Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 15(3); 2023 > Article
- Review Role of nutrition in wound healing and nutritional recommendations for promotion of wound healing: a narrative review
-
Myoungjean Ju1
 , Yoonhong Kim2
, Yoonhong Kim2 , Kyung Won Seo2
, Kyung Won Seo2
-
Annals of Clinical Nutrition and Metabolism 2023;15(3):67-71.
DOI: https://doi.org/10.15747/ACNM.2023.15.3.67
Published online: December 1, 2023
1Department of Nursing, Kosin University Gospel Hospital, Busan, Korea
2Department of Surgery, Kosin University Gospel Hospital, Busan, Korea
- Corresponding author: Kyung Won Seo, email: hahachristi@gmail.com
© 2023 The Korean Society of Surgical Metabolism and Nutrition · The Korean Society for Parenteral and Enteral Nutrition
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 65,535 Views
- 1,811 Download
- 14 Crossref
Abstract
-
Purpose Addressing both malnutrition and wound healing requires strategic intervention. However, guidelines for adequate nutrition for a variety of wounds are lacking. Based on the latest literature review, we summarize the role of nutrition in each stage of wound healing and nutritional recommendations for wound healing.
-
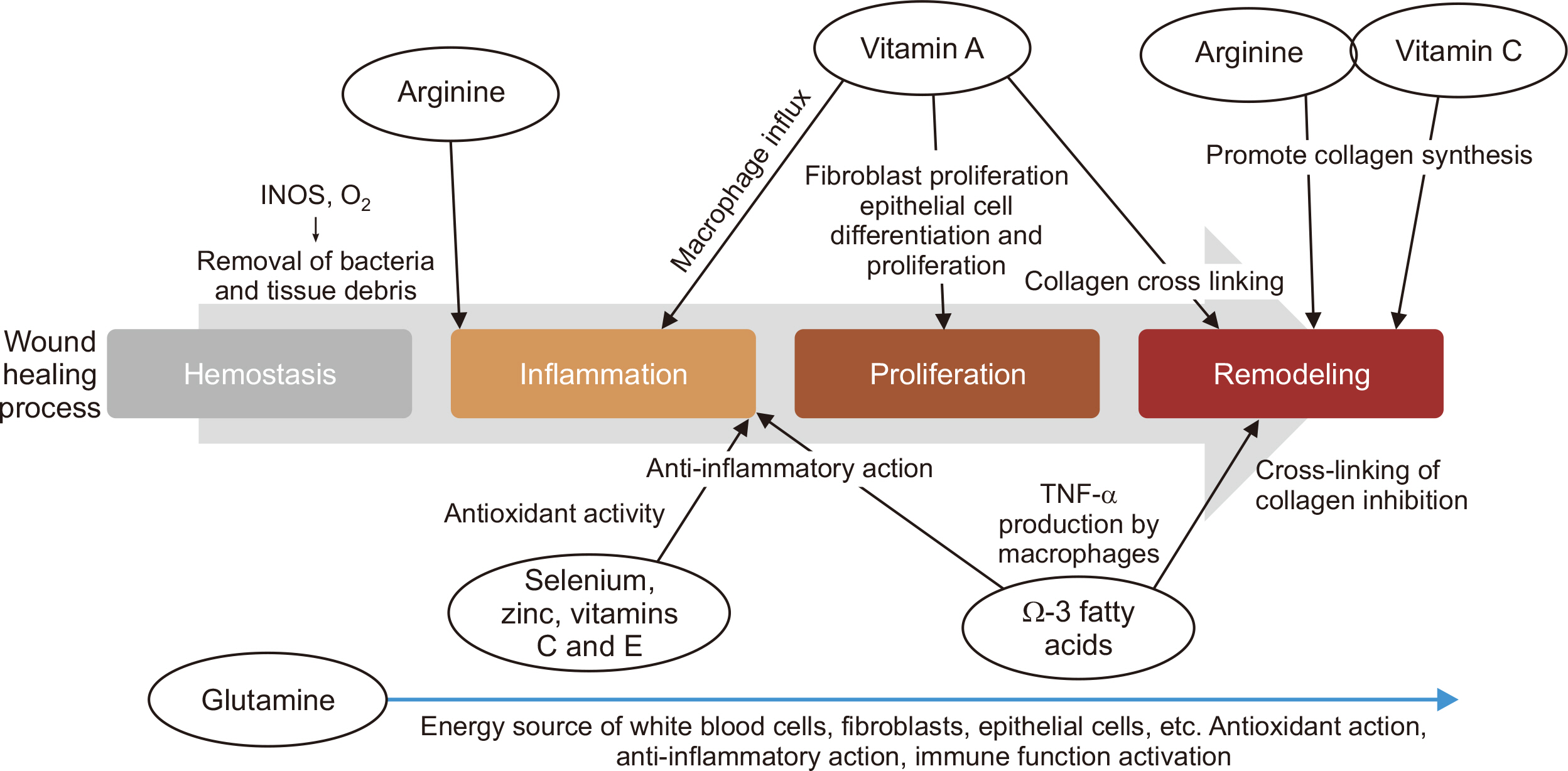
Current concept Wounds undergo three healing phases inflammatory, proliferative, and remodeling. The inflammatory phase involves clotting and cleaning the wound. The proliferative phase builds the wound bed through tissue growth. In the remodeling phase, collagen strength increases. Proper nutrition is crucial throughout. During inflammation, calcium, vitamin K, A, and E, zinc, and proteins are essential. In proliferation, amino acids, B vitamins, lipids, zinc, and iron play