Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > Ann Clin Nutr Metab > Volume 17(1); 2025 > Article
- Guideline A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part I. prescribing enteral nutrition orders
-
Ye Rim Chang1
 , Bo-Eun Kim2
, Bo-Eun Kim2 , In Seok Lee3
, In Seok Lee3 , Youn Soo Cho4
, Youn Soo Cho4 , Sung-Sik Han5
, Sung-Sik Han5 , Eunjung Kim6
, Eunjung Kim6 , Hyunjung Kim2
, Hyunjung Kim2 , Jae Hak Kim7
, Jae Hak Kim7 , Jeong Wook Kim8
, Jeong Wook Kim8 , Sung Shin Kim9
, Sung Shin Kim9 , Eunhee Kong10
, Eunhee Kong10 , Ja Kyung Min11
, Ja Kyung Min11 , Chi-Min Park12
, Chi-Min Park12 , Jeongyun Park13
, Jeongyun Park13 , Seungwan Ryu14
, Seungwan Ryu14 , Kyung Won Seo15
, Kyung Won Seo15 , Jung Mi Song16
, Jung Mi Song16 , Minji Seok17
, Minji Seok17 , Eun-Mi Seol18
, Eun-Mi Seol18 , Jinhee Yoon19
, Jinhee Yoon19 , Jeong Meen Seo20
, Jeong Meen Seo20 , for KSPEN Enteral Nutrition Committee
, for KSPEN Enteral Nutrition Committee -
Annals of Clinical Nutrition and Metabolism 2025;17(1):3-8.
DOI: https://doi.org/10.15747/ACNM.25.0002
Published online: April 1, 2025
1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
2Department of Dietetics, Samsung Medical Center, Seoul, Korea
3Department of Nutrition, Kyung Hee University Medical Center, Seoul, Korea
4Department of Nutrition Care, Severance Hospital, Yonsei University Health System, Seoul, Korea
5Center for Liver and Pancreatobiliary Cancer, National Cancer Center, Goyang, Korea
6Department of Nutritional Support Team, Seoul National University Hospital, Seoul, Korea
7Department of Internal Medicine, Myongji Hospital, Goyang, Korea
8Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
9Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
10Department of Family Medicine, Kosin University Gospel Hospital, Busan, Korea
11Graduate School of Nursing Science, Sungkyunkwan University, Seoul, Korea
12Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
13Department of Clinical Nursing, University of Ulsan, Ulsan, Korea
14Department of Surgery, Keimyung University Dongsan Hospital, Daegu, Korea
15Department of Surgery, Kosin University College of Medicine, Busan, Korea
16Nutrition Support Team, Asan Medical Center, Seoul, Korea
17Department of Nursing, Keimyung University Dongsan Medical Center, Daegu, Korea
18Department of Nursing, Seoul National University Hospital, Seoul, Korea
19Department of Home Health Care, Samsung Medical Center, Seoul, Korea
20Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- Corresponding author: Jeong Meen Seo, e-mail: jm0815.seo@samsung.com
© 2025 Korean Society of Surgical Metabolism and Nutrition · Korean Society for Parenteral and Enteral Nutrition · Asian Society of Surgical Metabolism and Nutrition · Japanese Society for Surgical Metabolism and Nutrition
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,864 Views
- 183 Download
- 1 Crossref
Abstract
-
Purpose This study aimed to develop a comprehensive practical guide for enteral nutrition (EN) designed to enhance patient safety and reduce complications in Korea. Under the leadership of the Korean Society for Parenteral and Enteral Nutrition (KSPEN), the initiative sought to standardize EN procedures, improve decision-making, and promote effective multidisciplinary communication.
-
Methods The KSPEN EN committee identified key questions related to EN practices and organized them into seven sections such as prescribing, delivery route selection, formula preparation, administration, and quality management. Twenty-one experts, selected based on their expertise, conducted a thorough literature review to formulate evidence-based recommendations. Drafts underwent peer review both within and across disciplines, with final revisions completed by the KSPEN Guideline Committee. The guide, which will be published in three installments, addresses critical elements of EN therapy and safety protocols.
