Abstract
-
Purpose
This study aimed to investigate the current perioperative nutritional practices and attitudes among gastrointestinal (GI) oncologic surgeons in Korea. Evidence-based perioperative nutritional practices are not well-established in this field.
-
Methods
A nationwide survey was conducted with 24 items, targeting GI oncologic surgical faculty members from March 2022 to April 2022 through social networking service messaging and email. Whole target number was 3,421.
-
Results
Out of responding 161 GI surgeons, 83.9% were male and 16.1% were female, and about 49.7% were in their 40s. When asked about their hospital policies, 67.1% reported the existence of formal nutritional screening programs. However, the execution and analysis of these programs varied considerably. Most surgeons conducted preoperative nutritional screening, with albumin testing the most frequently performed. In addition, nutritional supplementation—primarily protein drinks—was given before surgery. The duration for which these supplements were used varied from ≤3 days to 4–7 days. Most respondents recognized the importance of addressing nutritional deficiencies in patients with GI tumors; however, when asked about immunonutrition, 89.4% of surgeons admitted having limited knowledge.
-
Conclusion
Although there is recognition of the importance of evidence-based nutrition practices in GI and oncologic surgery programs, this study reveals limited implementation of such practices. This study highlights a considerable opportunity to leverage existing positive surgeon beliefs and published data on the benefits of perioperative nutrition to enhance surgical nutrition practices and to improve patient outcomes in Korea.
-
Keywords: Malnutrition; Neoplasms; Nutrition assessment; Republic of Korea; Surveys and questionnaires
Introduction
Background/rationale
Nutritional status plays a crucial role in the surgical outcomes of patients. Adequate nutrition is essential for maintenance of optimal health, and surgical procedures can place significant stress on the body. The nutritional status of a patient has a significant impact on the outcome of surgical interventions, including postoperative complications, length of hospital stay, and mortality rates [
1]. Malnutrition can impair the immune system, delay wound healing, and increase the risk of infection, prolonging hospitalization and leading to poor surgical outcomes. Several studies have demonstrated the importance of optimizing a patient’s nutritional status before surgery to reduce the risk of complications and to improve postoperative outcomes [
2-
4]. In surgical oncology, proper nutritional evaluation is essential to ensure that patients have the necessary energy, protein, and micronutrient stores to tolerate the stress of surgery and to support the healing process [
5]. Appropriate nutritional therapy in gastrointestinal (GI) oncologic patients, who often demonstrate malnutrition before and after surgery, has a positive effect on the surgical outcome [
6,
7]. In a survey study of European medical centers, 80% of institutions recognized that perioperative nutritional support reduced surgical complications and 59% acknowledge an effect on hospital stay, but only 20% of them implemented routine nutritional screening [
8]. GI oncology surgeons in Korea are expected to show interest in the nutritional status of patients before and after surgery. However, there are no data on perioperative nutritional screening and intervention in GI oncologic patients in Korea.
The aim of this study was to investigate the perioperative nutritional screening, awareness, and performance of nutritional support for Korean gastroenterological oncology surgeons who have seen many patients with malnutrition. Based on this survey, the overall awareness of surgeons on perioperative nutritional evaluation and nutritional support in Korea and the current status of implementation by institutions were identified, and treatment guidelines for nutritional evaluation and nutritional support for domestic surgical patients could be prepared.
Methods
Ethics statement
The Samsung Medical Center Intuitional Review Board approved this study (No. SMC 2022-01-124). Obtainment of the informed consent was waived.
Study design
Setting
A survey of 3,421 members of the Korean Society of Surgical Metabolism and Nutrition, the Korean Gastric Cancer Association, the Korean Association of Hepato-Biliary-Pancreatic Surgery and the Korean Society of Coloproctology was completed through social networking service (SNS) messaging and email from March 2022 to April 2022.
Participants
A total of 3,421 SNS messages and emails were sent, and 171 responses were received. We excluded 10 responses that were either duplicates or provided by doctors who did not perform GI surgery, leaving 161 participants for analysis.
Variables
Survey questionnaire items are outcome variables.