key roles. During remodeling, vitamins C and E, zinc, and water are critical for collagen synthesis and skin cell maturation. Vulnerable groups like the elderly, newborns, and obese patients need proper nutrition for skin maintenance. For pressure ulcers with malnutrition risk, recommendations are 30–35 kcal/kg/day energy, 1.25–1.5 g/kg/day protein, and 30 mL/kg water. Supplements might be added if regular meals don’t meet needs. For diabetic foot ulcers, despite common deficiencies, the 2019 International Working Group on the Diabetic Foot advises against prioritizing nutritional interventions over standard care due to limited high-quality evidence.
-
Conclusion Despite limited guidelines, nutrition assessment is vital for wound evaluation. A multidisciplinary approach is key, emphasizing nutrition’s role in wound healing. Implementing nutritional interventions tailored to the wound and the individual’s nutritional status is essential. This comprehensive strategy ensures the best wound care outcomes.
Introduction
Role of nutrients in each phase of wound healing
Nutritional assessment
Nutrition guidelines for various wounds
Conclusion
Supplementary materials
Acknowledgments
Authors’ contribution
Conceptualization: KWS. Formal analysis: MJ, KWS. Investigation: MJ, YK, KWS. Methodology: MJ, KWS. Project administration: MJ, KWS. Writing – original draft: MJ, KWS. Writing – review & editing: MJ, YK, KWS.
Conflict of interest
Kyung Won Seo is an editorial board member of the journal, but was not involved in the review process of this manuscript. Otherwise, there is no conflict of interest to disclose.
Funding
None.
Data availability
None.
Data from European Pressure Ulcer Advisory Panel, 2019 [23].