-
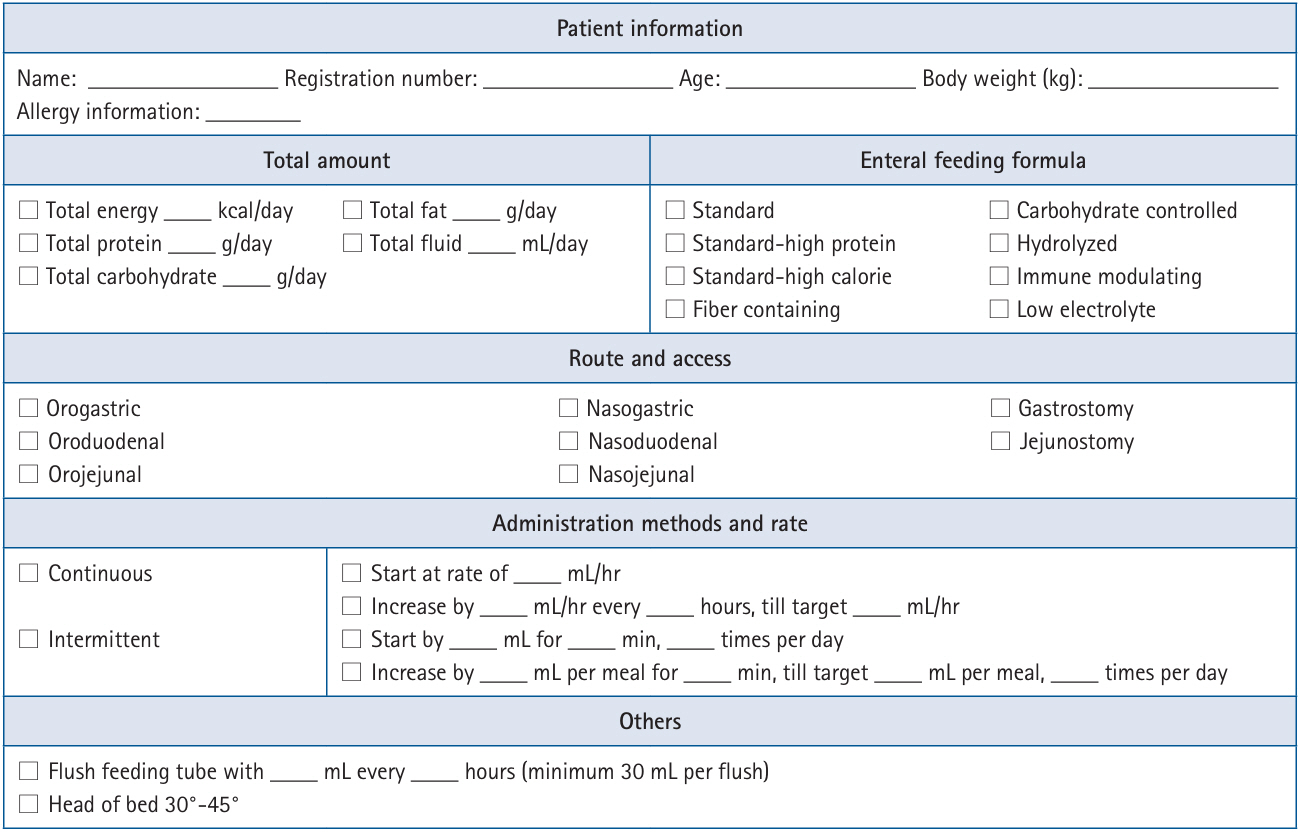
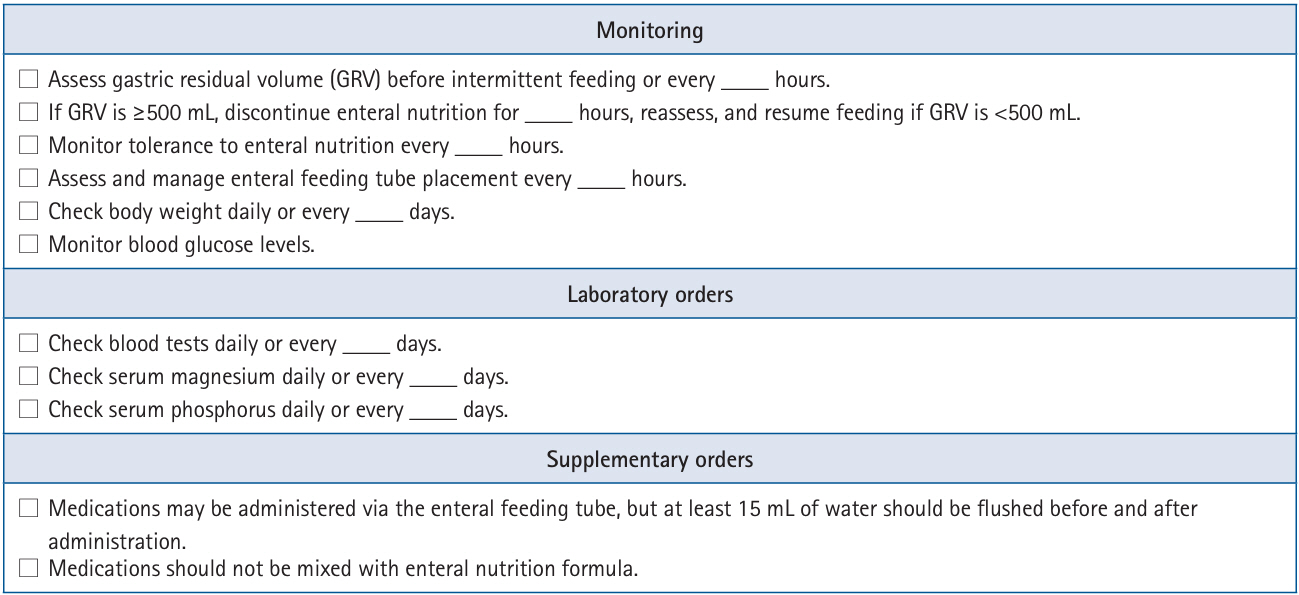
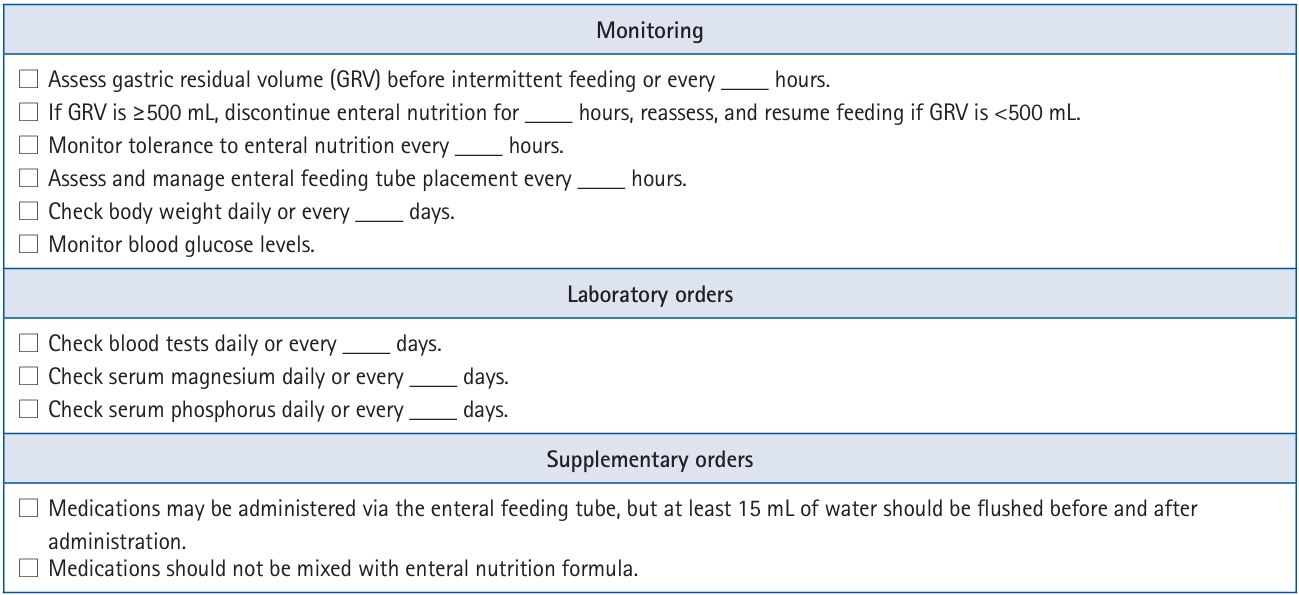
Results The practical guide recommends that EN orders include detailed elements and advocates the use of electronic medical records for communication. Standardized prescription forms and supplementary safety measures are outlined. Review frequency is adjusted according to patient condition—daily for critically ill or unstable patients and as dictated by institutional protocols for stable patients. Evidence indicates that adherence to these protocols reduces mortality, complications, and prescription errors.