Data sources/measurement
A questionnaire with 24 evaluation items developed by the Colorado Clinical and Translational Sciences Institute (CCTIS) [
9] was translated into Korean and used after adding the contents of the questionnaire (
Supplement 1). The Korean language questionnaire was reviewed for validity by five executives of the Korean Society of Surgical Metabolism and Nutrition. Concerning perioperative nutrition, the following three categories were evaluated: (1) local nutritional screening practices; (2) nutritional supplementation practices; and (3) attitudes toward nutrition practice improvement barriers and evidence [
9-
11]. Reliability of the orignial measurement tool could not be calculated due to complicated scale structure.
The proportion of final inclusion is 0.0467 (161 out of 3,421) and it is not a randomized sampling; therefore, there may be selection bias.
Study size
Sample size estimation was not done because all respondents were included.
Statistical methods
A descriptive statistics were applied.
Results
Participants’ demographics
Of the 161 survey participants, 135 (83.9%) were male and 26 (16.1%) were female. Additionally, 44 (27.3%) were <40 years of age, 80 (49.7%) were in their 40s, and 37 (23.0%) were ≥50 years of age. There were 138 GI surgical specialists (85.7%) and 23 GI fellows (14.3%) among the respondents. In total, 68 surgeons worked in general hospitals (42.2%) and 93 worked in tertiary referral hospitals (57.8%). There were 35 hepatobiliary specialist surgeons (21.7%), 66 colorectal specialist surgeons (41.0%), and 60 upper GI surgeons (37.3%). Finally, the number of annual GI oncologic surgeries per hospital was <400 cases according to 87 respondents (54.0%) and ≥400 cases according to 74 respondents (46.0%).
Characterization of practice and nutritional screening
Our survey results revealed that approximately two-thirds of represented hospitals are conducting nutritional screening programs. One hundred eight surgeons (67.1%) answered that their hospital has formal nutritional screening programs. Among those working in tertiary hospitals, 65 (69.9%) answered that there was a formal nutritional screening program, and 43 working in general hospitals (63.2%) responded that there was a formal nutritional screening program. There was no statistically significant difference between the two groups (P=0.320).
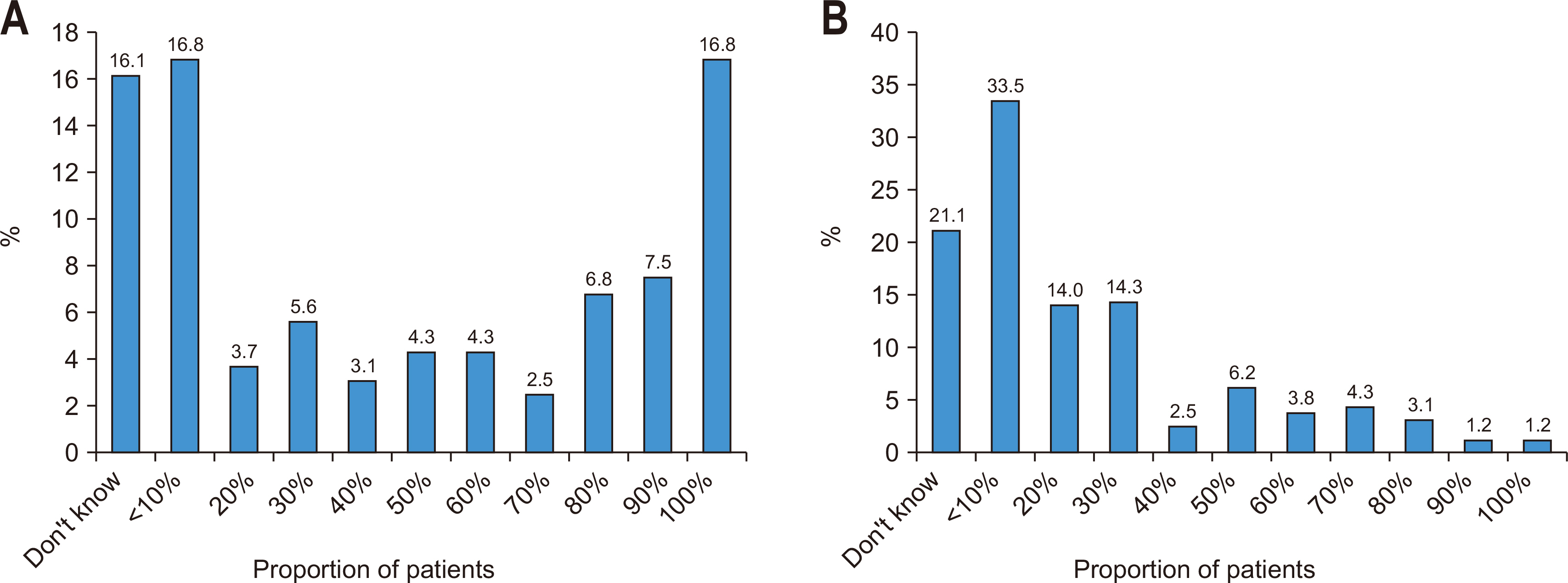
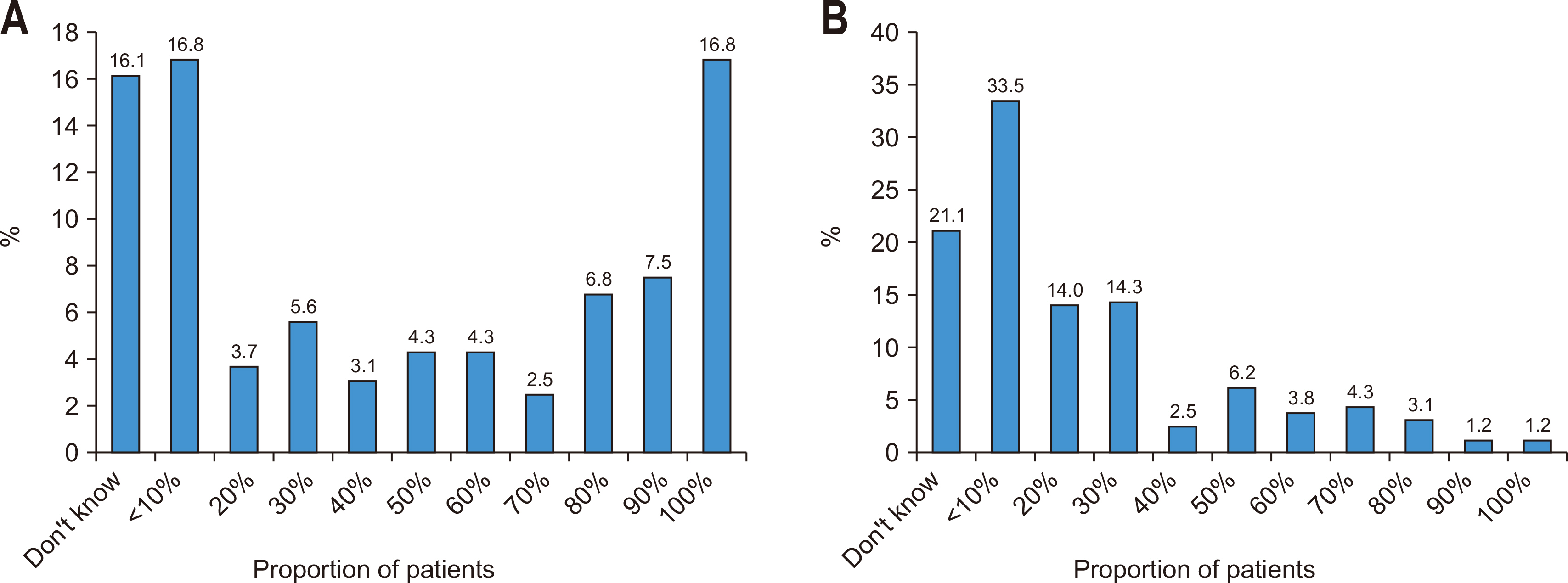
The survey data illustrated varying practices concerning preoperative nutritional screening among surgeons. For example, 16.8% of the surgeons carried out screenings of all their patients. In addition, a significant proportion, about 39.7%, reported performing screenings of at least half of their patients. In contrast, >30% of the surgeons either conducted screenings on <10% of their patients or were not interested in the percentage of patients undergoing these screenings.
