Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
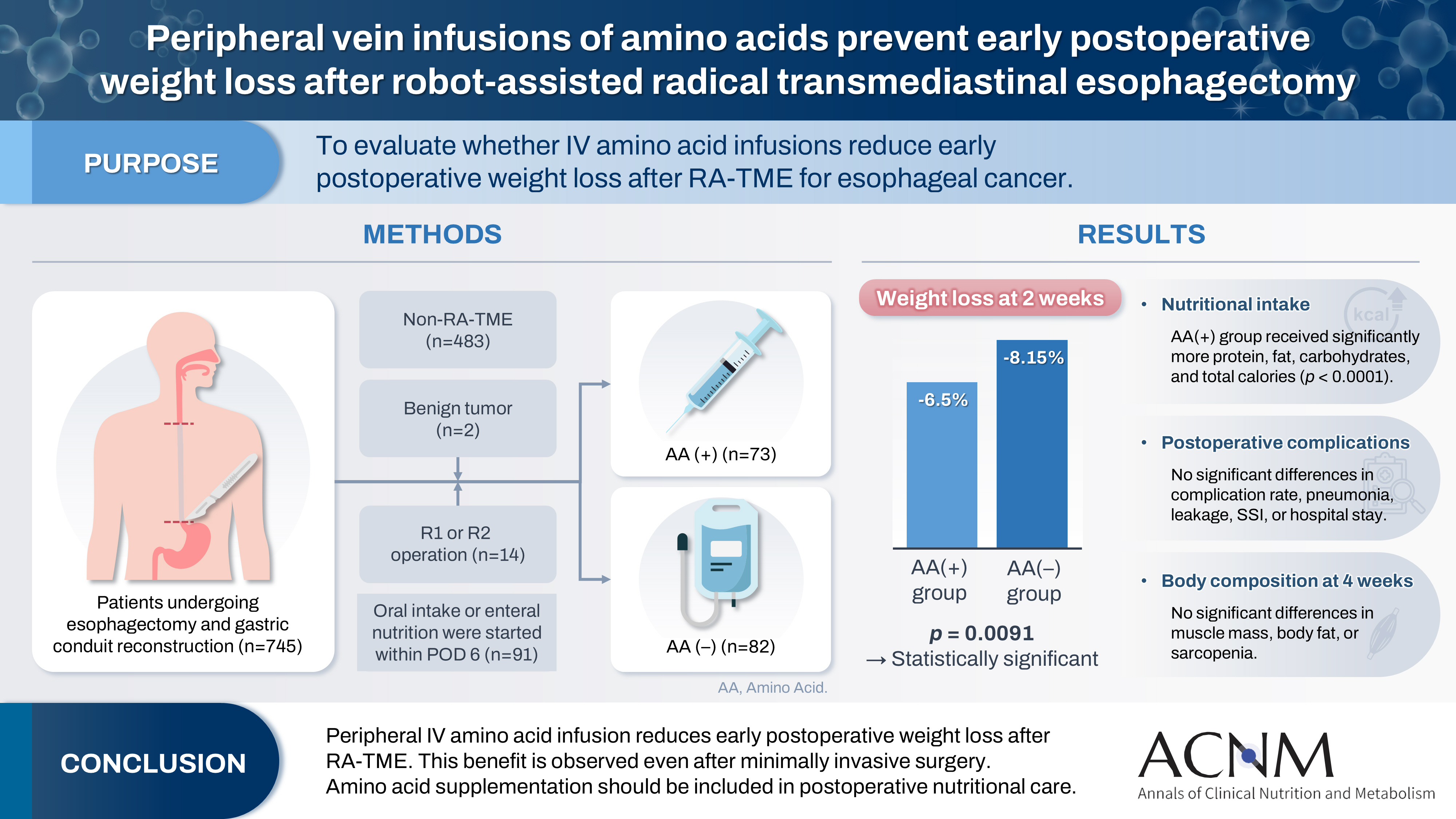
- Peripheral vein infusions of amino acids prevent early postoperative weight loss after robot-assisted radical transmediastinal esophagectomy: a retrospective study in Japan
- Tomonori Narita, Kazuhiko Fukatsu, Satoshi Murakoshi, Reo Inoue, Kenichi Kono, Midori Noguchi, Nana Matsumoto, Shoh Yajima, Koichi Yagi, Yoshifumi Baba
- Ann Clin Nutr Metab 2025;17(2):149-155. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0012
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 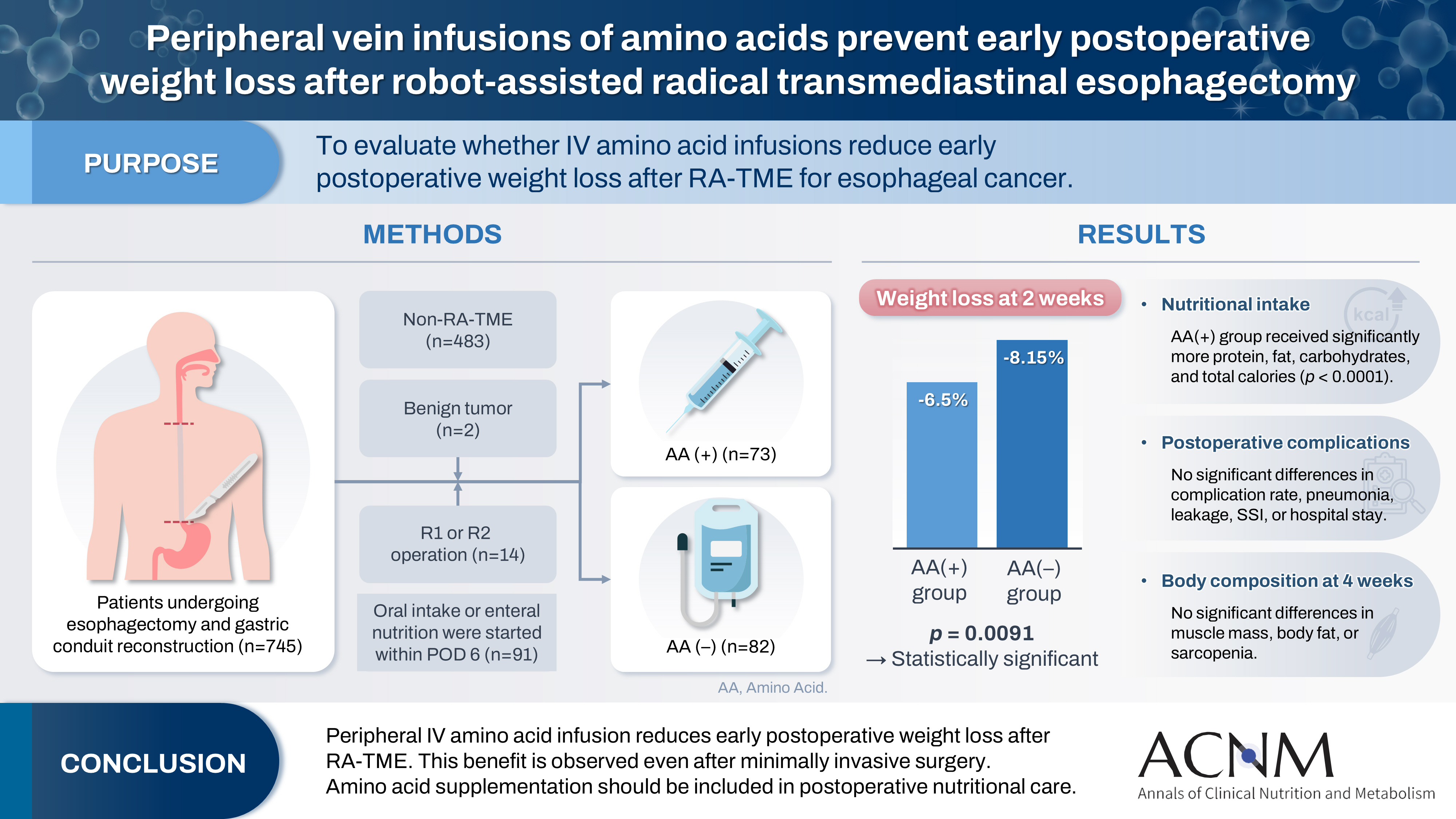
- Purpose
Postoperative body weight loss (PBWL) is linked to poor long-term outcomes following esophagectomy for esophageal cancer, making perioperative nutrition critically important. Although minimally invasive procedures such as robot-assisted radical transmediastinal esophagectomy (RA-TME) have become more prevalent, less attention has been paid to perioperative nutritional management. This study evaluates the impact of intravenous (IV) amino acid infusions on PBWL in patients undergoing RA-TME.
Methods
We retrospectively analyzed 155 patients who underwent RA-TME for esophageal or esophagogastric junction cancer at our hospital between 2011 and 2022. Patients were divided into two groups: AA(+) (n=73, received IV amino acids between postoperative days 1–6) and AA(–) (n=82, did not receive IV amino acids). Oral or enteral nutrition was withheld until postoperative day 6. We compared nutrient intake, postoperative outcomes, and nutritional status between groups.