-
Conclusion The KSPEN practical guide offers a robust framework for the safe delivery of EN tailored to Korea’s healthcare context. It emphasizes standardized protocols and interdisciplinary collaboration to improve nutritional outcomes, patient safety, and operational efficiency. Rigorous implementation and monitoring of adherence are critical for its success.
Introduction
Methodology
Practice guide
Practice recommendation
Rationale
Practice recommendation
Rationale
Practice recommendation
Rationale
Authors’ contribution
Conceptualization: all authors. Data curation: all authors. Formal analysis: all authors. Methodology: all authors. Project administration: all authors. Visualization: all authors. Funding acquisition: Not applicable. Writing – original draft: all authors. Writing – review & editing: all authors. All authors read and approved the final manuscript.
Conflict of interest
Ye Rim Chang has served as the editor of the Annals of Clinical Nutrition and Metabolism since 2024. However, she was not involved in the peer review process or decision-making regarding publication. Otherwise, no potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Not applicable.
Acknowledgments
We would like to express our sincere gratitude to the Korean Society for Parenteral and Enteral Nutrition (KSPEN) Guideline Committee members—In Gyu Kwon (Department of Surgery, Yonsei University Gangnam Severance Hospital, Seoul, Korea), Mina Kim (Department of Nursing, Inha University Hospital, Incheon, Korea), Bomi Kim (Department of Pharmacy, Seoul National University Hospital, Seoul, Korea), Seong Eun Kim (Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea), Jiyeon Kim (Department of Clinical Nutrition, National Cancer Center, Goyang, Korea), Ye Won Sung (Department of Pharmacy, Chungnam National University Hospital, Daejeon, Korea), Junghyun Yu (Nutritional Support Team, Yongin Severance Hospital, Yongin, Korea), Seung Hwan Lee (Department of Traumatology, Gachon University College of Medicine, Incheon, Korea), Jae Gil Lee (Department of Surgery, Ewha Womans University Mokdong Hospital, Seoul, Korea), Jee Young Lee (Department of Nursing, Kosin University Gospel Hospital, Busan, Korea), A Young Lim (Department of Clinical Nutrition, Seoul National University Bundang Hospital, Seongnam, Korea), Ji Yoon Cho (Department of Pharmacy, Daegu Fatima Hospital, Daegu, Korea)—for their invaluable contributions in reviewing and updating this practical guide for enteral nutrition.
Supplementary materials
None.
Correction
This article was corrected on November 13, 2025, to revise the article type.
- 1. Padar M, Uusvel G, Starkopf L, Starkopf J, Reintam Blaser A. Implementation of enteral feeding protocol in an intensive care unit: before-and-after study. World J Crit Care Med 2017;6:56-64. ArticlePubMedPMC
- 2. Kim SH, Park CM, Seo JM, Choi M, Lee DS, Chang DK, et al. The impact of implementation of an enteral feeding protocol on the improvement of enteral nutrition in critically ill adults. Asia Pac J Clin Nutr 2017;26:27-35. ArticlePubMed
- 3. Heyland DK, Cahill NE, Dhaliwal R, Sun X, Day AG, McClave SA. Impact of enteral feeding protocols on enteral nutrition delivery: results of a multicenter observational study. JPEN J Parenter Enteral Nutr 2010;34:675-84. ArticlePubMed
- 4. Roberts SR. Improving patient outcomes through registered dietitian order writing. Nutr Clin Pract 2013;28:556-65. ArticlePubMedPDF
- 5. Braga JM, Hunt A, Pope J, Molaison E. Implementation of dietitian recommendations for enteral nutrition results in improved outcomes. J Am Diet Assoc 2006;106:281-4. ArticlePubMed
- 6. Vanek VW. Providing nutrition support in the electronic health record era: the good, the bad, and the ugly. Nutr Clin Pract 2012;27:718-37. ArticlePubMed
- 7. Armada ER, Villamanan E, Lopez-de-Sa E, Rosillo S, Rey-Blas JR, Testillano ML, et al. Computerized physician order entry in the cardiac intensive care unit: effects on prescription errors and workflow conditions. J Crit Care 2014;29:188-93. ArticlePubMed
- 8. Heyland DK, Dhaliwal R, Lemieux M, Wang M, Day AG. Implementing the PEP uP protocol in critical care units in Canada: results of a multicenter, quality improvement study. JPEN J Parenter Enteral Nutr 2015;39:698-706. ArticlePubMed
- 9. Taylor B, Brody R, Denmark R, Southard R, Byham-Gray L. Improving enteral delivery through the adoption of the “Feed Early Enteral Diet adequately for Maximum Effect (FEED ME)” protocol in a surgical trauma ICU: a quality improvement review. Nutr Clin Pract 2014;29:639-48. ArticlePubMed
- 10. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159-211. ArticlePubMed
- 11. NSW Agency for Clinical Innovation. Guidelines for home enteral nutrition (HEN) services. 2nd ed. Agency for Clinical Innovation; 2012.
