Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
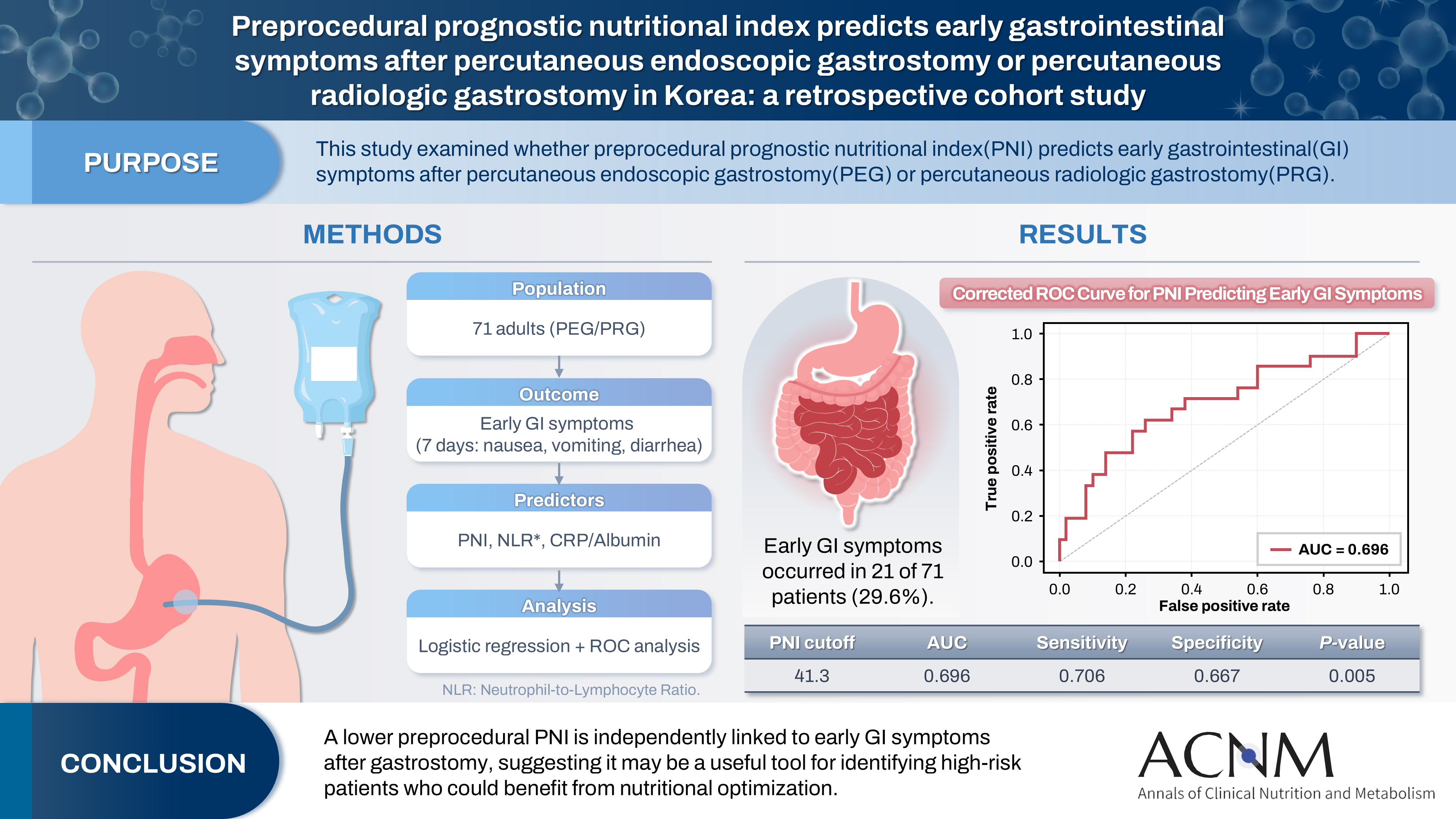
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
- Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0032
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 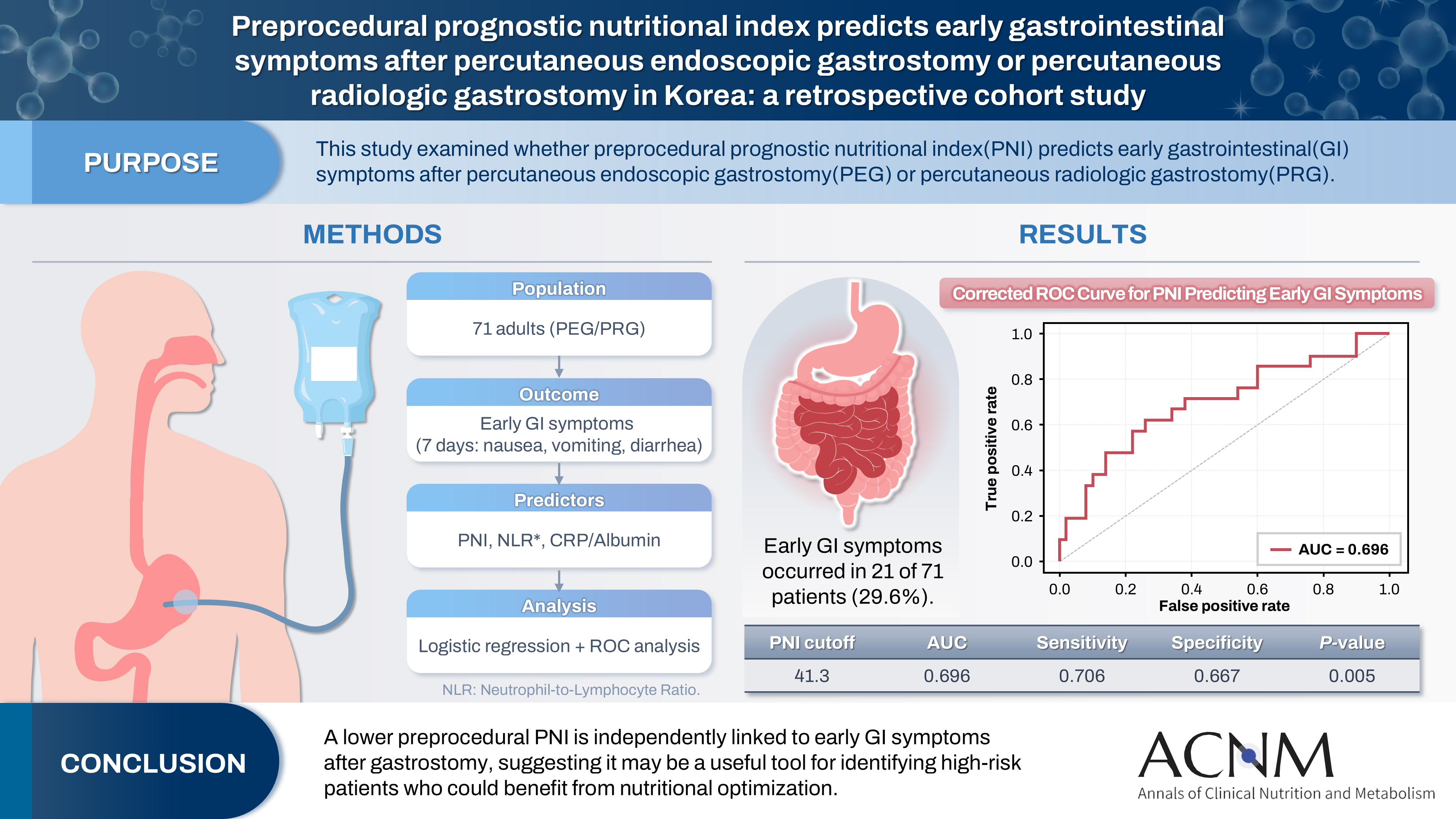
- Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
- 869 View
- 19 Download

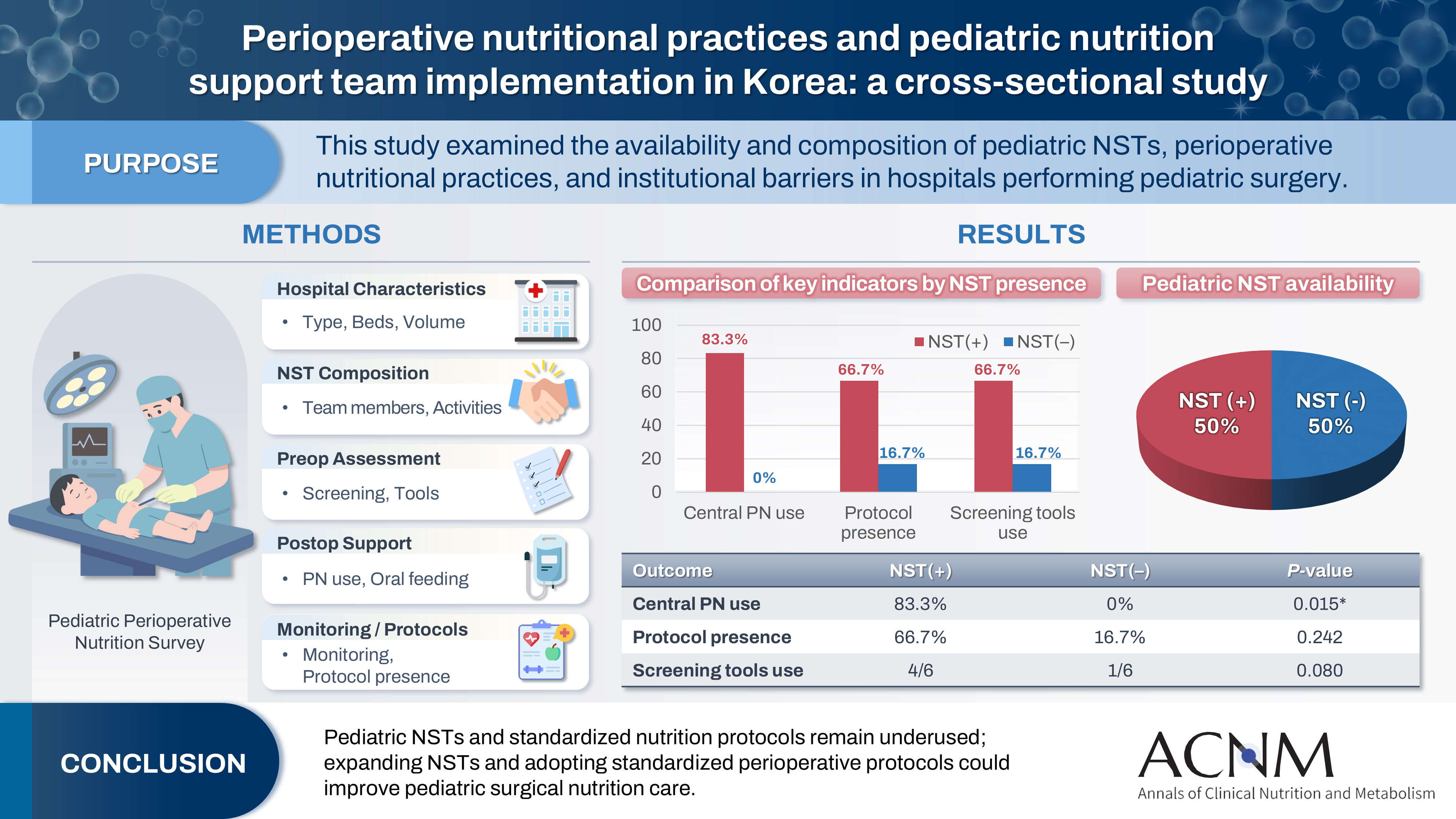
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 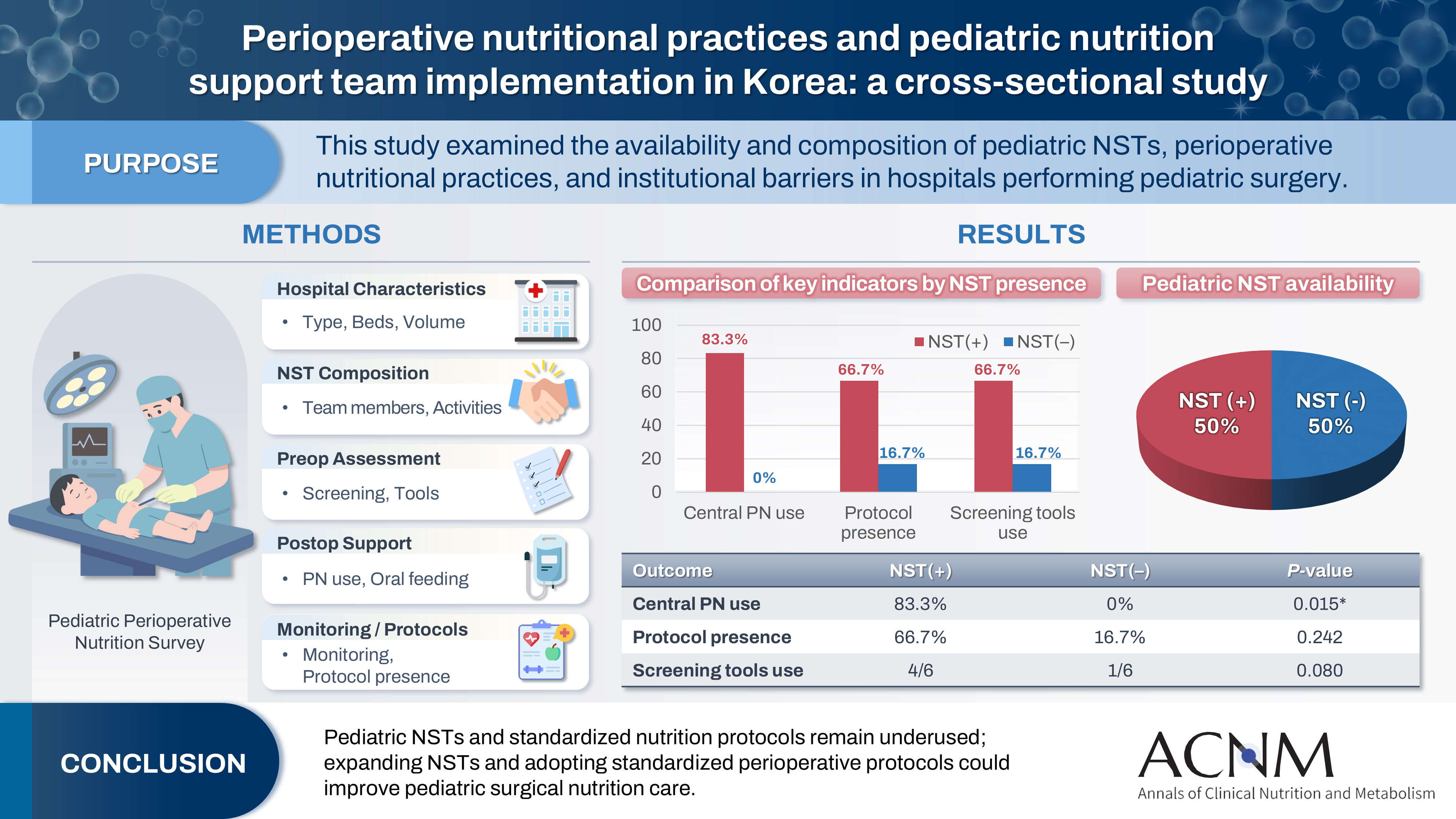
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 1,448 View
- 23 Download

- Perioperative nutritional management to improve long-term outcomes in critically ill perioperative organ transplant patients: a narrative review
- Toshimi Kaido
- Ann Clin Nutr Metab 2025;17(1):18-24. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0005
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review examines the significance of perioperative nutritional management in organ transplantation, with a particular focus on liver