Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
Original Article
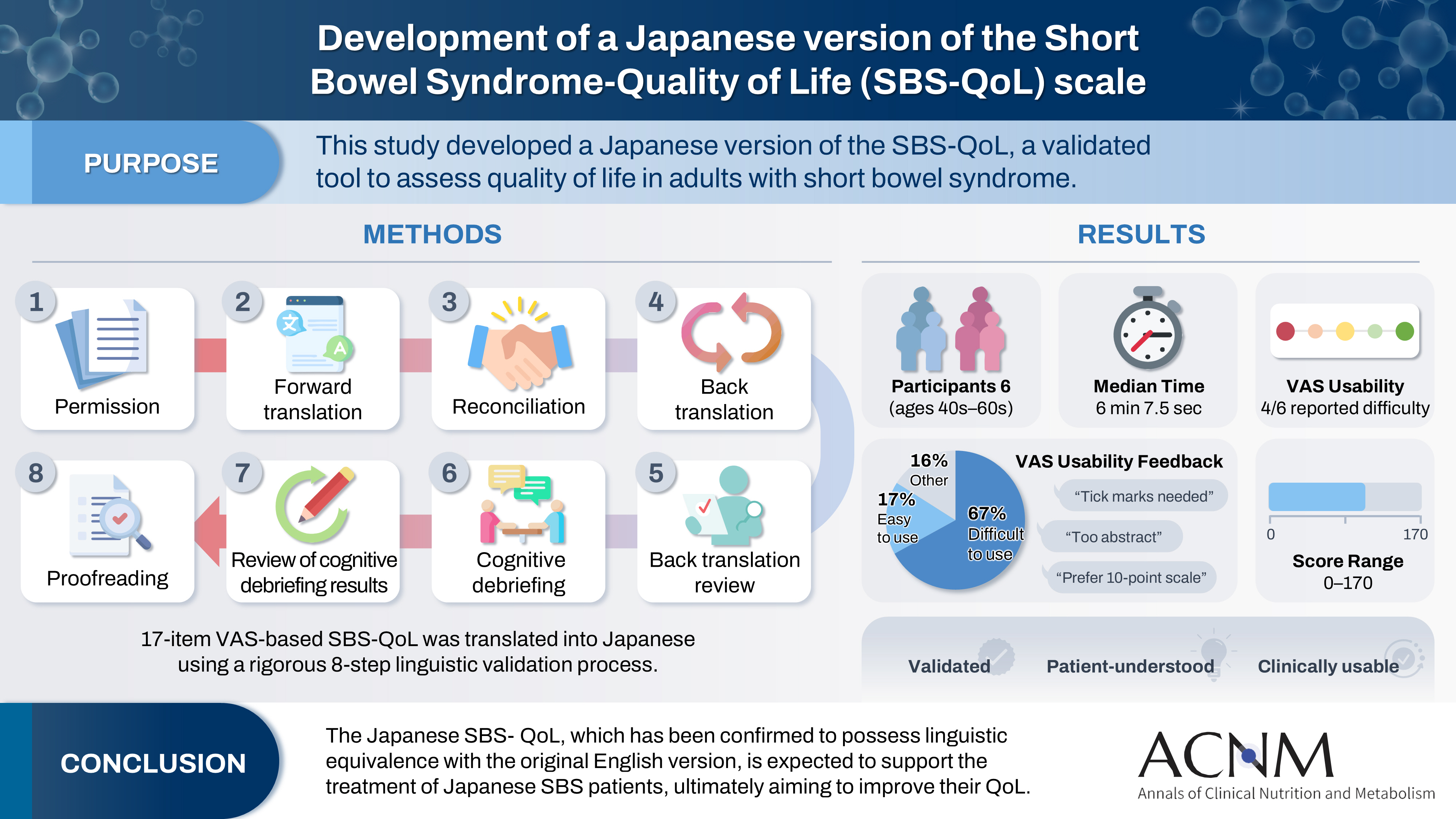
- Development of a Japanese version of the Short Bowel Syndrome-Quality of Life (SBS-QoL) scale
- Yuko Tazuke, Mayu Suzuki, Sae Kikuchi, Kaori Ishiguro, Hiroomi Okuyama
- Ann Clin Nutr Metab 2025;17(2):132-138. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 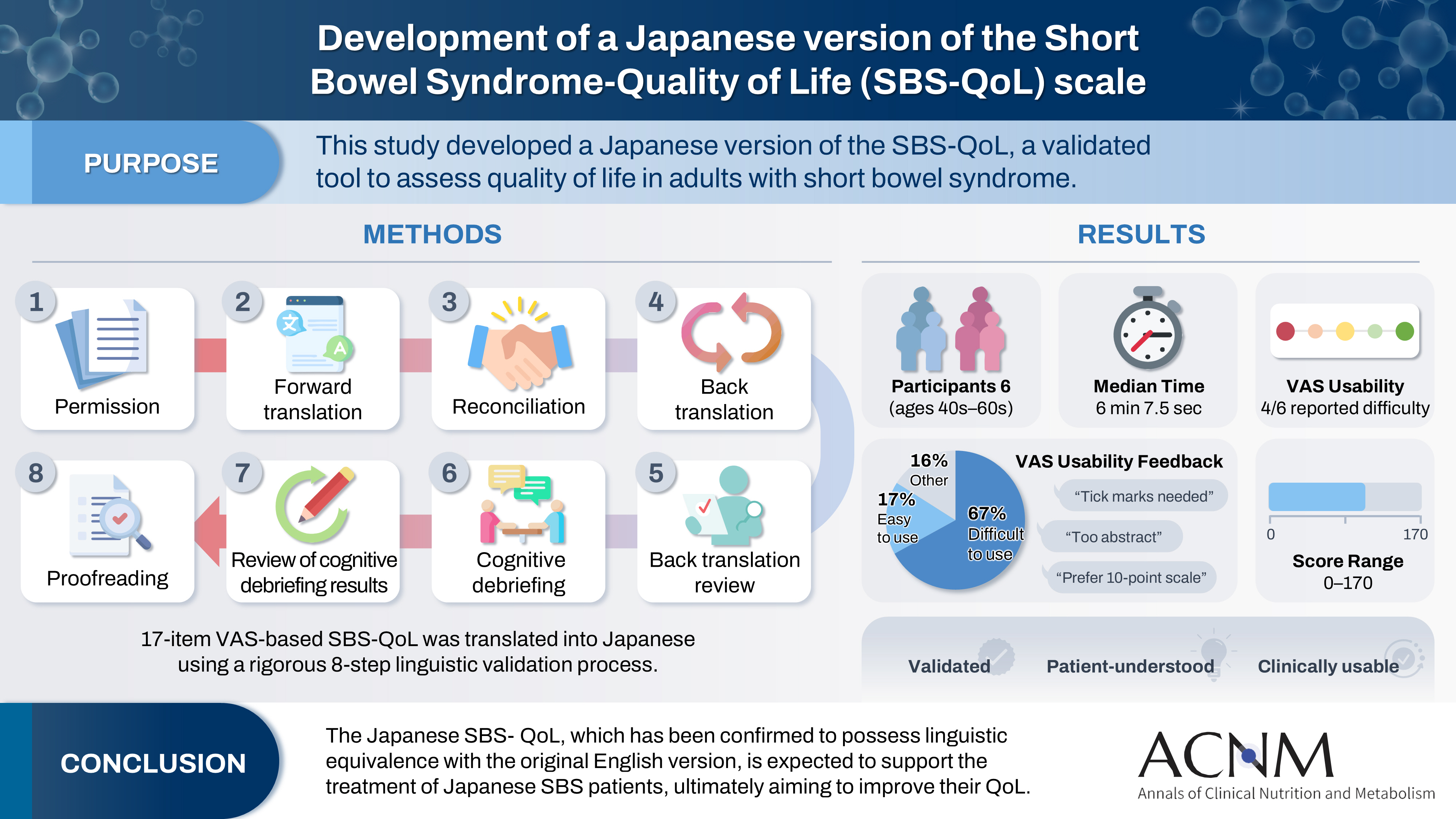
- Purpose
The Short Bowel Syndrome‐Quality of Life (SBS‐QoL) scale is a reliable and sensitive instrument developed to measure and evaluate the quality of life (QoL) in adult patients with short bowel syndrome (SBS). In Japan, increasing attention has been given to the assessment of QoL in patients with SBS; however, no Japanese‐language SBS‐specific scale is currently available. This study aimed to develop a Japanese version of the SBS‐QoL based on the original English version.
Methods
A provisional Japanese version was created in accordance with the guidelines of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force, utilizing a process of forward translation, adjustment, and back translation.
Results
Cognitive debriefing using the provisional Japanese version was conducted with six Japanese patients with SBS. Based on these results, the Japanese wording was evaluated and revised, leading to the creation of the final Japanese version.
Conclusion
The Japanese SBS‐QoL, which has been confirmed to possess linguistic equivalence with the original English version, is expected to support the treatment of Japanese SBS patients, ultimately aiming to improve their QoL.
- 1,781 View
- 19 Download

Review
- Dysphagia and quality of life: a narrative review
- Jung Mi Song
- Ann Clin Nutr Metab 2024;16(2):43-48. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.43
-
 Abstract
Abstract
 PDF
PDF - Purpose: Dysphagia is a chronic health condition that causes impairment of eating and drinking functions. It occurs in various diseases such as stroke, neurodegenerative disease, brain tumor, and head and neck cancer, and can also occur during the normal aging process.
