Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Articles
- Page Path
- HOME > J Clin Nutr > Volume 10(1); 2018 > Article
- Case Report Esophageal Obstruction Caused by the Solidification of Residue of an Enteral Feeding Formula
- Hancheol Jo1, Ye Rim Chang1, So Mi Kim2, Dong Wook Kim1, Ye Seob Jee1
- 소화관영양처방의 잔류물의 고형화에 의해 발생된 식도막힘
- 조한철1, 장예림1, 김소미2, 김동욱1, 지예섭1
-
Journal of the Korean Society for Parenteral and Enteral Nutrition 2018;10(1):25-30.
DOI: https://doi.org/10.15747/jcn.2018.10.1.25
Published online: June 30, 2018
Departments of Surgery
Internal Medicine, Dankook University Hospital, Cheonan, Korea
- Correspondence to Ye Seob Jee Department of Surgery, Dankook University Hospital, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea Tel: +82-41-550-6379, Fax: +82-41-550-0524, E-mail: ysjee77@gmail.com
• Received: December 28, 2017 • Revised: May 18, 2018 • Accepted: May 20, 2018
Copyright: © Korean Society for Parenteral and Enteral Nutrition
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,676 Views
- 2 Download
- 1 Crossref
Abstract
- The nutritional support of acutely ill patients is very important and early enteral nutrition is recommended. Feeding via the nasogastric route is used widely for its ease of access if the patient cannot maintain volitional food intake. If the position of the tip or side holes of the nasogastric tube (NGT) is above the gastroesophageal junction, there is the possibility of retention and solidification of the administered enteral feeding formula in the esophagus. Therefore, the tip of the NGT should be checked carefully; a chest radiograph to confirm its position can be considered, especially in patients with a higher risk of aspiration and gastroesophageal reflux. In addition, careful consideration of the risk factors that can trigger esophageal obstruction is required when feeding patients in the intensive care unit. This paper describes two unusual cases of esophageal obstruction caused by the solidification of residue of an enteral feeding formula.
INTRODUCTION
The nutritional support of acute ill patients is very important and early enteral nutrition (EN) is recommended to maintain gut integrity and attenuate disease severity.1 Feeding via the nasogastric route is widely used for its ease of access if the patient cannot maintain volitional food intake. Recently, tubes for nasogastric feeding have been developed and used; however, Levin tubes, which have been designed for drainage of gastric contents, have been widely used in particular. Levin tubes have multiple side holes within 20 cm of the tip of the tube, so even if the tip is located in the stomach, the feeding formula can be delivered to the esophagus through the side holes. Herein, we report two cases of esophageal obstruction caused by malpositioned feeding tubes.
CASE REPORT
An 87-year-old female was transferred to the intensive care unit (ICU) from a local hospital with a diagnosis of acute cholecystitis. She developed pain in the right upper quadrant while undergoing treatment for pneumonia 4 days prior to her transfer to the ICU. She had no specific past medical history.
She was intubated and mechanically ventilated due to exacerbation of the pneumonia and developed a parapneumonic pleural effusion the next day, during the treatment of acute cholecystitis. After she was hemodynamically stabilized on the 3rd day following her ICU admission, a Levin tube (size 14, French gauge) was inserted and continuous enteral feeding of a formula called Harmonilan® (Nutrichem Diät + Pharma GmbH, Roth, Germany) was administered at an infusion rate of 480 mL per day. Additionally, oral medication via the tube (powdered losartan and furosemide) was administered. The assigned doctor confirmed the position of the Levin tube by auscultation.
Her clinical course gradually improved with intravenous (IV) antibiotic administration and percutaneous drainage of the pleural effusion. Initially, we administered ceftriaxone and metronidazole with a focus on treating the acute cholecystitis. Subsequently, the antibiotics were changed from ceftriaxone to meropenem for treatment of biliary sepsis on the second hospital day, and on the 20th hospital day, they were changed to piperacillin/tazobactam and gemifloxacin to focus more on treating the pneumonia. IV pantoprazole and metoclopramide had been administered since her initial hospitalization. She was weaned off the mechanical ventilator on the 8th hospital day and was transferred to the general ward on the 22nd hospital day with nasal continuous positive airway pressure therapy.
Continuous enteral feeding via the Levin tube proceeded and was gradually increased to 960 mL per day. She defecated on the 16th hospital day for the first time since being hospitalized. Subsequently, she had loose stool but no diarrhea.