transplantation. Organ transplant recipients often experience malnutrition and sarcopenia due to nutritional and metabolic abnormalities associated with organ dysfunction. Because transplantation is a highly invasive procedure, optimizing perioperative nutritional care is critical for improving short-term outcomes and reducing postoperative infection-related mortality.
Current concept
Recent clinical investigations have shown that liver transplant recipients, who are frequently afflicted with end-stage liver disease and uncompensated cirrhosis, are particularly vulnerable to protein-energy malnutrition and secondary sarcopenia. Our analysis identified low pre-transplant nutritional status and the absence of preoperative branched-chain amino acid supplementation as independent risk factors for post-transplant sepsis. In response, we developed a customized nutritional therapy protocol that incorporates precise body composition analysis, serial measurements of biochemical markers (including prealbumin, zinc, and the branched-chain amino acid/tyrosine ratio), and targeted supplementation with branched-chain amino acids, zinc acetate, and synbiotics. Early initiation of enteral nutrition coupled with postoperative rehabilitative interventions resulted in improved outcomes. In addition, stratified body composition parameters correlated with survival differences and informed revised transplantation criteria.
Conclusion
Tailored perioperative nutritional management and rehabilitative strategies are essential for improving early postoperative outcomes in liver transplantation. These findings underscore the need for proactive nutritional assessment and intervention, which may represent a breakthrough in transplant prognosis. Future research should refine nutritional protocols and integrate novel biomarkers, while education and interdisciplinary collaboration remain crucial for enhancing transplant outcomes and reducing complications. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 4,356 View
- 108 Download
- 1 Crossref

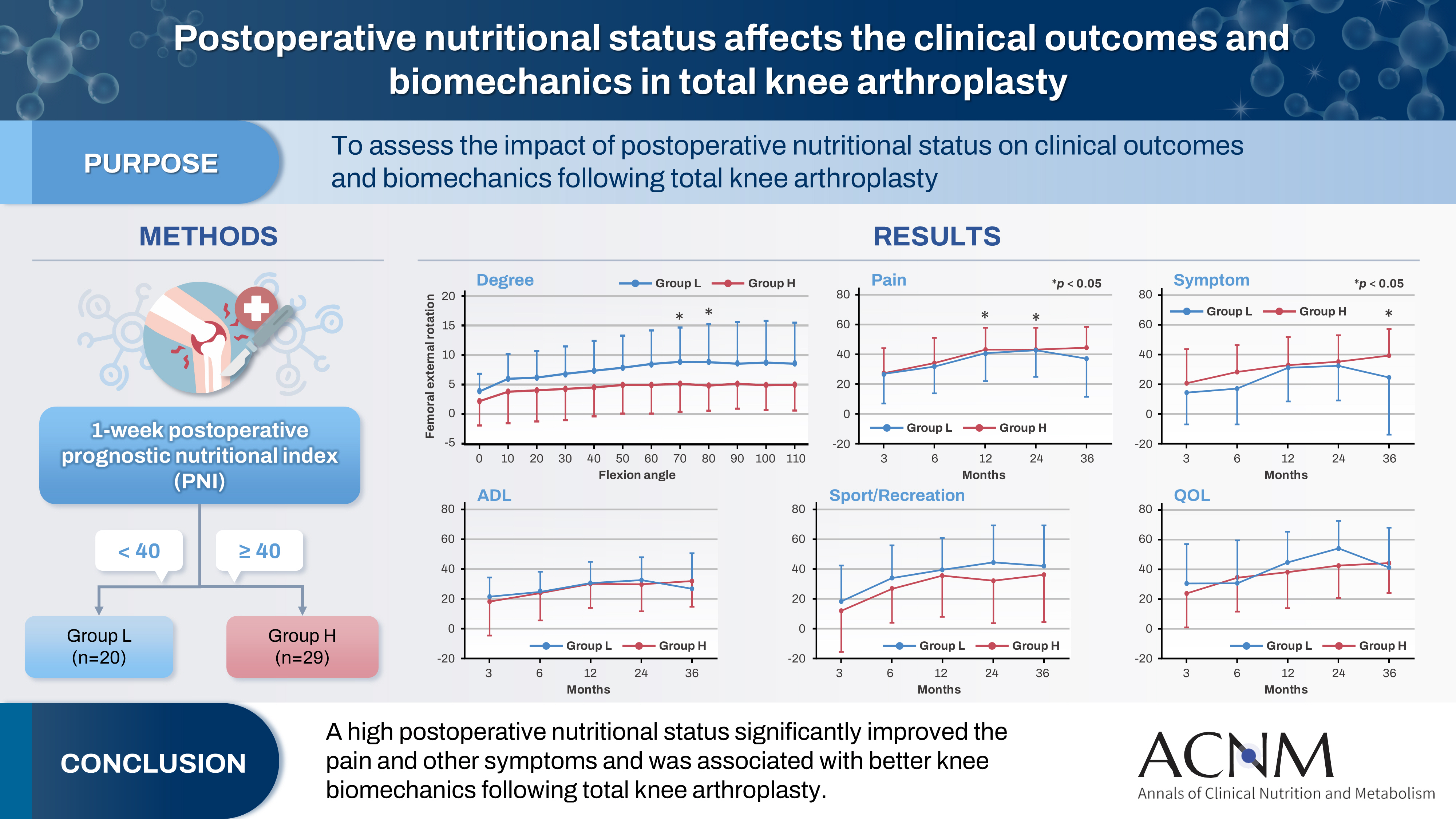