- 1. Spear M. Acute or chronic? What's the difference? Plast Surg Nurs 2013;33:98-100. ArticlePubMed
- 2. Rhie JW. Chronic wound. J Korean Med Assoc 2015;58:784-5. Article
- 3. Santamaria N, Creehan S, Fletcher J, Alves P, Gefen A. Preventing pressure injuries in the emergency department: current evidence and practice considerations. Int Wound J 2019;16:746-52. ArticlePubMedPMCPDF
- 4. Choi SW, Seo KB. Treatment of diabetic foot ulcer. J Korean Wound Manag 2014;10:20-2. Article
- 5. Medlin S. Nutrition for wound healing. Br J Nurs 2012;21:S11-2. S14-5. Article
- 6. Korean Society of Surgical Metabolism and Nutrition. Clinical metabolism and nutrition for surgical patients. Gabon Medical Book; 2016. Article
- 7. Tsugawa N, Shiraki M. Vitamin K nutrition and bone health. Nutrients 2020;12:1909.ArticlePubMedPMC
- 8. Lansdown AB. Nutrition 2: a vital consideration in the management of skin wounds. Br J Nurs 2004;13:1199-210. ArticlePubMed
- 9. Brown KL, Phillips TJ. Nutrition and wound healing. Clin Dermatol 2010;28:432-9. ArticlePubMed
- 10. Deng L, Du C, Song P, Chen T, Rui S, Armstrong DG, et al. The role of oxidative stress and antioxidants in diabetic wound healing. Oxid Med Cell Longev 2021;2021:8852759. ArticlePubMedPMCPDF
- 11. Demling RH. 2009;Nutrition, anabolism, and the wound healing process: an overview. Eplasty 9:e9. ArticlePubMedPMC
- 12. Munoz N, Litchford M, Cereda E. 2022;Nutrition and wound care. Phys Med Rehabil Clin N Am 33:811-22. ArticlePubMed
- 13. Wild T, Rahbarnia A, Kellner M, Sobotka L, Eberlein T. Basics in nutrition and wound healing. Nutrition 2010;26:862-6. ArticlePubMed
- 14. Sherman AR, Barkley M. Nutrition and wound healing. J Wound Care 2011;20:357-8. 360. 362-7. ArticlePubMed
- 15. Grada A, Phillips TJ. Nutrition and cutaneous wound healing. Clin Dermatol 2022;40:103-13. ArticlePubMed
- 16. Langer G, Fink A. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev 2014;2014:CD003216. ArticlePubMedPMC
- 17. Saeg F, Orazi R, Bowers GM, Janis JE. 2021;Evidence-based nutritional interventions in wound care. Plast Reconstr Surg 148:226-38. ArticlePubMed
- 18. Flanigan KH. Nutritional aspects of wound healing. Adv Wound Care 1997;10:48-52. ArticlePubMed
- 19. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res 2010;89:219-29. ArticlePubMedPMCPDF
- 20. Mukherjee K, Kavalukas SL, Barbul A. Nutritional aspects of gastrointestinal wound healing. Adv Wound Care (New Rochelle) 2016;5:507-15. ArticlePubMedPMC