After a month of treatment, her Levin tube got occluded and was removed for replacement, but insertion of a new Levin tube failed repeatedly. Insertion of the Levin tube under guidance of gastrofiberoscopy was attempted, but it also failed. Obstruction of the esophagus due to solidification of residual enteral feeding formula material at the level of 20 cm from the upper incisors was noted (Fig. 1A).
Fig. 1
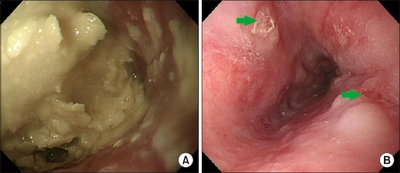
(A) Esophageal obstruction due to enteral feeding formula. (B) After pushing the formula downward, a shallow ulcer of the distal esophagus was noted (arrows).
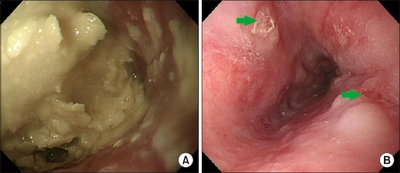
A gastroenterology physician was consulted and the bezoar was pushed downward to the stomach with a gastrofiberscope. After the whole bezoar was completely removed from the esophageal lumen (requiring about 11 minutes), shallow ulcers of the esophageal mucosa were observed (Fig. 1B). The esophageal mucosal ulcers were treated with IV esomeprazole. A new Levin tube was reinserted under guidance of a gastrofiberscope and continuous enteral feeding via the Levin tube resumed the next day with another feeding formula called Encover® (EN Otsuka Pharmaceutical Co., Hanamaki, Japan), without intolerance.
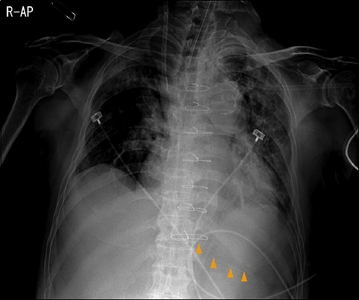
During a retrospective review of serial chest radiographs, we found that the tip of the Levin tube had been malpositioned above the gastroesophageal junction (GEJ) instead of inside the stomach (Fig. 2). The position of the newly inserted Levin tube was confirmed by the assigned physician using chest radiograph, and enteral feeding continued without complication.
The patient was scheduled to undergo elective cholecystectomy; however, her clinical course worsened due to relapsing pneumonia. She expired on the 71st day of her hospitalization.
A 68-year-old male complaining of severe chest pain was transferred to the ICU from a local hospital with a diagnosis of ascending aortic pseudoaneurysm. He had a past medical history of diabetes mellitus, left temporal cerebral infarction, right upper lobectomy due to lung cancer at another hospital one year prior to this hospitalization, and received an endovascular stent of the right common carotid artery and left subclavian artery two months prior to hospitalization.
On the second hospital day, he underwent ascending aorta replacement surgery with an artificial graft. IV cefbuperazone and IV pantoprazole were administered, and continuous IV injections of nitroglycerin, labetalol (for control of blood pressure), regular insulin (for control of blood glucose level), and furosemide (for proper fluid balance) were also administered.
Because he did not respond to pain stimulation and his mental status did not improve after cessation of sedatives on the first postoperative day (POD), magnetic resonance imaging of the brain was performed, and a neurologist diagnosed him as having acute multiple cerebral infarctions. We added a continuous injection of IV heparin to prevent further aggravation of the cerebral infarctions.
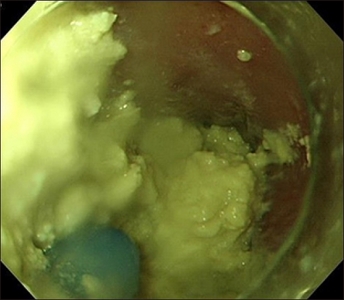
On the fourth POD, he was still receiving mechanical ventilation therapy. On that day, a Levin tube was inserted, and its placement was confirmed with auscultation. Continuous enteral feeding with Harmonilan® was initiated with an infusion rate of 480 mL per day, and it was gradually increased to 960 mL per day. Administration of oral medication (levosulpiride) via the tube ensued, until the Levin tube occluded on the 12th POD. He had not defecated since his hospitalization. The assigned doctor attempted reinsertion of the Levin tube but failed repeatedly. On the next day, gastrofiberoscopy was performed for evaluation of the esophagus and insertion of the Levin tube, but esophageal obstruction due to solidification of residual enteral feeding formula was noted (Fig. 3).
