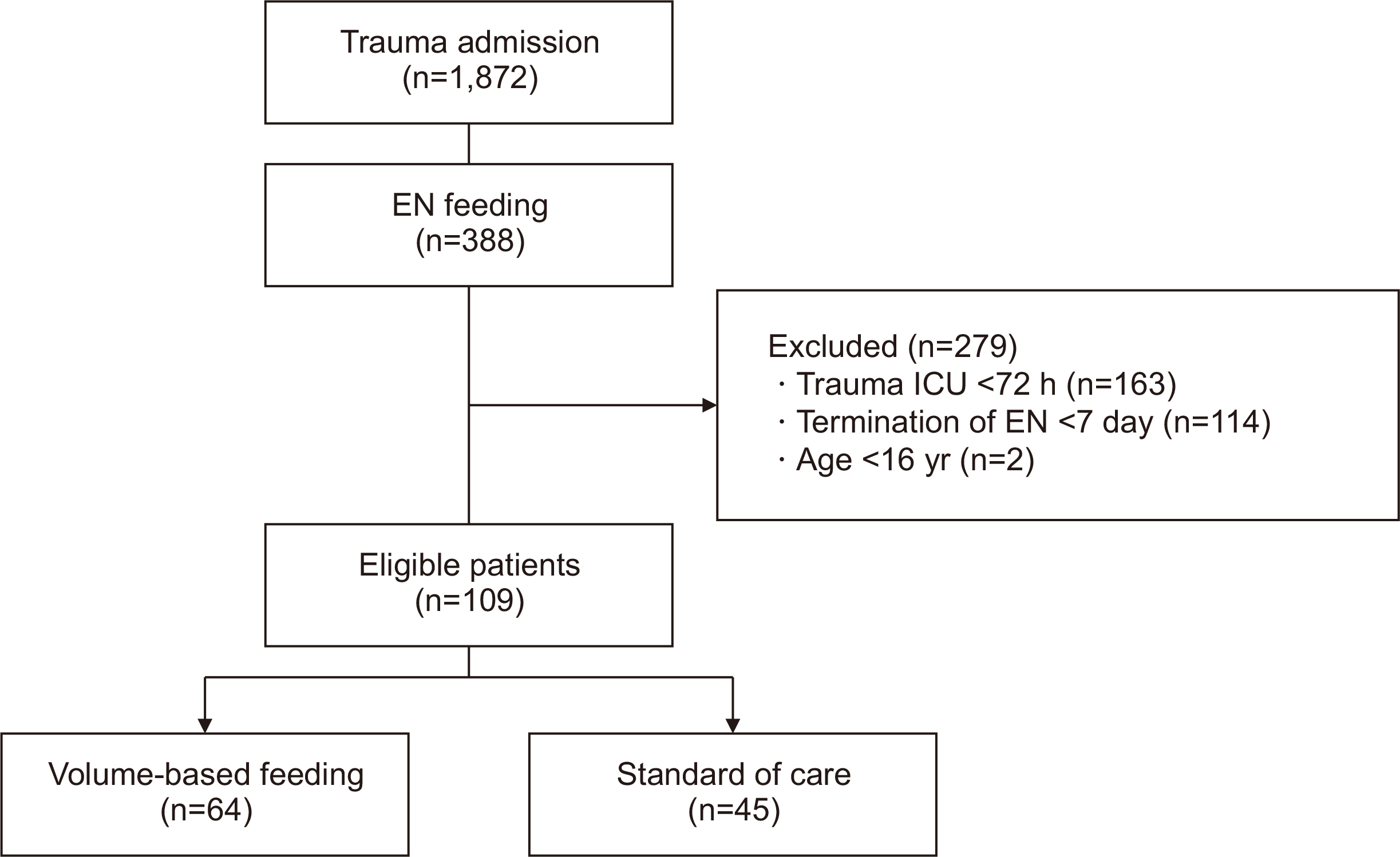
 Cite
Cite

