Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
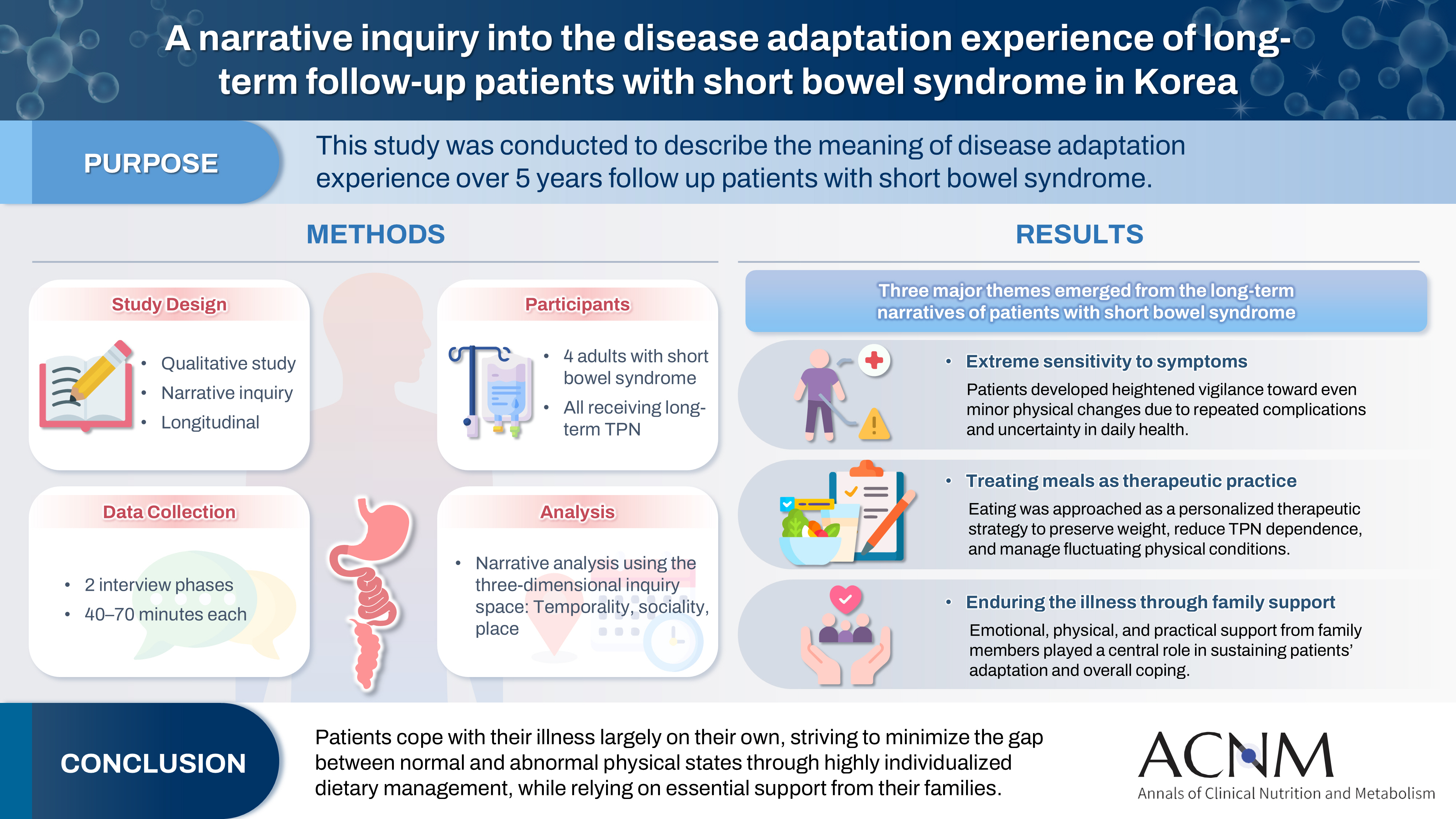
- A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
- Eun-Mi Seol, Eunjung Kim
- Ann Clin Nutr Metab 2025;17(3):188-195. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0028
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 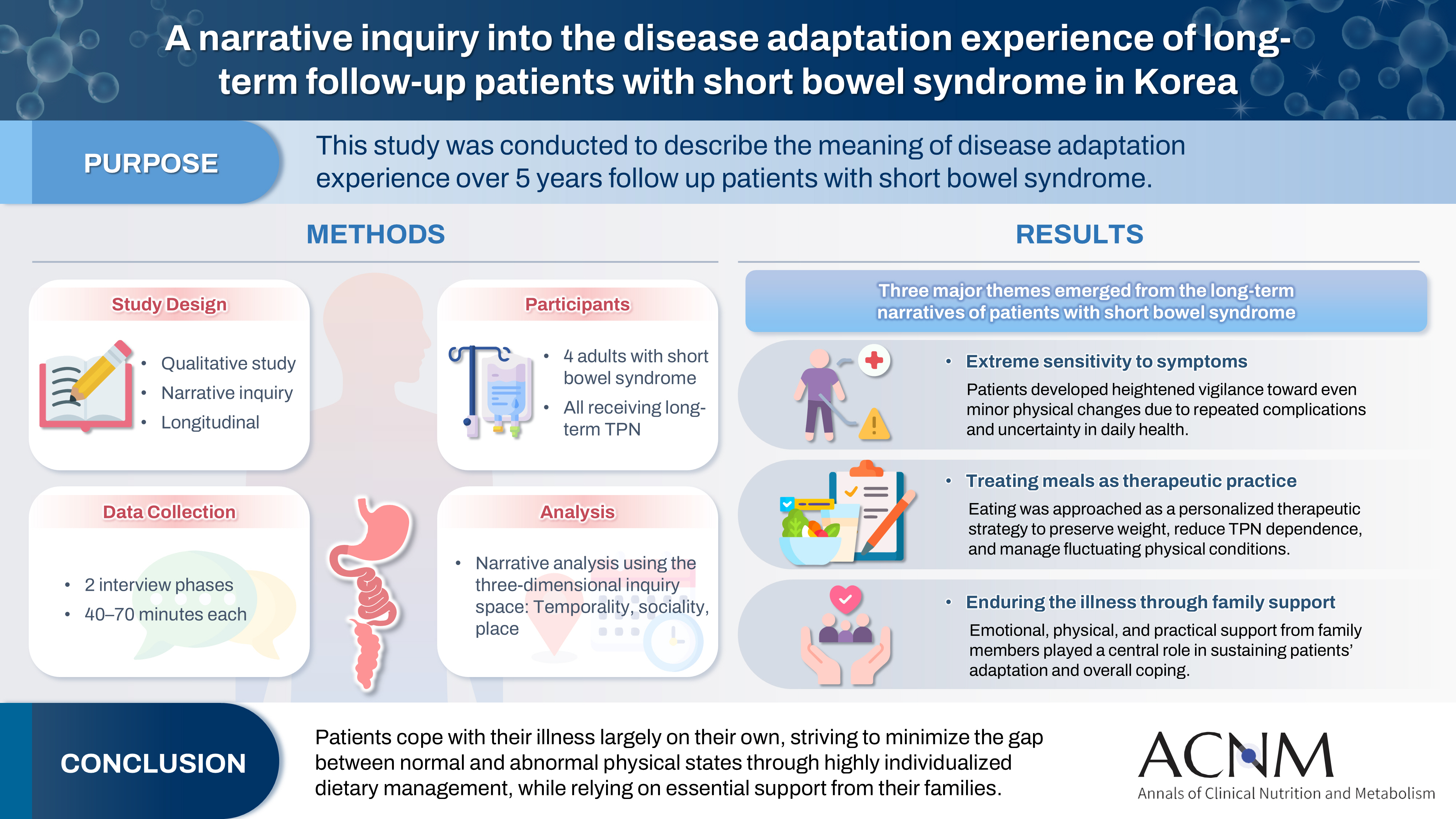
- Purpose
This study was conducted to describe the meaning of disease adaptation experience over a 5-year long-term follow-up of patients with short bowel syndrome.
Methods
Four patients were recruited from a tertiary hospital in Korea. This study was conducted through first and second interviews from January 2019 to July 2022. The transcribed data were analyzed using narrative methods.
Results
The mean age of the participants was 64 years, and the mean treatment period after small bowel resection was 100 months. The participants lost a mean of 19.3 kg body weight and all were receiving home total parenteral nutrition 2–7 days a week. The meaning of the experience of adapting to the disease for patients was found to be “extremely sensitive to the symptoms,” “considering eating food as another effective treatment method,” and “enduring the disease through family affection.”
Conclusion
Patients are struggling alone to cope with physical symptoms and adapt to their disease. For this, they are doing their best to narrow the gap between normal and abnormal physical conditions by thoroughly implementing diet therapy according to their physical characteristics. This entire process is supported by their families.