- Impact of postoperative nutritional status on the patients’ clinical outcomes and knee biomechanics following total knee arthroplasty in Japan: a prospective cohort study
- Kenichi Kono, Tetsuya Tomita, Takaharu Yamazaki, Masashi Tamaki, Shuji Taketomi, Ryota Yamagami, Reo Inoue, Yuki Taniguchi, Sakae Tanaka, Kazuhiko Fukatsu
- Ann Clin Nutr Metab 2025;17(1):50-57. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.019
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 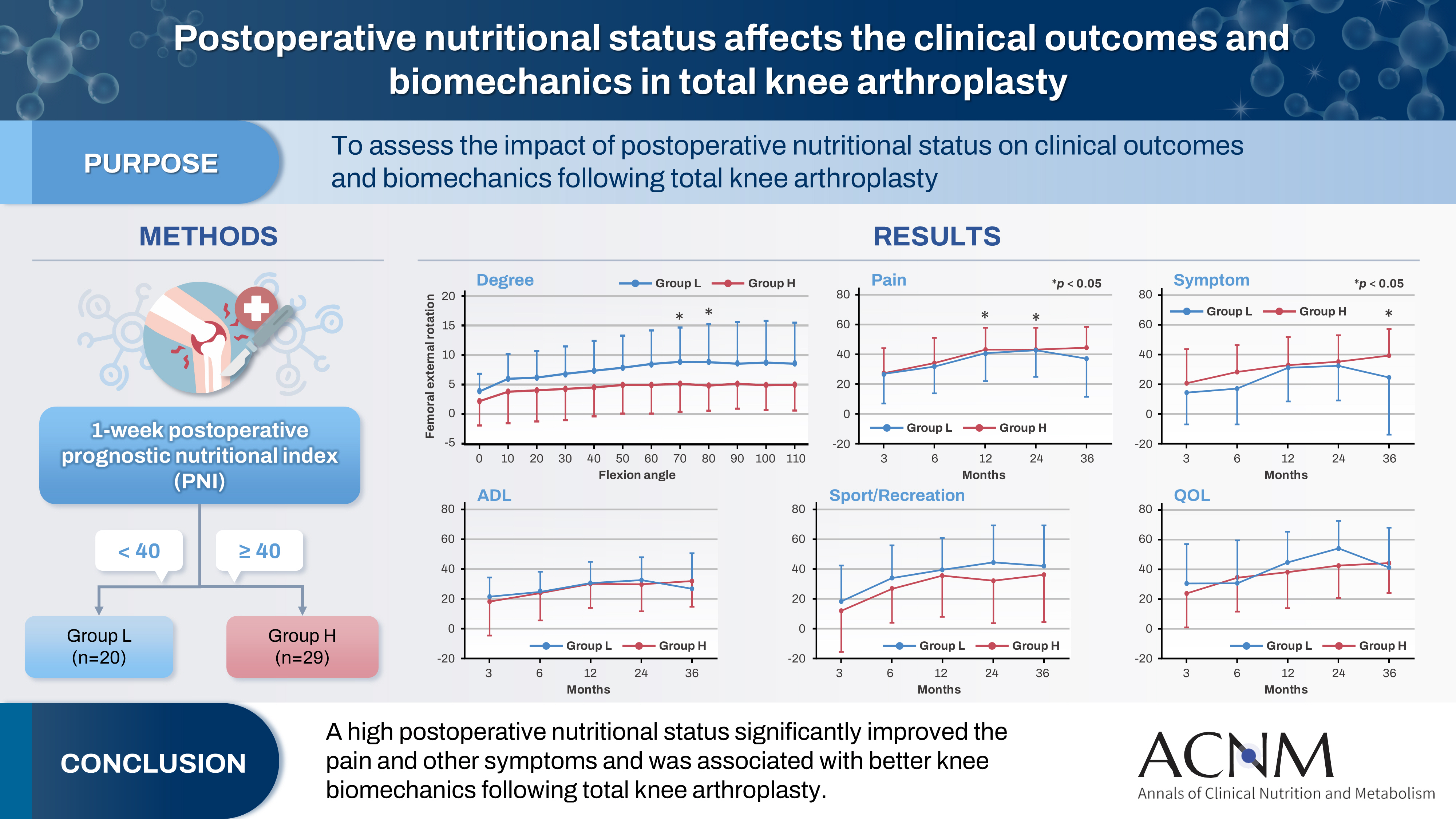
- Purpose
The impact of postoperative nutritional status on clinical outcomes and biomechanics following total knee arthroplasty remains largely unknown. This study aimed to assess this question using the prognostic nutritional index to evaluate the nutritional status of orthopedic participants.
Methods
Patients with knee osteoarthritis who underwent total knee arthroplasty (n=49) in Japan were divided into two groups based on their 1-week postoperative prognostic nutritional index. Group L patients had a