A gastroenterology physician was consulted, and again the bezoar was pushed downward to the stomach using a gastrofiberscope (requiring about 18 minutes). A new Levin tube was reinserted under the guidance of a gastrofiberscope and continuous enteral feeding with another feeding formula called Greenbia DM solution® (Dr. Chung’s Food, Cheongju, Republic of Korea) via the Levin tube was resumed on the next day. The position of the newly inserted Levin tube was confirmed by the assigned physician with chest radiograph, and enteral feeding continued, without any sign of intolerance. The infusion rate of the feeding was increased up to 1,440 mL per day.
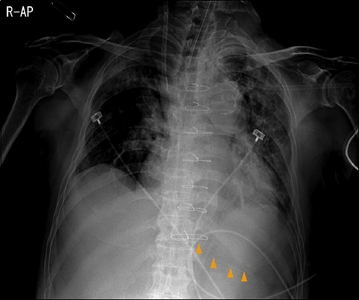
In this patient, the tip of the former Levin tube had been positioned in the stomach, as noted in a retrospective review of chest radiographs. However, the portion of the tube that reached inside the stomach was about 15 cm in length (Fig. 4). Therefore, it is reasonable to assume that some of the side holes of the tube were located above the GEJ.
Fig. 4
The tip of the Levin tube located in the stomach (arrowheads), but the portion of the tube inside the stomach was about 15 cm.
The patient had no complication associated with the ascending aorta replacement surgery, but as the cerebral infarction condition became chronic, the patient had a tracheostomy placed on the 15th POD. He was bedridden for about six months in ICU, and finally was transferred to a local hospital without significant improvement.
DISCUSSION
In most cases reporting esophageal obstruction caused by solidification of residual enteral feeding formula, Levin tubes were used and the position of the tip was not confirmed radiographically (Table 1).2-4 For example, Tawfic et al.2 reported a patient who suffered esophageal obstruction by bezoar from an enteral feeding formula. In that case, the malpositioning of the nasogastric tube (NGT) in the esophagus was confirmed, leading to an accumulation of the formula in the distal esophagus, which subsequently solidified. Tawfic et al.2 suggested that a major mistake was the failure to use a radiograph or a second method to confirm the correct position of the NGT. By radiographically confirming the location of the tip, it is possible to prevent esophageal obstruction.
Table 1
Overview of the esophageal obstruction cases
| Age/sex | Medical condition | Enteral access | Malposition of tube tip | Treatment | Result | |
|---|---|---|---|---|---|---|
| Case 1 | 87/F | Acute cholecystitis, pneumonia | Levin tube (14 Fr) | Yes | Endoscopy | Successful clearing of esophagus |
| Case 2 | 68/M | Ascending aorta pseudoaneurysm, diabetes mellitus, left temporal cerebral infarction | Levin tube (14 Fr) | Yes | Endoscopy | Successful clearing of esophagus |
| Tawfic et al.2 | 20/M | Meningoencephalitis | NGT (14 Fr) | Yes | Endoscopy with sodium bicarbonate solution | Successful clearing of esophagus |
| Marcus et al.3 | 80/F | Vascular dementia, chronic heart failure, diabetes mellitus, hypothyroidism | NGT (size unavailable) | No | Endoscopy | Successful clearing of esophagus |
| Degheili et al.4 | 69/M | Myocardial infarction, anoxic brain injury | NGT (size unavailable) | No | Feeding jejunostomy | Unavailable |
Some case reports assume that the cause of solidification is the interaction of the casein component of the feeding formula with the acidic pH of the gastric juice. In a case report by Turner et al.,5 an enteral feeding formula containing a casein component was administered, which resulted in esophageal obstruction. Since the formula containing dried skim milk instead of casein, which does not induce solidification even at a pH below one, Turner et al.5 suggested using a formula that does not contain casein and administering acid-lowering medications. Gupta et al.6 recommended administering pancreatic enzyme extract because it can prevent and liquefy the solidification of casein-containing formula. However, because Harmonilan® does not contain casein, it is unknown which component caused solidification in the two aforementioned cases.