The survey further revealed the practice of preoperative nutritional supplementation among surgeons treating patients undergoing GI tumor surgery. It was found that 33.5% of surgeons provided nutritional supplementation to <10% of their patients. Notably, 21.1% of surgeons seemed disinterested in nutritional supplementation and were unable to provide any estimates. On the other hand, 14.3% and 14.0% of surgeons administered supplementation to 30% and 20% of their patients, respectively. Only a small fraction, about 1.2%, provided nutritional supplementation to all their patients (
Fig. 1).
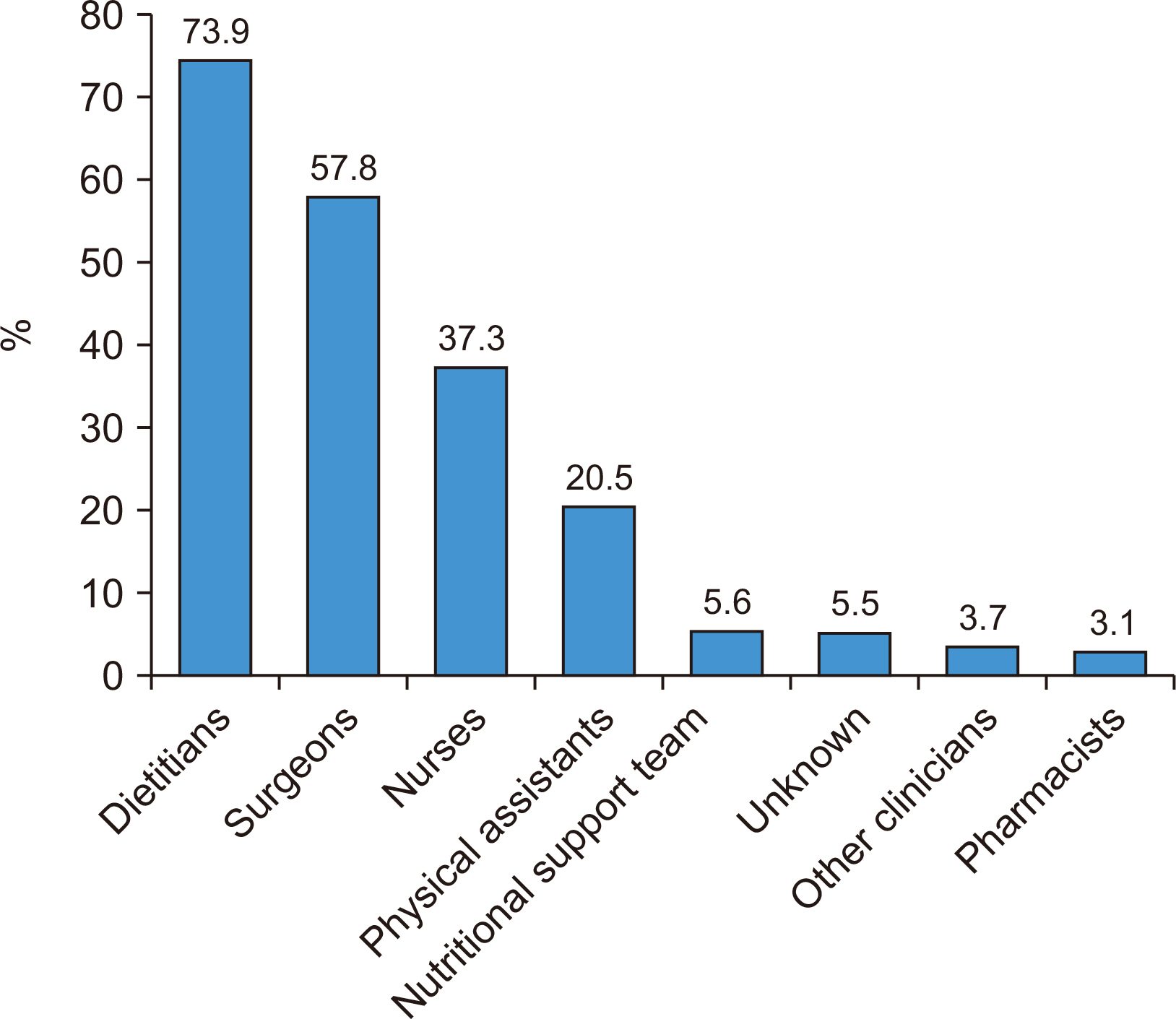
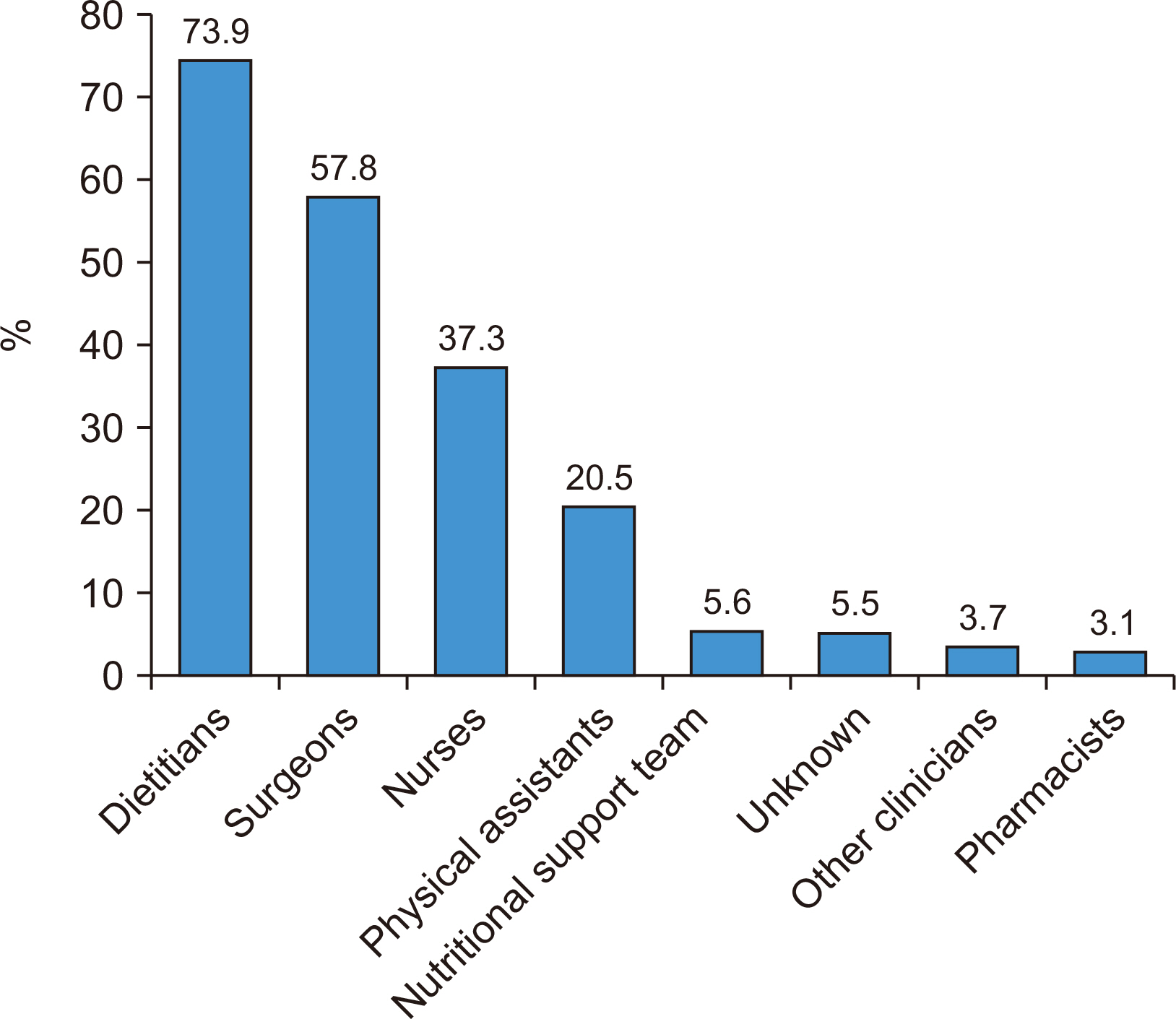
Perioperative nutritional evaluation was predominantly carried out by dietitians (73.9%), followed by surgeons (57.8%), nurses (37.3%), and physical assistants (20.5%). In smaller proportions, the nutritional support team (5.6%) and those who were either unaware or did not have anyone specifically assigned to perform nutritional assessment (5.5%) were responsible. Less frequently, other clinicians (3.7%) and pharmacists (3.1%) carried out the assessment (
Fig. 2).