prognostic nutritional index <40, whereas Group H comprised patients with a prognostic nutritional index ≥40. Postoperative improvements in Knee Injury and Osteoarthritis Outcome Score were evaluated. The patients performed squats under single-fluoroscopic surveillance in the sagittal plane for biomechanical evaluation. A two-dimensional/three-dimensional registration technique was employed to measure the tibiofemoral kinematics. The axial rotation of the femoral component relative to the tibial component and the anteroposterior translation of the medial and lateral femorotibial contact points were measured.
Results
Group H showed significantly higher pain scores than Group L at 12 and 36 months postoperatively and a significantly higher symptom score at 36 months postoperatively. The kinematic comparison revealed that the axial external rotation in Group L was larger than that in Group H from 70° to 80° with flexion. Moreover, in the medial anteroposterior translation, Group L was more anteriorly located than Group H, with flexion beyond 30°.
Conclusion
The results suggest that a high postoperative nutritional status significantly improved pain and other symptoms and was associated with better knee biomechanics following total knee arthroplasty.
- 2,769 View
- 37 Download

- Perioperative nutritional practices and attitudes among gastrointestinal oncologic surgeons in Korea: a nation-wide survey study
- Dae Hoon Kim, Jeong-Meen Seo, Min-Gew Choi
- Ann Clin Nutr Metab 2023;15(3):81-87. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.81
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: This study aimed to investigate the current perioperative nutritional practices and attitudes among gastrointestinal (GI) oncologic surgeons in Korea. Evidence-based perioperative nutritional practices are not well-established in this field.
Methods: A nationwide survey was conducted with 24 items, targeting GI oncologic surgical faculty members from March 2022 to April 2022 through social networking service messaging and email. Whole target number was 3,421.