- 12. Bischoff SC, Austin P, Boeykens K, Chourdakis M, Cuerda C, Jonkers-Schuitema C, et al. ESPEN guideline on home enteral nutrition. Clin Nutr 2020;39:5-22. ArticlePubMed
References
Figure & Data
REFERENCES
Citations

- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
Suk-Kyung Hong
Ann Clin Nutr Metab.2025; 17(1): 1. CrossRef
- Figure
- Related articles
-
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN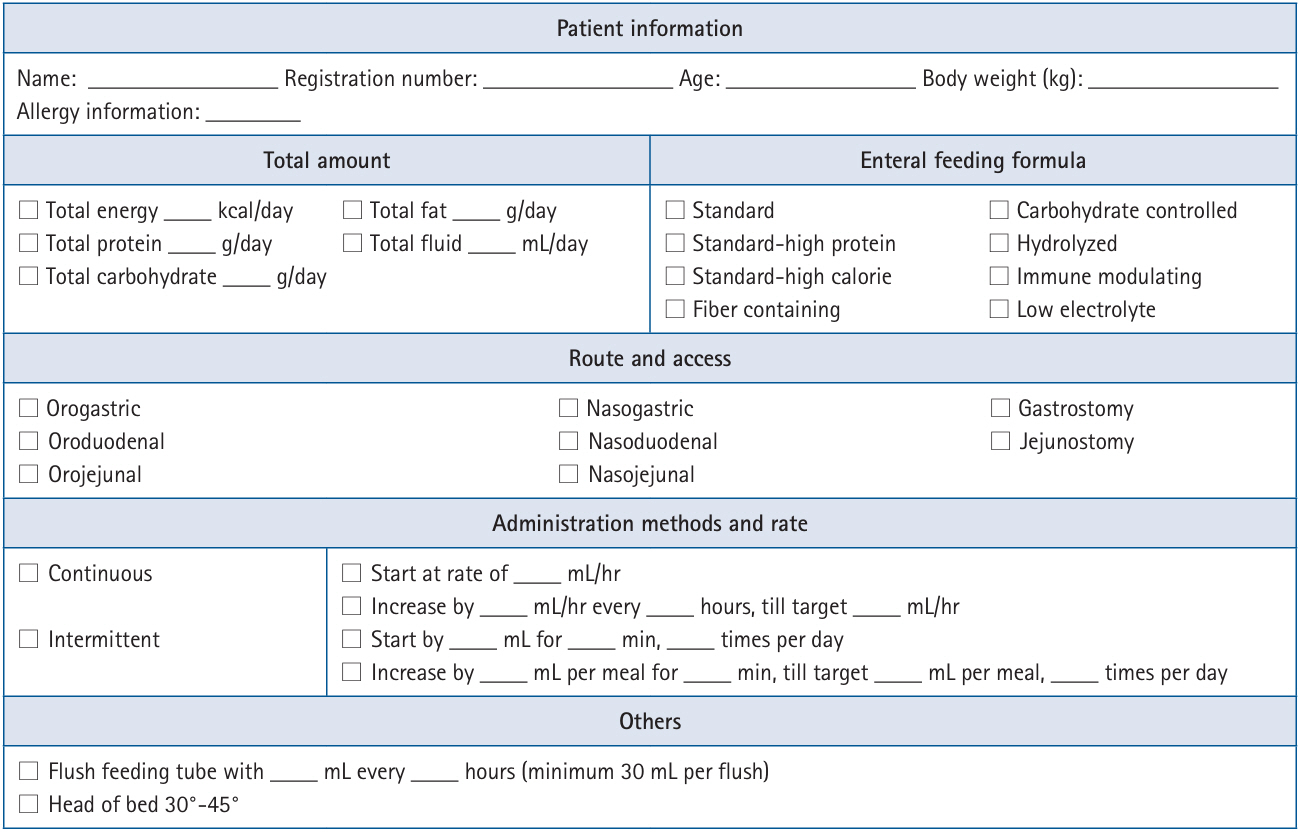
 Cite
Cite