- 1,210 View
- 22 Download

- Vitamin D Deficiency is Prevalent in Short Bowel Syndrome Patients on Long-Term Parenteral Nutrition Support
- SungHyo An, Sanghoon Lee, Hyun-Jung Kim, Hyo Jung Park, Jeong-Meen Seo
- J Clin Nutr 2021;13(1):12-16. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.12
-
 Abstract
Abstract
 PDF
PDF - Purpose: Short bowel syndrome (SBS) is the most common etiology for intestinal failure (IF) and these patients are at high risk of developing micronutrient deficiencies. This study aimed at assessing the level of vitamins in adult SBS patients at different stages of their disease before the initiation of multidisciplinary intestinal rehabilitation.
Methods: Patient data from November 2015 to March 2017 were retrospectively reviewed. Adult patients who underwent extensive bowel resection and were classified as SBS-IF were selected. Clinical data including age, sex, etiology of IF, biochemical data, nutritional status, nutrition support, and outcome of intestinal rehabilitation were analyzed.
Results: Nine patients with SBS-IF were included in the analysis. There were 6 male patients and 3 female patients, with a median age of 55.0 years. Vitamin levels were analyzed at 306 days (median) after the development of SBS. At the time of vitamin levels screening, 4 patients were receiving daily intravenous vitamin supplementation. Five patients were not receiving vitamin supplementations, either intravenously or orally. Vitamin B12 was within the normal range in 6 patients and higher than normal in 3 patients. Vitamin D was within the normal range in 3 patients and lower than normal in 6 patients. Vitamin E was within the normal range in 7 patients and higher than normal in 2 patients. Folate was within the normal range in 8 patients (not checked in 1 patient). Ambulatory patients had significantly higher vitamin D levels compared to hospitalized patients (P=0.015).
Conclusion: Vitamin D levels had decreased in 67% of patients with SBS in Korea, while vitamin B12, folate, and vitamin E deficiencies were rarely seen. -
Citations
Citations to this article as recorded by- A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
Eun-Mi Seol, Eunjung Kim
Ann Clin Nutr Metab.2025; 17(3): 188. CrossRef
- A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
- 1,893 View
- 6 Download
- 1 Crossref

- Muscle Protein Metabolism in Critically Illness
- Min Chang Kang
- Surg Metab Nutr 2020;11(2):35-39. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.35
-
 Abstract
Abstract
 PDF
PDF - Most patients experience a considerable amount of muscle wasting during critical care. A decrease in muscle mass causes weakness which inevitably leads to delayed recovery. Since muscle also plays an important role in protein metabolism, metabolic instability increases as muscle mass decreases. Accordingly, various treatments have been attempted to maintain muscle mass and function in critically ill patients; however, it is still difficult to prevent muscle loss. It is known that muscle wasting in critical illness is primarily due to increased muscle protein breakdown rather than a decrease in muscle protein synthesis. Nutritional therapy and rehabilitation are fundamentally important, but additional anabolic agents may be needed to overcome anabolic resistance. In this review, we will learn about muscle protein metabolism in critically ill patients and how various treatments affect muscle protein metabolism.
-
Citations
Citations to this article as recorded by- Combined intravenous bolus amino acid supplementation and mobilization on early muscle loss in critically ill adults: A randomized controlled trial
Lizl Veldsman, Guy A. Richards, Daniel Nel, Tertius A. Kohn, Renée Blaauw
Journal of Parenteral and Enteral Nutrition.2026; 50(2): 170. CrossRef - Low protein content of plant-derived nutrition limits the protein transition in hospitalized patients: Results from an observational study
M.A. van Bree, B.C. Schouten, E.S. Wolters, M.R. Soeters, H.M. Kruizenga
Clinical Nutrition ESPEN.2025; 69: 311. CrossRef - Combined Protein, Probiotics, and Exercise Therapy for Sarcopenia: A Comprehensive Review
Ryuk Jun Kwon, Mohammad Al Mijan, Soo Min Son, Wanho Yoo, Taehwa Kim
Cells.2025; 14(17): 1375. CrossRef - Double-Edge Effects of Leucine on Cancer Cells
Burkitkan Akbay, Zhannur Omarova, Alexander Trofimov, Bayan Sailike, Orynbassar Karapina, Ferdinand Molnár, Tursonjan Tokay