Results: Out of responding 161 GI surgeons, 83.9% were male and 16.1% were female, and about 49.7% were in their 40s. When asked about their hospital policies, 67.1% reported the existence of formal nutritional screening programs. However, the execution and analysis of these programs varied considerably. Most surgeons conducted preoperative nutritional screening, with albumin testing the most frequently performed. In addition, nutritional supplementation—primarily protein drinks—was given before surgery. The duration for which these supplements were used varied from ≤3 days to 4–7 days. Most respondents recognized the importance of addressing nutritional deficiencies in patients with GI tumors; however, when asked about immunonutrition, 89.4% of surgeons admitted having limited knowledge.
Conclusion: Although there is recognition of the importance of evidence-based nutrition practices in GI and oncologic surgery programs, this study reveals limited implementation of such practices. This study highlights a considerable opportunity to leverage existing positive surgeon beliefs and published data on the benefits of perioperative nutrition to enhance surgical nutrition practices and to improve patient outcomes in Korea.
- 1,592 View
- 10 Download

- Perioperative nutrition support: a narrative review
- Rajeev Joshi, Asma Khalife
- Ann Clin Nutr Metab 2023;15(2):40-45. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.40
-
 Abstract
Abstract
 PDF
PDF - Purpose: Proper nutrition and supplementation are paramount in surgical patients. Suboptimal nutrition status is increasingly recognized as an independent predictor of poor surgical outcomes. The purpose of this review is to highlight the need for nutritional protocols, with an emphasis on perioperative nutrition.
Current concept: Perioperative nutrition support is considered an adjunctive strategy in most centers, although it is proven to be the key in improving surgical outcomes. There is a need to increase the standards and formulate policies and protocols to optimize perioperative nutrition support. Components of perioperative nutrition include nutritional screening and assessment, prehabilitation, preoperative metabolic optimization and carbohydrate loading, postoperative early enteral feeding and perioperative parenteral nutrition, immunonutrition and micronutrients, and oral nutritional supplementation vs. hospital-based kitchen feeds. Supplemental parenteral nutrition becomes valuable when enteral nutrition alone cannot fulfil energy needs. In patients in the surgical intensive care unit who are dealing with hemodynamic instability, high levels of serum lactate unrelated to thiamine deficiency, acidosis, significant liver dysfunction, high blood sugar, and high blood lipid levels, parenteral nutrition must be started with caution. In the post-surgery care ward, it is advisable to administer up to 30 kcal/kg/day and 1.2–2 g/kg/day of protein.
Conclusion: The positive impact of comprehensive nutritional support and the importance of setting and executing standards must be highlighted. Emphasis should be placed on overcoming existing challenges in implementing nutrition therapy in current surgical practice, as better perioperative nutrition supports better surgical outcomes. -
Citations
Citations to this article as recorded by- Nutritional intervention for weight loss in presurgical phase – case study
Ana-Maria Damian
The Romanian Journal of Nutrition.2024; 4(4): 4. CrossRef
- Nutritional intervention for weight loss in presurgical phase – case study
- 26,297 View
- 235 Download
- 1 Crossref

- Impact of Visceral Fat Area Measured by Bioelectrical Impedance Analysis on Clinico-Pathologic Outcomes of Colorectal Surgery
- Kyeong Eui Kim, Woo Jin Song, Minji Seok, Sung Uk Bae, Woon Kyung Jeong, Seong Kyu Baek
- J Clin Nutr 2021;13(1):17-23. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.17
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study investigated the relationship between the visceral fat area (VFA) and clinico-pathological outcomes in patients with colorectal cancer (CRC).
Methods: This retrospective study included 204 patients who underwent anthropometric measurement by bioelectrical impedance analysis (BIA) before surgical treatment for CRC between January 2016 and June 2020.
Results: According to the average value of the visceral fat area, 119 (58.3%) patients had a low visceral fat area, and 85 (59.1%) patients had a high visceral fat area. Patients with visceral obesity showed a higher BMI compared to patients without visceral obesity, (21.8±1.9 vs. 25.7±2.5, P<0.001). There was no significant difference in the overall perioperative outcomes including total operation time, time to gas out, sips of water, soft diet, hospital stay, and morbidity between patients in the low and high VFA groups. We divided patients into two subgroups according to the degree of cancer progression and more advanced cases with low VFA showed significantly more total and positive retrieved lymph nodes (LNs) (20.9±10.3 vs. 16.1±7.1, P=0.021 and 3.3±2.9 vs. 2.2±2.3, P=0.019, respectively) and a higher proportion of more than 12 retrieved LNs compared to patients with a high VFA (95.1% vs. 90.0%, P=0.047). Body composition analysis showed that phase angle, muscle composition, and body fluid composition were not statistically different between the two groups. However, body fat mass was statistically higher in the high VFA group (22.0±4.6 vs. 12.8±3.1, P<0.001).
Conclusion: Visceral obesity measured by BIA showed lower total and positive retrieved LNs and was not associated with adverse peri-operative outcomes, inflammatory and nutritional, and pathologic outcomes for CRC.