Since gastroesophageal reflux (GER) can increase the risk of esophageal obstruction during EN, it is recommended that risk for GER should be identified and decreased by maintaining elevation of the head of bed, and administering prokinetics and/or proton pump inhibitors.3 Douzinas et al.7 reported that GER became worse with a longer duration of NGT feeding in mechanically ventilated patients because NGT feeding causes mechanical irritation of the esophagus and relaxation of the lower esophageal sphincter. In addition, percutaneous gastrostomy and semi-recumbent positioning should be considered to lower the risk of GER.8
More attention should be given to ICU patients receiving enteral feeding via an NGT. Degheili et al.4 reported a case of esophageal obstruction due to a bezoar from a casein-based feeding formula and suggested risk factors that predispose patients to gastrointestinal (GI) bezoars may include delayed gastric emptying, supine positioning, reduction in gastric acidity, history of previous gastric surgeries, peptic ulcer disease, achalasia, GI malignancies, Crohn’s disease, hypothyroidism, presence of hiatal hernia, and neuropathic or myotonic dystrophy. They also suggested that a multidisciplinary team approach is required for the estimation of the risk of GI obstruction from bezoar when providing ICU patients with enteral feeding. In a retrospective study of esophageal bezoar by Caldeira et al.,9 there were 9 patients who were diagnosed with esophageal bezoar across the span of three years in 1,003 patients (0.9%) who received enteral feeding. The mean duration of enteral feeding was 12 days, and all these cases involved patients who were mechanically ventilated. So the duration of enteral feeding of mechanically ventilated patients can be a clue as to which patients should be given more attention.
The NGT used for feeding in these two cases was a Levin tube with multiple side holes within 20 cm of the tip, which allows for drainage of gastric contents. Compared with an NGT designed only for feeding and made of polyurethane, a Levin tube is made of silicone and usually has a smaller inner diameter compared to that of a polyurethane tube. In the first case, the tip of the NGT was located in the esophagus. In the second case, the tip of the NGT was located in the stomach, but the distance from the GEJ to the tip of the tube was inadequate and some of the side holes might have been located in the esophagus. It is reasonable to assume that total or part of the administered feeding formula was retained in the esophagus and thus solidification occurred; additionally, the reflux of gastric contents with an acidic pH may have triggered the solidification. In the first case, the patient did not have a significant past medical history, but she received mechanical ventilation due to pneumonia. In the second case, the patient had a past medical history of diabetes mellitus and was diagnosed with acute cerebral infarction, which may alter the motility of the esophageal sphincter and cause retention of the enteral formula.10 Listed risk factors related to the patients in these two cases might have resulted in the esophageal obstruction observed in these two cases.
In conclusion, feeding tubes that are designed solely for feeding rather than drainage should be used to prevent esophageal obstruction due to enteral formula. The tube should be carefully inserted and checked radiographically to be sure that all side holes are located within the stomach. Risk factors for esophageal obstruction due to bezoar formation should be identified and minimized. Lastly, if a patient is expected to receive enteral feeding for an extended duration, casein-based formulas should be avoided, if possible.
- 1. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient:Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40(2):159-211. PubMed
- 2. Tawfic QA, Bhakta P, Date RR, Sharma PK. Esophageal bezoar formation due to solidification of enteral feed administered through a malpositioned nasogastric tube:case report and review of the literature. Acta Anaesthesiol Taiwan 2012;50(4):188-90. ArticlePubMed