Biomolecules.2024; 14(11): 1401. CrossRef - Compartmental analysis: a new approach to estimate protein breakdown and meal response in health and critical illness
Nicolaas E. P. Deutz, Mariëlle P. K. J. Engelen
Frontiers in Nutrition.2024;[Epub] CrossRef - Amino acid kinetics in the critically ill
Nicolaas E.P. Deutz, Krista L. Haines, Paul E. Wischmeier, Mariëlle P.K.J. Engelen
Current Opinion in Clinical Nutrition & Metabolic Care.2024; 27(1): 61. CrossRef
- Combined intravenous bolus amino acid supplementation and mobilization on early muscle loss in critically ill adults: A randomized controlled trial
- 4,774 View
- 34 Download
- 6 Crossref

- Multidisciplinary Intestinal Rehabilitation for Short Bowel Syndrome in Adults: Results in a Korean Intestinal Rehabilitation Team
- Sojeong Yoon, Sanghoon Lee, Hyo Jung Park, Hyun-Jung Kim, Jihye Yoon, Ja-Kyung Min, Jeong-Meen Seo
- J Clin Nutr 2018;10(2):45-50. Published online December 31, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.2.45
-
 Abstract
Abstract
 PDF
PDF Purpose:
Intense multidisciplinary team effort is required for the intestinal rehabilitation of patients afflicted with the short bowel syndrome (SBS). These include enteral and parenteral nutrition (PN) support, monitoring of complications related to treatment, and considering further medical or surgical options for intestinal adaptation.
Methods:
In the Intestinal Rehabilitation Team (IRT) at the Samsung Medical Center, we have experienced 20 cases of adult SBS requiring multidisciplinary intestinal rehabilitation. This study is a retrospective review of the collected medical records.
Results:
Of the 20 subjects treated, 12 patients were male and 8 patients were female. At the time of referral to the IRT, the mean age was 51.5 years, and the mean body weight was 50.1 kg, which was 90% of the usual body weight. The diseases or operative managements preceding massive bowel resection were malignancy in 11 cases, cardiac surgery in 2 cases, trauma in 2 cases and one case, each of tuberculosis, corrosive esophagitis, atrial fibrillation, simultaneous pancreas and kidney transplantation, and perforated appendicitis. Of these, there were 14 survivals and 6 mortalities. The fatalities were attributed to progression of disease, intestinal failure-associated liver disease, and sepsis (unrelated to intestinal failure) (2 cases each). Among the 14 surviving patients, 8 patients have been weaned off PN, whereas 6 are still dependent on PN (mean PN dependence 36%).
Conclusion:
This paper reports the results of multidisciplinary intestinal rehabilitation of adult short bowel patients treated at the Samsung Medical Center. Further studies are required to improve survival and enteral tolerance of these patients.
-
Citations
Citations to this article as recorded by- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
Yunhyung Kim, Yeon Hee Kim, Jae Sim Jeong
Journal of Korean Association for Qualitative Research.2024; 9(1): 1. CrossRef - Intestinal Rehabilitation Program for Adult Patients with Intestinal Failure: A 20-Year Analysis of Outcomes in the Single-Center Experience at a Tertiary Hospital
Kyoung Moo Im, Jae Hee Chung
Digestive Diseases and Sciences.2024; 69(5): 1770. CrossRef - Vitamin D Deficiency is Prevalent in Short Bowel Syndrome Patients on Long-Term Parenteral Nutrition Support
SungHyo An, Sanghoon Lee, Hyun-Jung Kim, Hyo Jung Park, Jeong-Meen Seo
Journal of Clinical Nutrition.2021; 13(1): 12. CrossRef - Multidisciplinary Intestinal Rehabilitation in Children: Results from a Korean Intestinal Rehabilitation Team
Cheolgu Lee, Sanghoon Lee, Hyo Jung Park, Hyun-Jung Kim, Ja-Kyung Min, Jeong-Meen Seo
Advances in Pediatric Surgery.2020; 26(2): 61. CrossRef
- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
- 1,223 View
- 1 Download
- 4 Crossref

- Early Experience with Serial Transverse Enteroplasty in a Korean Intestinal Rehabilitation Team
- Jiyoon Hong, Sang Oh Yun, Sanghoon Lee, Hyun-Jung Kim, Hyo Jung Park, Jeong-Meen Seo
- Surg Metab Nutr 2018;9(1):11-15. Published online June 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.1.11
-
 Abstract
Abstract
 PDF
PDF Purpose:
For patients with short bowel syndrome, surgery can play an important role in the management of intestinal failure (IF). Serial transverse enteroplasty (STEP) has become a popular choice of bowel lengthening among surgeons for its safety and effectiveness in improving enteral autonomy. In this study, we report 5 cases of STEP procedure on 4 patients.