Results
Patient backgrounds, surgical outcomes, and complication rates were similar in both groups. However, the AA(+) group received significantly greater energy and nutrient intake. PBWL at 2 weeks post-surgery was significantly lower in the AA(+) group than in the AA(–) group (6.50% vs. 8.15%, P=0.0091).
Conclusion
IV amino acid infusion may help mitigate early PBWL after RA-TME.
- 1,335 View
- 17 Download

- Association between decreased dietary intake during hospitalization and long-term weight loss in postoperative gastric cancer patients over 75 years of age: a retrospective cohort study
- Daiki Tabe, Isao Miyajima, Akira Tsukada
- Ann Clin Nutr Metab 2025;17(1):75-84. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0004
-
 Abstract
Abstract
 PDF
PDF - Purpose
Weight loss following gastrectomy is a significant concern, and maintaining adequate nutrition is necessary, especially given the growing number of older adult patients. This study examined the relationship between postoperative food intake and long-term weight loss in postgastrectomy patients aged ≥75 years.
Methods
Out of 88 patients who underwent gastrectomy for gastric cancer at our institute, 46 were aged ≥75 years. These patients were divided into two groups: one with an average energy intake exceeding 50% of the basal metabolic rate and one with an intake below 50% of the basal metabolic rate. The percentage change in body weight up to 6 months post-surgery was compared between the groups.
Results
In the group with higher dietary intake, the rate of weight change at 3 and 6 months postoperatively was lower, and fewer patients received postoperative adjuvant chemotherapy.
Conclusion
Poor postoperative food intake may serve as a predictor of weight loss up to 3 months following surgery in postgastrectomy patients aged ≥75 years. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,261 View
- 26 Download
- 1 Crossref

- Changes in perceptions of taste after bariatric surgery: a narrative review
- Young Suk Park
- Ann Clin Nutr Metab 2024;16(3):120-124. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.120
-
 Abstract
Abstract
 PDF
PDF - Purpose: Bariatric surgery effectively treats severe obesity, leading to significant weight loss and improved comorbidities. However, many patients experience postoperative alterations in taste perception, affecting food selection and eating behavior. This narrative review examines the current understanding of taste perception changes following bariatric surgery, including patterns, potential mechanisms, impact on weight loss outcomes, and implications for patient care.
Current concept: Changes in taste perception are frequently reported after bariatric procedures, with prevalence rates from 36% to 72%. Common alterations involve decreased preference and increased sensitivity to sweet and fatty tastes, potentially leading to reduced calorie intake and healthier food choices. Persistence of these changes varies and may depend on surgery type, with Roux-en-Y gastric bypass patients often experiencing more substantial effects than sleeve gastrectomy patients. Potential mechanisms include alterations in gut hormone secretion (e.g., GLP-1, peptide YY, ghrelin), modifications in neural pathways (e.g., vagus nerve), and shifts in the gut microbiome. These factors may collectively influence taste sensitivity and preferences, contributing to weight loss outcomes. Altered reward processing may reduce the appeal of high-calorie foods.
Conclusion: Alterations in taste perception are common after bariatric surgery and may significantly impact dietary behaviors, weight loss, and quality of life. While exact mechanisms are not fully understood, changes in gut hormones, neural pathways, and microbiota are likely involved. Patient counseling and postoperative management of bariatric surgery patients should address potential changes in taste. Further research is needed to elucidate the long-term impacts of taste alterations on weight-loss maintenance and nutritional status.
- 5,836 View
- 60 Download

- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
- Ji-Hyeon Park, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Jong Won Kim, Ki Bum Park, In Cho, Sun-Hwi Hwang, Dong-Wook Kim, Su Mi Kim, Seung-Wan Ryu, Seong Chan Gong, Pil Young Jung, Hoon Ryu, Sung Geun Kim, Chang In Choi, Dae-Hwan Kim, Sung-IL Choi, Ji-Ho Park, Dong Jin Park, Gyu-Yeol Kim, Yunhee Choi, Hyuk-Joon Lee
- Ann Clin Nutr Metab 2022;14(2):55-65. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.55
-
 Abstract
Abstract
 PDF
PDF - Purpose: To develop an individualized model for predicting the extent of unintentional weight loss following gastrectomy in patients with gastric cancer based on related risk factors and to externally validate this model using multicenter clinical data in Korea.
Materials and Methods: Among gastric cancer patients who underwent curative gastrectomy at 14 different gastric cancer centers, clinical data from patients with more than one weight measurement during the three-year follow-up period were retrospectively collected. Risk factors associated with weight loss in gastric cancer patients after gastrectomy were analyzed, and a predictive model was developed. Internal and external validation were performed.