- 21. Jaffe L, Wu S. The role of nutrition in chronic wound care management: what patients eat affects how they heal. Podiatry Manag 2017;11/12:77-83.Article
- 22. National Institute for Health and Care Excellence (NICE). Nutrition support in adults (QS24). NICE; 2012.Article
- 23. European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. The 2019 international prevention and treatment of pressure ulcers/injuries: clinical practice guideline. EPUAP; 2019.Article
- 24. Da Porto A, Miranda C, Brosolo G, Zanette G, Michelli A, Ros RD. Nutritional supplementation on wound healing in diabetic foot: what is known and what is new? World J Diabetes 2022;13:940-8. ArticlePubMedPMC
- 25. Rayman G, Vas P, Dhatariya K, Driver V, Hartemann A, Londahl M, et al. 2020;; International Working Group on the Diabetic Foot (IWGDF). Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes Metab Res Rev 36 Suppl 1:e3283. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

- Assessment of energy requirements in patients with obesity: A narrative review
Cagney Cristancho, Kris M. Mogensen, Malcolm K. Robinson
Nutrition in Clinical Practice.2026; 41(1): 54. CrossRef - Zinc supplementation and 60-day mortality in patients receiving total parenteral nutrition: a single-center experience
Mei-Yuan Liu, Chia-Yin Kuo, Hwung-Chung Lee, Jheng-Yan Wu
Frontiers in Nutrition.2026;[Epub] CrossRef - Electrospun-based nanofibers as ROS-scavenging scaffolds for accelerated wound healing: a narrative review
Mohammad Ebrahim Astaneh, Narges Fereydouni
International Journal of Polymeric Materials and Polymeric Biomaterials.2025; 74(15): 1349. CrossRef - Implementing a screening protocol for food insecure patients within a long‐term acute care hospital (LTACH): A community health needs assessment (CHNA)
Molly MacDonald, Christopher Stimson, Marti Samsel, Tina Gross
Nutrition in Clinical Practice.2025; 40(6): 1598. CrossRef - Nanoformulations Loaded with Phytochemicals for Combating Wound Infections and Promoting Wound Healing: Current Applications and Innovations
Panoraia I. Siafaka, Androulla N. Miliotou, Mehmet Evren Okur, Gökçe Karaotmarlı Güven, Ioannis D. Karantas, Neslihan Üstündağ Okur
Applied Sciences.2025; 15(10): 5413. CrossRef - Combining Topical Oxygen and Negative-Pressure Wound Therapy: New Insights from a Pilot Study on Chronic Wound Treatment
Bartosz Molasy, Mateusz Frydrych, Rafał Kuchciński, Stanisław Głuszek