- 1,451 View
- 3 Download

- Analysis of Muscle Using CT Anthropometry in Major Trauma Patients
- Hang Joo Cho, Yunsup Hwang, Yoon Hyun Lee, Dae Hyun Cho, Dae-Sang Lee, Maru Kim
- Surg Metab Nutr 2020;11(1):12-15. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.12
-
 Abstract
Abstract
 PDF
PDF - Purpose: The feasibility of nutritional assessment using computed tomography anthropometry has been previously proven. The abdominal muscle at the L3 vertebra is a well-known nutritional biomarker for predicting the prognosis of various diseases, and especially sarcopenia. However, any studies on nutritional assessment of the brain, face, or neck via computed tomography are still scarce. We retrospectively investigated the applicability of the masseter muscle as a nutritional biomarker.
Materials and Methods: Patients who underwent simultaneous brain and abdominopelvic computed tomography at a regional trauma center were retrospectively analyzed. Their masseter muscles at 2 cm below the zygomatic arch and abdominal muscle at L3 were assessed via computed tomography anthropometry. Basic clinical data including trauma information was also reviewed. The data was analyzed in conjunction with the patients’ mortality.
Results: A total of 411 patients were analyzed in the study (316 men and 95 women, mean age: 50.41 years, mean areas of the masseter and abdominal muscles: 10.6 and 137.3 cm2, respectively) and there 146 major trauma patients with an injury severity score higher than 15. The masseter muscle area was decreased in the mortality group of major trauma patients (10.4 vs 7.9 cm2, P=0.001). However, abdominal muscles did not show statistical significance (137.9 vs. 117.7 cm2, P=0.054).
Conclusion: The masseter muscle, when analyzed via computed tomography anthropometry, showed a statistical association with patients’ mortality and it could prove its feasibility as a nutritional biomarker.
- 683 View
- 1 Download

- Clinical Application of Bioelectrical Impedance Analysis and its Phase Angle for Nutritional Assessment of Critically III Patients
- Hyung-Sook Kim, Eun Sook Lee, Yeon Joo Lee, Jae Ho Lee, Choon-Taek Lee, Young-Jae Cho
- J Clin Nutr 2015;7(2):54-61. Published online August 31, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.2.54
-
 Abstract
Abstract
 PDF
PDF Purpose:
Phase angle (PA) is objectively determined from resistance and reactance measured by bioelectrical impedance analysis (BIA)−a quick, noninvasive method. The aim of this study was to evaluate the clinical application of PA by BIA for nutritional assessment of critically ill patients.
Methods:
Eighty nine adult patients admitted to a medical intensive care unit (ICU) of a tertiary academic hospital from August 2012 to September 2013 were analyzed. PA values were measured by direct segmental multi-frequency BIA. As traditional nutrition assessment tools, body mass index (BMI), serum albumin levels, total lymphocyte counts, and our hospital’s nutrition screening index (NSI) were also recorded. Correlations between the results of BIA and other traditional parameters were analyzed.
Results:
PA showed correlation with traditional nutritional parameters, including BMI (r=0.479), serum albumin (r=0.347), and NSI score (r=0.483). Patients with PA lower than the median value (3.5°) had significantly lower nutritional status, increased duration of mechanical ventilation (P=0.039), and increased length of ICU stay (P=0.041).
Conclusion:
PA, as a reflection of body cell mass, measured by BIA could be a potentially useful parameter for nutritional assessment in critically ill patients.
-
Citations
Citations to this article as recorded by- Optimal Enteral Nutrition Support Preserved Muscle Mass in Critically Ill Children
Kantisa Sirianansopa, Chavisa Rassameehirun, Sirinuch Chomtho, Orapa Suteerojntrakool, Lalida Kongkiattikul, Eric Gumpricht
Journal of Nutrition and Metabolism.2022; 2022: 1. CrossRef - Prognostic value of phase angle and bioelectrical impedance vector in critically ill patients: A systematic review and meta-analysis of observational studies
Júlia Lima, Igor Eckert, Maria Cristina Gonzalez, Flávia Moraes Silva
Clinical Nutrition.2022; 41(12): 2801. CrossRef - Bioelectrical Impedance Analysis for Prediction of Early Complications after Gastrectomy in Elderly Patients with Gastric Cancer: the Phase Angle Measured Using Bioelectrical Impedance Analysis
Byunghyuk Yu, Ki Bum Park, Ji Yeon Park, Seung Soo Lee, Oh Kyoung Kwon, Ho Young Chung
Journal of Gastric Cancer.2019; 19(3): 278. CrossRef
- Optimal Enteral Nutrition Support Preserved Muscle Mass in Critically Ill Children
- 3,798 View
- 20 Download
- 3 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