Results: The data from 2,649 patients were divided into a derivation set (n=1,420 from Seoul National University Hospital) and validation set (n=1,229 from 13 different gastric cancers). Postoperative duration (six vs. 12, 24, or 36 months), sex (female vs. male), age, preoperative body mass index, type of surgery (pylorus-preserving vs. total, distal or proximal gastrectomy), and cancer stage (I vs. II or III) were included in the final prediction model. The model showed approximately 20% accuracy in predicting weight loss at each period: R2 at six, 12, 24 and 36 months after gastrectomy in internal validation=0.20, 0.21, 0.17, and 0.18, respectively, and in external validation=0.20, 0.22, 0.18, and 0.18, respectively. Calibration slopes of internal and external validation were 0.95 and 1.0, respectively.
Conclusion: Although predictive accuracy of the model did not reach an acceptable level, repeated external validation measurements showed high reliability. The model may serve as a basic reference in clinical practice. -
Citations
Citations to this article as recorded by- Development and Feasibility Assessment of Mobile Application-Based Digital Therapeutics for Postoperative Supportive Care in Gastric Cancer Patients Following Gastrectomy
Ji-Hyeon Park, Hyuk-Joon Lee, JeeSun Kim, Yo-Seok Cho, Sunjoo Lee, Seongmin Park, Hwinyeong Choe, Eunhwa Song, Youngran Kim, Seong-Ho Kong, Do Joong Park, Byung-Ho Nam, Han-Kwang Yang
Journal of Gastric Cancer.2024; 24(4): 420. CrossRef
- Development and Feasibility Assessment of Mobile Application-Based Digital Therapeutics for Postoperative Supportive Care in Gastric Cancer Patients Following Gastrectomy
- 2,677 View
- 22 Download
- 1 Crossref

- Postoperative Weight Changes, Nutritional Status and Clinical Significance of Colorectal Cancer Patients
- Sun Young Kim, Ji Sun Kim, Eon Chul Han
- Surg Metab Nutr 2019;10(2):46-53. Published online December 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.2.46
-
 Abstract
Abstract
 PDF
PDF Purpose:
Although weight loss is an important factor for assessing the nutritional status, patient counselling or management is limited due to fewer studies on weight loss after colorectal cancer surgery.
Materials and Methods:
Totally, 374 patients were included in the analysis (between August 2010 to December 2016). Patients’ weight was determined before surgery, and at 1 week, 6 weeks, 3 months, and 6 months after surgery. Change in weight was reviewed based on the gender and administration of chemotherapy. Severe weight loss is defined as greater than 5% weight loss after surgery.
Results:
The weight changes post-surgery at 1 week (−2.56±2.62 vs. −3.36±2.68, P<0.005), 6 weeks (−3.23±3.82 vs. −4.57±3.96, P=0.001), and 3 months (−0.93±5.01 vs. −2.79±4.86, P<0.001) were significantly greater in male subjects, as compared to female patients. However, at 6 months post-surgery, most patients showed weight gain with no statistical significance between the genders (1.11±4.64 vs. 1.94±6.26, P=0.143). Weight change based on treatment (with or without chemotherapy) reveal significant differences between the genders at 3 months post-surgery only (−1.33±4.65 vs. −2.52 ±5.15, P=0.027). Multivariate analysis for factors of severe weight loss show that the male gender [adjusted odds ratio (OR): 1.83, P=0.027)], adjuvant chemotherapy (adjusted OR 2.11, P=0.008), and presence of post-operative complications (adjusted OR 2.12, P=0.029) were significant factors.
Conclusion:
In postoperative colorectal cancer patients, the weight and nutritional status require careful monitoring for at least 2 months after surgery, in order to prevent hindrance to chemotherapy. (Surg Metab Nutr 2019;10:-53)
-
Citations
Citations to this article as recorded by- The impact of pre‐surgery nutrition intervention on weight loss, nutrition status, and quality of life in colorectal cancer patients with elective surgery
Wen Lynn Teong, Wei Yee Wong, Su Lin Lim, Choon Hui Low, Cassandra Lim Duan Qi, Ruochen Du
Malignancy Spectrum.2025; 2(2): 74. CrossRef - Serial measurements of body composition using bioelectrical impedance and clinical usefulness of phase angle in colorectal cancer
Seung‐Rim Han, Jung Hoon Bae, Chul Seung Lee, Abdullah Al‐Sawat, Soo Ji Park, Hyo Jin Lee, Mi Ran Yoon, Hyeong Yong Jin, Yoon Suk Lee, Do Sang Lee, In Kyu Lee
Nutrition in Clinical Practice.2022; 37(1): 153. CrossRef
- The impact of pre‐surgery nutrition intervention on weight loss, nutrition status, and quality of life in colorectal cancer patients with elective surgery
- 2,321 View
- 14 Download
- 2 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