Materials and Methods:
In the Intestinal Rehabilitation Team at Samsung Medical Center, all patients were managed by a multidisciplinary team specialized in the care of intestinal failure patients. Retrospective review of medical records was performed.
Results:
3 patients were children and 1 patient was an adult. Improvement in enteral autonomy was achieved in all patients following each STEP procedure. Suspected suture line leakage was seen in one patient, which was successfully managed by conservative treatment There were no other serious complications related to the procedures.
Conclusion:
STEP procedure continues to be an important management option in intestinal rehabilitation of patients with extreme short bowel. We report a small series of STEP performed safely and effectively in Korea.
-
Citations
Citations to this article as recorded by- Early Bowel Lengthening Procedures: Bi-Institutional Experience and Review of the Literature
Elisa Negri, Riccardo Coletta, Lynette Forsythe, Francesca Gigola, Maria Chiara Cianci, Antonino Morabito
Children.2022; 9(2): 221. CrossRef
- Early Bowel Lengthening Procedures: Bi-Institutional Experience and Review of the Literature
- 1,105 View
- 1 Download
- 1 Crossref

- Nutrition Therapy for Adult Intestinal Failure Patients
- Hyo Jung Park
- J Clin Nutr 2016;8(3):72-76. Published online December 31, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.3.72
-
 Abstract
Abstract
 PDF
PDF Intestinal failure (IF) is a condition, in which the intestinal function or length remaining is below the minimum amount required for the absorption of sufficient nutrients and fluid to maintain normal life. The nutritional supply of IF depends on the anatomical site, length, and function of the remaining bowel. The goals of nutritional therapy for patients with IF are to achieve bowel adaptation to absorb nutrients sufficiently to live a healthy life with the current intestinal condition, and to promote the enteral autonomy to control nutrient digestion, absorption, excretion, and bowel movement. To stabilize and recover the patient’s nutrition condition after a huge bowel resection, the intestinal rehabilitation team (IRT) for individual nutritional therapy should be established. IRT carefully monitors the changes in body weight, medication use, patient’s symptoms, nutrient deficiency, hydration status, function of the remaining bowel, degree of bowel adaptation, adverse effects due to nutritional therapy, and enteral balance. To achieve intestinal adaptation and enteral autonomy through complicated and difficult nutritional intensive therapy in IF patients, it is essential to manage the patients through multidisciplinary collaboration involving physicians, pharmacists, dietitians, and nurses.
- 800 View
- 2 Download

- Intestinal Rehabilitation after Extensive Bowel Resection in Post-Gastrectomy Patients
- Seung Rim Han, Sanghoon Lee, Chae-Youn Oh, Hyun-Jung Kim, Hyo Jung Park, Jun Ho Lee, Tae Sung Sohn, Jae Moon Bae, Jeong-Meen Seo
- Surg Metab Nutr 2015;6(2):33-37. Published online December 30, 2015
- DOI: https://doi.org/10.18858/smn.2015.6.2.33
-
 Abstract
Abstract
 PDF
PDF Purpose:
Surgical complications requiring massive bowel resection after gastrectomy are rare. However, when such an event occurs the patient may develop short bowel syndrome and intestinal failure. We report our experience of intestinal rehabilitation in four post-gastrectomy patients.
Materials and Methods:
From January 2011 to June 2014, four cases of short bowel syndrome were identified in post-gastrectomy patients. All patients were managed by a multidisciplinary team specialized in the care of intestinal failure patients. Patients’ medical records were reviewed retrospectively.
Results:
The original diagnosis was early gastric cancer in all patients. One patient had synchronous esophageal cancer. Patients required extensive bowel resection due to bowel strangulation from internal herniation (3 cases), superior mesenteric artery torsion (1 case). Remnant small bowel length ranged from 10 cm to 80 cm and partial resection of the colon was performed in three cases. One patient received serial transverse enteroplasty (STEP) and one patient is receiving continuous enteral feeding via surgical gastrostomy. There were no cases of intestinal failure-associated liver disease. Two patients are receiving home parenteral nutrition in varying degrees. Two patients have been weaned off parenteral nutrition.
Conclusion:
Four post-gastrectomy patients with short bowel syndrome were managed. Despite application of various medical and surgical measures, weaning off parenteral nutrition was difficult in these patients.
- 872 View
- 0 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