Current concept: As patients experience symptoms of dysphagia, they no longer feel the pleasure of eating, depression and anxiety increase, and self-esteem decreases. Prolonged loss of appetite can lead to malnutrition, which can lead to death due to serious complications such as aspiration pneumonia and airway obstruction. Dysphagia reduces quality of life by affecting basic activities of daily living, limitations in social life, nutritional deficiencies, and mood disorders.
Conclusion: Accordingly, I plan to conduct a literature review on the quality of life of patients with dysphagia. First, to determine the relationship between quality of life and sociodemographic, physical health, and mental health characteristics of patients with dysphagia. I also aim to review quality of life measurement tools and intervention programs for patients with dysphagia. -
Citations
Citations to this article as recorded by- Incidence and Risk Factors of Dysphagia After Cardiac Surgery: A Scoping Review
Christos Kourek, Vania Labropoulou, Emilia Michou, Stavros Dimopoulos
Journal of Clinical Medicine.2025; 14(12): 4279. CrossRef - Psychometric Properties of the Spanish Version of the Swallowing Quality of Life Questionnaire in Fibromyalgia Patients
Irene Calles-Plata, Araceli Ortiz-Rubio, Laura Pérez-Gisbert, Irene Torres-Sánchez, Andrés Calvache Mateo, Marie Valenza, Alejandro Heredia-Ciuró
Healthcare.2025; 13(22): 2948. CrossRef - Association Between Swallowing Dysfunction and Multidimensional Quality of Life Among Community-Dwelling Healthy Korean Older Adults: A Pilot Cross-Sectional Study
Hyun-Ah Jang, Jun-Seon Choi
Healthcare.2025; 13(22): 2964. CrossRef
- Incidence and Risk Factors of Dysphagia After Cardiac Surgery: A Scoping Review
- 17,716 View
- 316 Download
- 3 Crossref

Original Articles
- Efficacy of high-protein diet protocol and education after distal gastrectomy for gastric cancer patients to prevent loss of lean body mass in Korea: a non-randomized controlled study
- Hee Kyung Yoon, Sun Ae Kim, Ji Yoon Han, Dong Jin Kim
- Ann Clin Nutr Metab 2024;16(1):10-19. Published online April 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.1.10
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: We studied whether active education of patients about the importance of a high-protein diet can prevent lean body mass loss after gastrectomy for gastric cancer.
Methods: In the study group, intensive high protein diet education and monitoring was performed immediate post operative, 1, 3, and 6 months after surgery. Study group patients were compared with data from the control group formed using propensity matching with the study group for age, sex, resection extent, and TNM stage. Clinicopathologic factors were compared between the groups, and changes in quality of life (QOL) and lean body mass between preoperative levels and 6 months after surgery were assessed.
Results: Among the 100 patients, 31 patients from each group were matched with propensity matching. The groups had no significant clinicopathologic differences. Although the changes in QOL scale and body composition did not differ statistically between the groups, a favorable trend was observed in the study group. Six months after surgery, the mean change in the QOL scale, which measured physical, role, emotional, cognitive, and social functioning, decreased less than the control group or even increased in the study group. In the body composition analysis, the study group showed greater reductions in weight, body mass index, fat mass, and body fat percentage than the control group, and their lean body mass and skeletal muscle mass decreased less.
Conclusion: A high-protein diet protocol and education might increase patient QOL and prevent a decrease in lean body weight 6 months after distal gastric resection.
- 4,813 View
- 42 Download

- Development of the Korean Version of the Gastrointestinal Quality of Life Index Questionnaire
- In Jun Yang, Heung-Kwon Oh, Jeehye Lee, Jung Wook Suh, Hong-min Ahn, Hyeonjeong Park, Hyun Hee Sim, Yong Beom Cho, In Kyu Lee, Seungbum Ryoo, Dong-Won Lee, Duck-Woo Kim, Sung-Bum Kang
- Ann Clin Nutr Metab 2022;14(1):32-37. Published online June 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.1.32
-
 Abstract
Abstract
 PDF
PDF - Purpose: To establish a standardized quality of life measurement that allows global cross-study comparisons, we translated the Gastrointestinal Quality of Life Index (GIQLI) into Korean and linguistically validated the Korean version of the GIQLI (K-GIQLI) in patients who underwent colorectal surgery.
Materials and Methods: A cross-cultural adaptation of the original GIQLI was created based on the established guidelines. Based on participation in a cognitive interview, 20 patients with colorectal cancer were enrolled in the study. To ensure that the Korean version of the questionnaire was understood as intended, the time needed to complete the questionnaire was measured, and three additional items related to comprehension were added.
