-
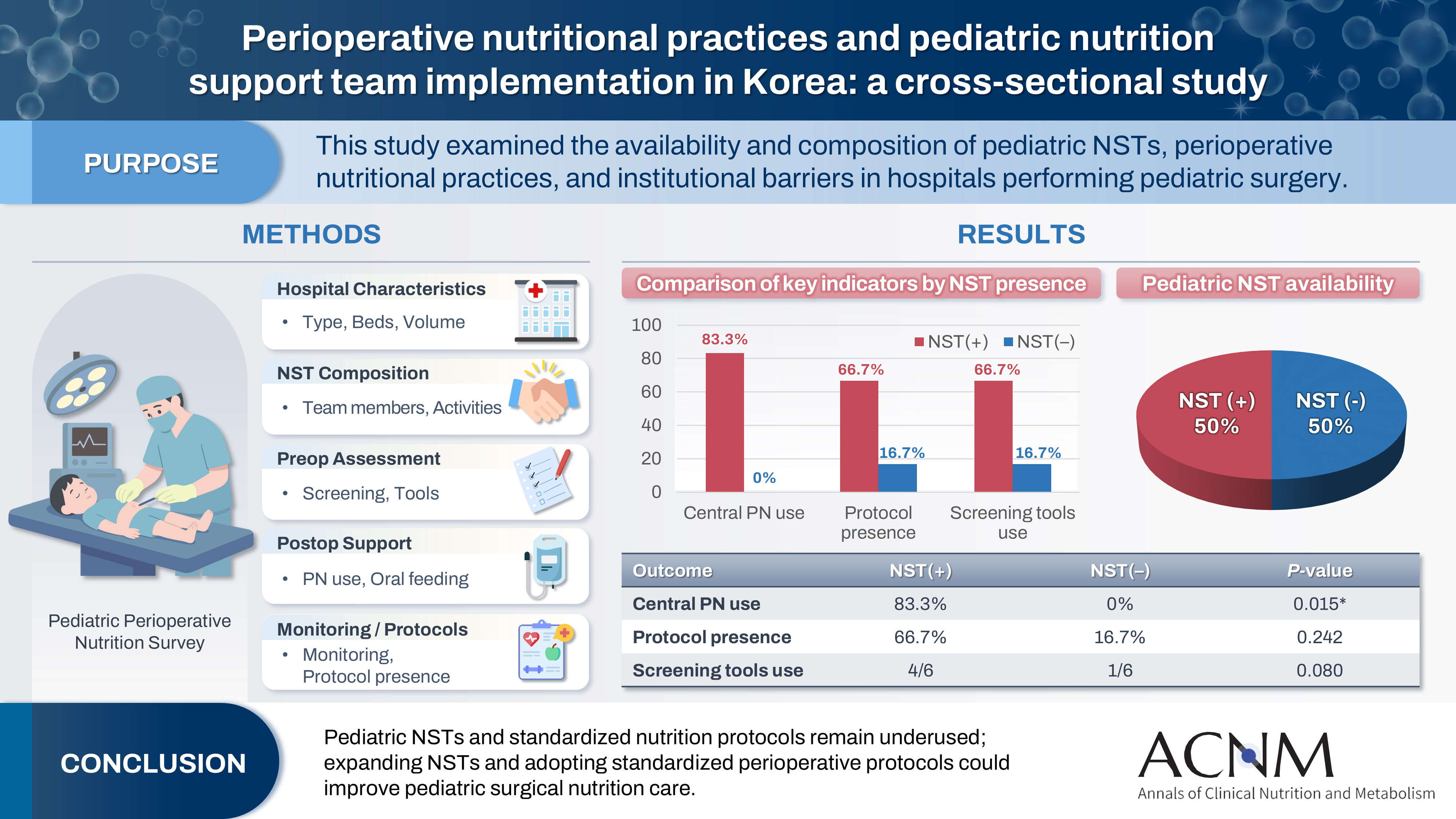
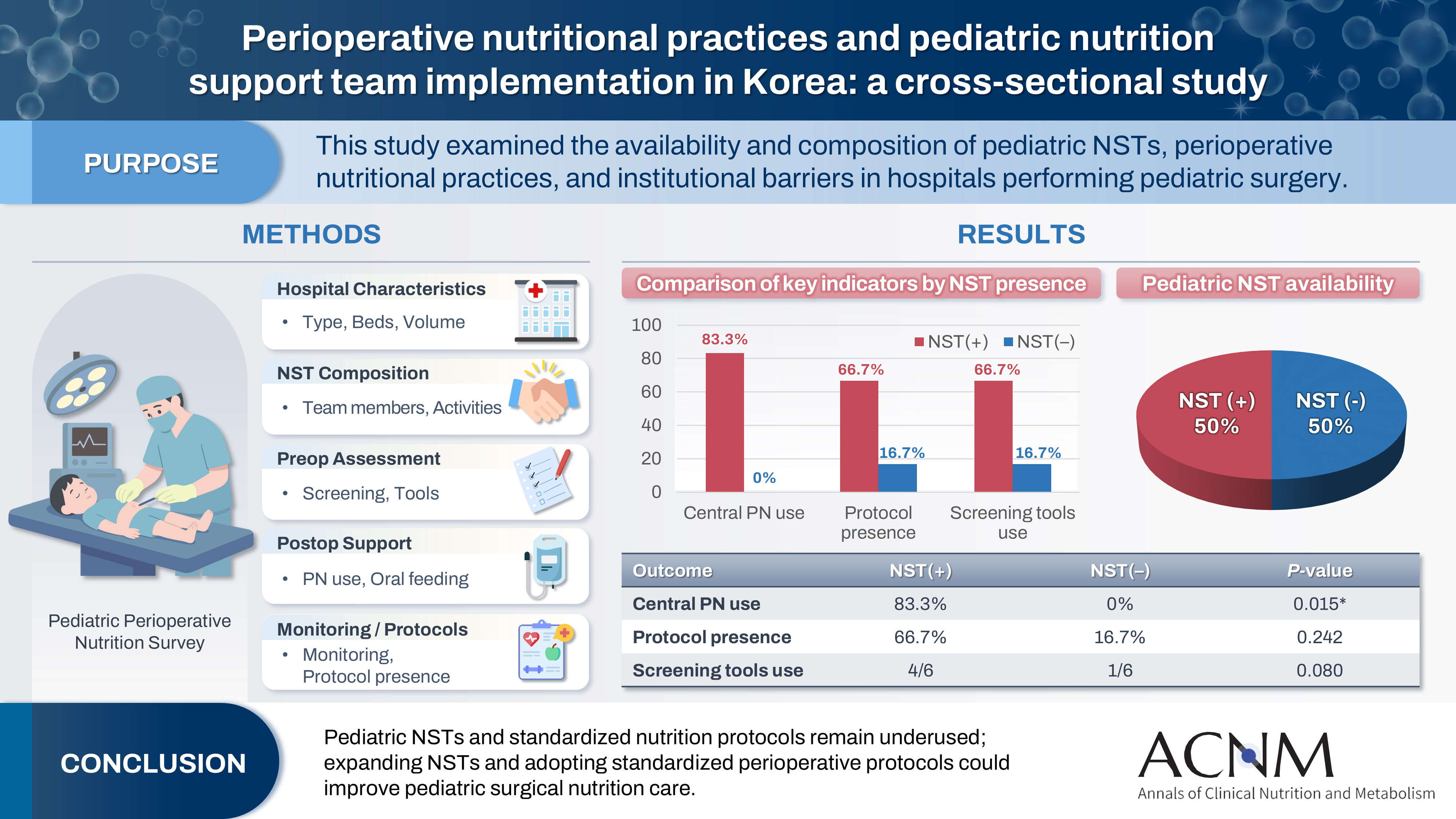
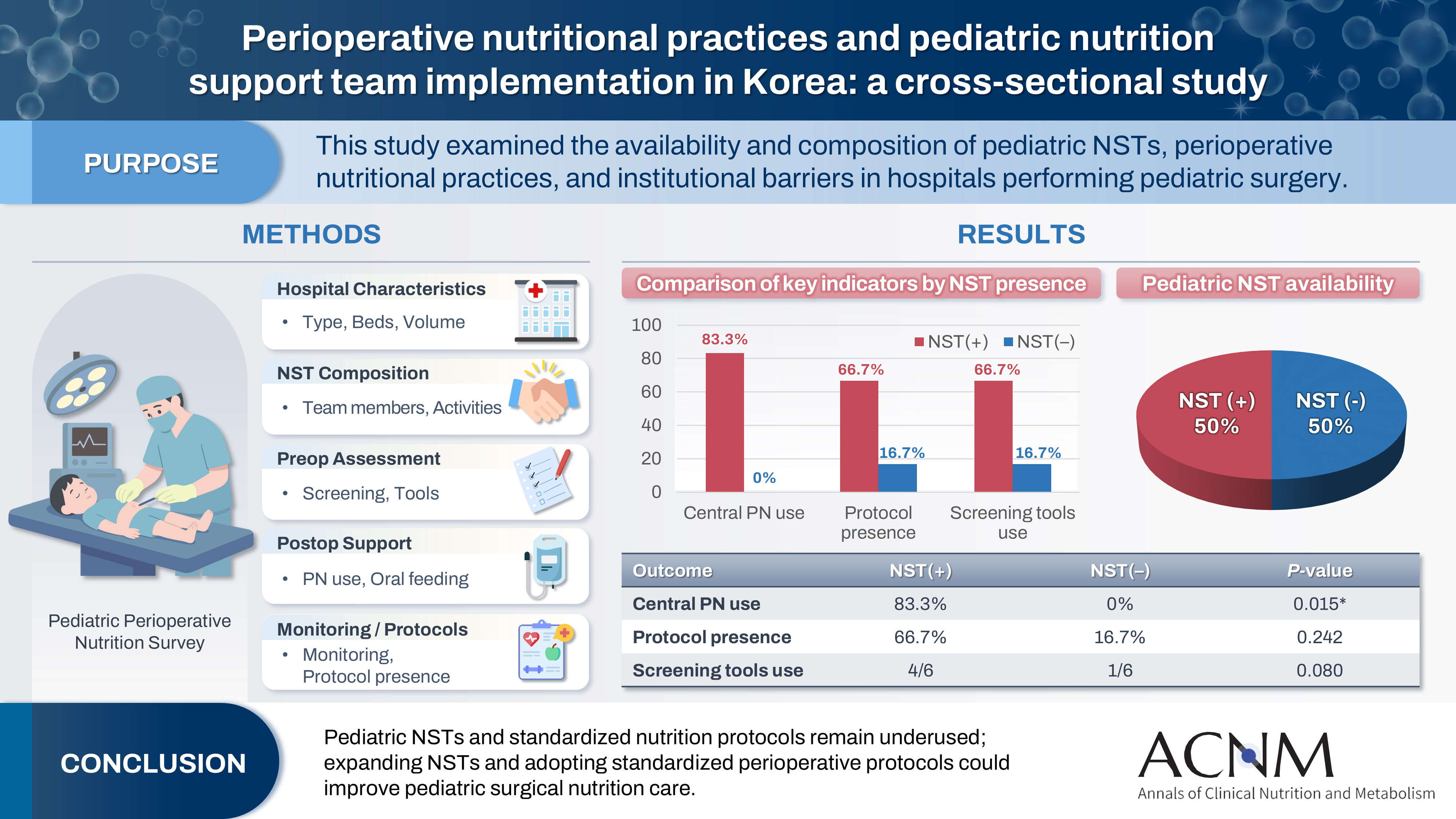
Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
-
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
-
Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
-
DOI: https://doi.org/10.15747/ACNM.25.0027
-
-
 Graphical Abstract Graphical Abstract
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material
 - Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
-
Nutritional Support for Pediatric Patients with Biliary Atresia
-
Joong Kee Youn, Ji-Young Song, Hyun-Young Kim
-
J Clin Nutr 2017;9(2):56-61. Published online December 31, 2017
-
DOI: https://doi.org/10.15747/jcn.2017.9.2.56
-
-
 Abstract Abstract
 PDF PDF
Biliary atresia (BA) is a major cause of extrahepatic biliary obstruction in children. Malnutrition is a significant clinical problem in children with BA. BA may induce the malabsorption of fat and fat-soluble vitamins, resulting in cholestasis and an impaired nutritional status. For the treatment of BA, it is most important to reconstruct the bile flow as early as possible by performing a Kasai portoenterostomy. After the Kasai operation, growth and nutrition are restored, but to follow normal growth and development, it is necessary to evaluate the nutritional status and support. Therefore, the purpose of nutritional support in children with BA is to normalize growth and development, prevent further liver damage and deterioration of the patient’s nutritional status, avoid vitamin and mineral deficiencies, and improve the quality of life of patients.
|