- 3. Marcus EL, Arnon R, Sheynkman A, Caine YG, Lysy J. Esophageal obstruction due to enteral feed bezoar:a case report and literature review. World J Gastrointest Endosc 2010;2(10):352-6. ArticlePubMedPMC
- 4. Degheili JA, Sebaaly MG, Hallal AH. Nasogastric tube feeding-induced esophageal bezoar:case description. Case Rep Med 2017;doi:10.1155/2017/1365736. [Epub ahead of print]. ArticlePDF
- 5. Turner JS, Fyfe AR, Kaplan DK, Wardlaw AJ. Oesophageal obstruction during nasogastric feeding. Intensive Care Med 1991;17(5):302-3. ArticlePubMedPDF
- 6. Gupta R, Share M, Pineau BC. Dissolution of an esophageal bezoar with pancreatic enzyme extract. Gastrointest Endosc 2001;54(1):96-9. ArticlePubMed
- 7. Douzinas EE, Tsapalos A, Dimitrakopoulos A, Diamanti- Kandarakis E, Rapidis AD, Roussos C. Effect of percutaneous endoscopic gastrostomy on gastro-esophageal reflux in mechanically-ventilated patients. World J Gastroenterol 2006;12(1):114-8. ArticlePubMedPMC
- 8. Ibáñez J, Peñafiel A, Raurich JM, Marse P, Jordá R, Mata F. Gastroesophageal reflux in intubated patients receiving enteral nutrition:effect of supine and semirecumbent positions. JPEN J Parenter Enteral Nutr 1992;16(5):419-22. ArticlePubMed
- 9. Caldeira A, Casanova P, Sousa R, Martins P, Banhudo A, Pimentel J. Enteric nutrition and esophageal impactation:what relationship. Acta Med Port 2010;23(2):183-90. PubMed
- 10. Wang X, Pitchumoni CS, Chandrarana K, Shah N. Increased prevalence of symptoms of gastroesophageal reflux diseases in type 2 diabetics with neuropathy. World J Gastroenterol 2008;14(5):709-12. ArticlePubMedPMC
References
Figure & Data
REFERENCES
Citations
Citations to this article as recorded by 

- Body Composition and Physical Performance Measures of a Special Operations Police Unit: Characteristics and Associations Between Determinant Factors of Physical Performance
Braian Fink, Tomás T. Freitas, Santiago Zabaloy
Journal of Science in Sport and Exercise.2024; 6(1): 61. CrossRef
Esophageal Obstruction Caused by the Solidification of Residue of an Enteral Feeding Formula
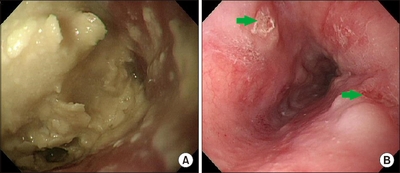
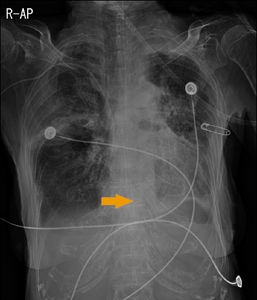
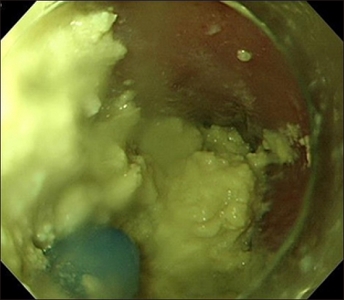
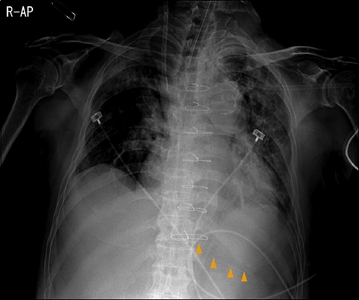
Fig. 1
(A) Esophageal obstruction due to enteral feeding formula. (B) After pushing the formula downward, a shallow ulcer of the distal esophagus was noted (arrows).
Fig. 2
The tip of the Levin tube located in the distal esophagus (arrow).
Fig. 3
Esophageal obstruction due to enteral feeding formula.
Fig. 4
The tip of the Levin tube located in the stomach (arrowheads), but the portion of the tube inside the stomach was about 15 cm.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Esophageal Obstruction Caused by the Solidification of Residue of an Enteral Feeding Formula
Overview of the esophageal obstruction cases
| Age/sex | Medical condition | Enteral access | Malposition of tube tip | Treatment | Result | |
|---|---|---|---|---|---|---|
| Case 1 | 87/F | Acute cholecystitis, pneumonia | Levin tube (14 Fr) | Yes | Endoscopy | Successful clearing of esophagus |
| Case 2 | 68/M | Ascending aorta pseudoaneurysm, diabetes mellitus, left temporal cerebral infarction | Levin tube (14 Fr) | Yes | Endoscopy | Successful clearing of esophagus |
| Tawfic et al.2 | 20/M | Meningoencephalitis | NGT (14 Fr) | Yes | Endoscopy with sodium bicarbonate solution | Successful clearing of esophagus |
| Marcus et al.3 | 80/F | Vascular dementia, chronic heart failure, diabetes mellitus, hypothyroidism | NGT (size unavailable) | No | Endoscopy | Successful clearing of esophagus |
| Degheili et al.4 | 69/M | Myocardial infarction, anoxic brain injury | NGT (size unavailable) | No | Feeding jejunostomy | Unavailable |
F = female; M = male; NGT = nasogastric tube.
Table 1 Overview of the esophageal obstruction cases
F = female; M = male; NGT = nasogastric tube.

 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN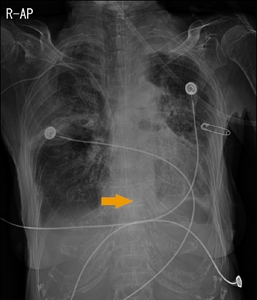
 Cite
Cite