Results: From May to July 2021, two translators, whose native language was Korean translated the GIQLI items into Korean, and a native English editor who had no knowledge of the original questionnaire translated the items back into English. In the cognitive interview, the median age of the patients was 61.8 (range: 44~82) years, and the median time required to complete the questionnaire was 6.5 (range: 5~10) min. For the language and cultural adaptation process, the participants’ comprehension of the questionnaire was measured on a scale of 1~5, with a mean score of 4 (range: 3~4).
Conclusion: The K-GIQLI was developed and did not exhibit a significant difference from the original English version in terms of social, linguistic, and cultural differences between the Western world and Republic of Korea. -
Citations
Citations to this article as recorded by- Comparison of laparoscopic and robotic surgery of choledochal cyst in pediatrics: single center experience
Jiyong Jang, Dayoung Ko, Joong Kee Youn, Hee-Beom Yang, Hyun-Young Kim
Surgical Endoscopy.2026; 40(1): 462. CrossRef - Longitudinal quality of life assessment after laparoscopic colorectal cancer surgery using the Gastrointestinal Quality of Life Index questionnaire: A multicentre prospective study
Tae‐Gyun Lee, Seung‐Bum Ryoo, Heung‐Kwon Oh, Yong Beom Cho, Chang Hyun Kim, Ju Hyun Lee, Hong‐Min Ahn, Hye‐Rim Shin, Mi Jeong Choi, Min Hyeong Jo, Duck‐Woo Kim, Sung‐Bum Kang
Colorectal Disease.2025;[Epub] CrossRef
- Comparison of laparoscopic and robotic surgery of choledochal cyst in pediatrics: single center experience
- 2,405 View
- 19 Download
- 2 Crossref

- Longitudinal Change in Health-Related Quality of Life after Total Gastrectomy: Approach Based on the Minimally Important Difference
- Sang Chun Park, Oh Jeong, Ji Hoon Kang, Mi Ran Jung
- Ann Clin Nutr Metab 2021;13(2):43-51. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.43
-
 Abstract
Abstract
 PDF
PDF - Purpose: The post-operative quality of life (QoL) is a significant concern for patients undergoing gastrectomy. Unlike subtotal gastrectomy, the detailed aspects of QoL involving the ability to perform everyday activities that reflect physical, psychological, and social well-being; and satisfaction with levels of functioning and control of the disease after total gastrectomy remain poorly investigated.
Materials and Methods: We enrolled 170 patients who underwent total gastrectomy for gastric carcinoma and completed the European Organisation for Research and Treatment of Cancer (EORTC) Quality-of-Life questionnaires (QLQ) C30 and STO22 preoperatively and post-operatively at 1, 6, and 12 months. We investigated the QoL change in terms of the minimally important difference (MID), which refers to a score change patients would perceive as clinically important (effect size >0.5).
Results: At 1-month post-surgery, MID in global health, physical, social, role, emotional, and cognitive functions was observed at 44.0%, 68.0%, 42.7%, 38.7%, 32.0%, and 16.0% respectively. Of QLQ-C30 symptoms, MID was frequently observed in appetite (52.9%). Of the QLQ-STO22 symptoms, MID was frequently observed in eating restrictions (74.1%), dysphagia (63.5%), pain (51.8%), and anxiety (50.6%). At 12 months post-surgery, MID in global health, physical, role, cognitive, social, and emotional functions was 32.9%, 58.8%, 42.4%, 40.0%, 36.5%, and 17.6%, respectively. Of QLQ-C30 symptoms, MID was frequently observed in diarrhea (52.9%). Of the QLQ-STO22 symptoms, MID was frequently observed in eating restrictions (63.5%), dysphagia (52.9%), body image (55.3%), pain (55.3%), and anxiety (51.8%). Male sex, comorbidity, D2 lymphadenectomy, and post-operative morbidity were associated with MID in global health at 12 months post-surgery.
Conclusion: This study provides information about the detailed aspects of impairment in various functions and symptoms of QoL after total gastrectomy. This information can be used to develop a tailor-made management plan for QoL. -
Citations
Citations to this article as recorded by- Experiences After Endoscopic Resection in Patients With Early Gastric Cancer in Korea: A Qualitative Study
Yoon Kyung Kim, Chun-Ja Kim, Eunyoung Park, Ji Yea Lee, Kee-Myung Lee, Elizabeth A. Schlenk
Journal of Transcultural Nursing.2025; 36(5): 593. CrossRef - Proximal gastrectomy with tubular stomach reconstruction vs total gastrectomy for proximal gastric cancer following neoadjuvant chemotherapy: A multicenter retrospective study
Yi-Ming Lu, Peng Jin, Hai-Kuo Wang, Xin-Xin Shao, Hai-Tao Hu, Yu-Juan Jiang, Wang-Yao Li, Yan-Tao Tian
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Experiences After Endoscopic Resection in Patients With Early Gastric Cancer in Korea: A Qualitative Study
- 3,327 View
- 9 Download
- 2 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