Journal of Clinical Medicine.2025; 14(15): 5564. CrossRef - Undifferentiated connective tissue dysplasia and skin: what to do? Dietitian’s position
E. A. Nikitina, S. V. Orlova, T. T. Batysheva, N. V. Balashova, M. V. Alekseeva
Medical alphabet.2025; 1(19): 60. CrossRef - Nutritional Immunity in Wound Infection: Unveiling the Role of Dietary Elements in Host–Pathogen Interaction
Chaoming Chen, Xuanfan Hu, Da He, Xuemei He, Lan Shen
Food Science & Nutrition.2025;[Epub] CrossRef - Role of Nutrients and Diet in Wound Healing: The Emerging Paradigm for Effective Therapy
Aishik Banerjee, Arup Ghosh, Subhrajyoty Basu, Soumitra Sahana, Amit Kundu, Sumanta Mondal
Current Indian Science.2025;[Epub] CrossRef - Lueyang Black‐Boned Chicken and Black Bean Soup Promoting the Acute Healing of Skin Wounds, Accompanying Special Flavor Substances
Mengya Zhao, Zining Luo, Pengyan Tong, Yining Jia, Xin Yang, Jing Liu, Fangyu Long
Food Chemistry International.2025;[Epub] CrossRef - Cancer-Related Malnutrition and Oxidative Stress in Colorectal Cancer Surgery: A Narrative Review of Pathophysiology and Postoperative Outcomes
Andrii Zahorodnii, Alicja Jelska, Paulina Głuszyńska, Hady Razak Hady
Antioxidants.2025; 14(11): 1289. CrossRef - UCI Sports Nutrition Project: The Role of Nutrition in the Prevention and Management of Illnesses and Injuries in Elite Cycling
Patrick B. Wilson, David B. Pyne, Adrian Rotunno
International Journal of Sport Nutrition and Exercise Metabolism.2025; : 1. CrossRef - Clinical Impact of Nutritional Intervention on Pressure Injury Healing in a Paraplegic Patient: A Case Report
Young ran Kim, Mi young Jang, Jun ho Park
Clinical Nutrition Research.2025; 14(4): 241. CrossRef - Impact of Epigenetics, Diet, and Nutrition-Related Pathologies on Wound Healing
John Hajj, Brandon Sizemore, Kanhaiya Singh
International Journal of Molecular Sciences.2024; 25(19): 10474. CrossRef
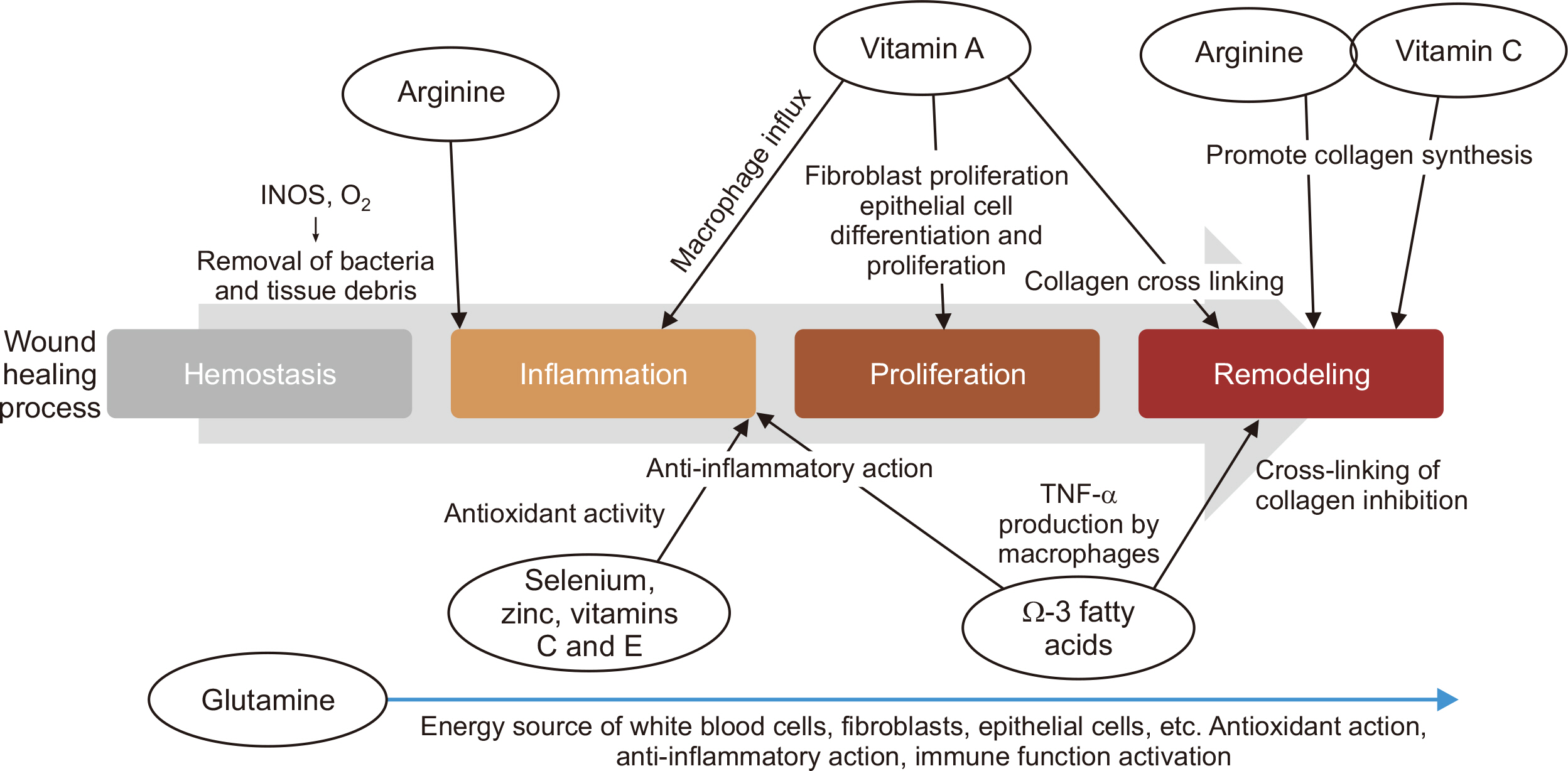
Fig. 1
Suggestion of supplementation regimen for malnourished or at risk of malnutrition
| Nutrient | Stage I pressure injury | Stage 2 or greater pressure injury |
|---|---|---|
| Calories | 30–35 kcal/kg/day | Over than 30–35 kcal/kg/day |
| Protein | 1.2–1.5 g/kg/day | Over than 1.2–1.5 g/kg/day |
| Additional oral nutritional supplement |
- | Arginine, zinc, antioxidant supplements |
Data from European Pressure Ulcer Advisory Panel, 2019 [
Data from European Pressure Ulcer Advisory Panel, 2019 [

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN Cite
Cite