Perioperative nutritional evaluation was performed in 91.3% of all cases. In the group that performed nutritional evaluation, 38.8% performed it only before surgery and 48.3% performed it both before and after surgery, while 12.9% did so only after surgery. In 4.5% of cases, nutritional screening was not conducted at all.
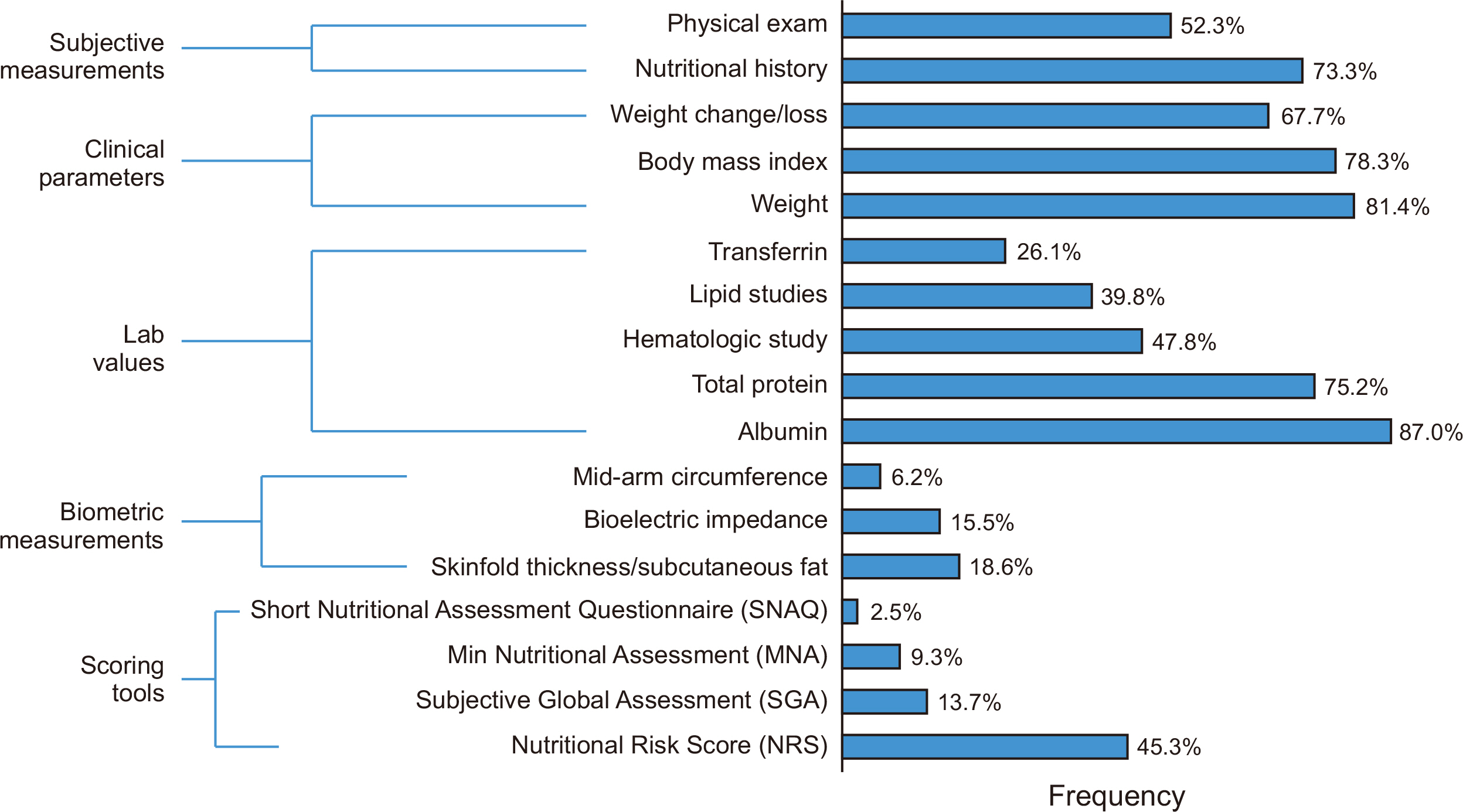
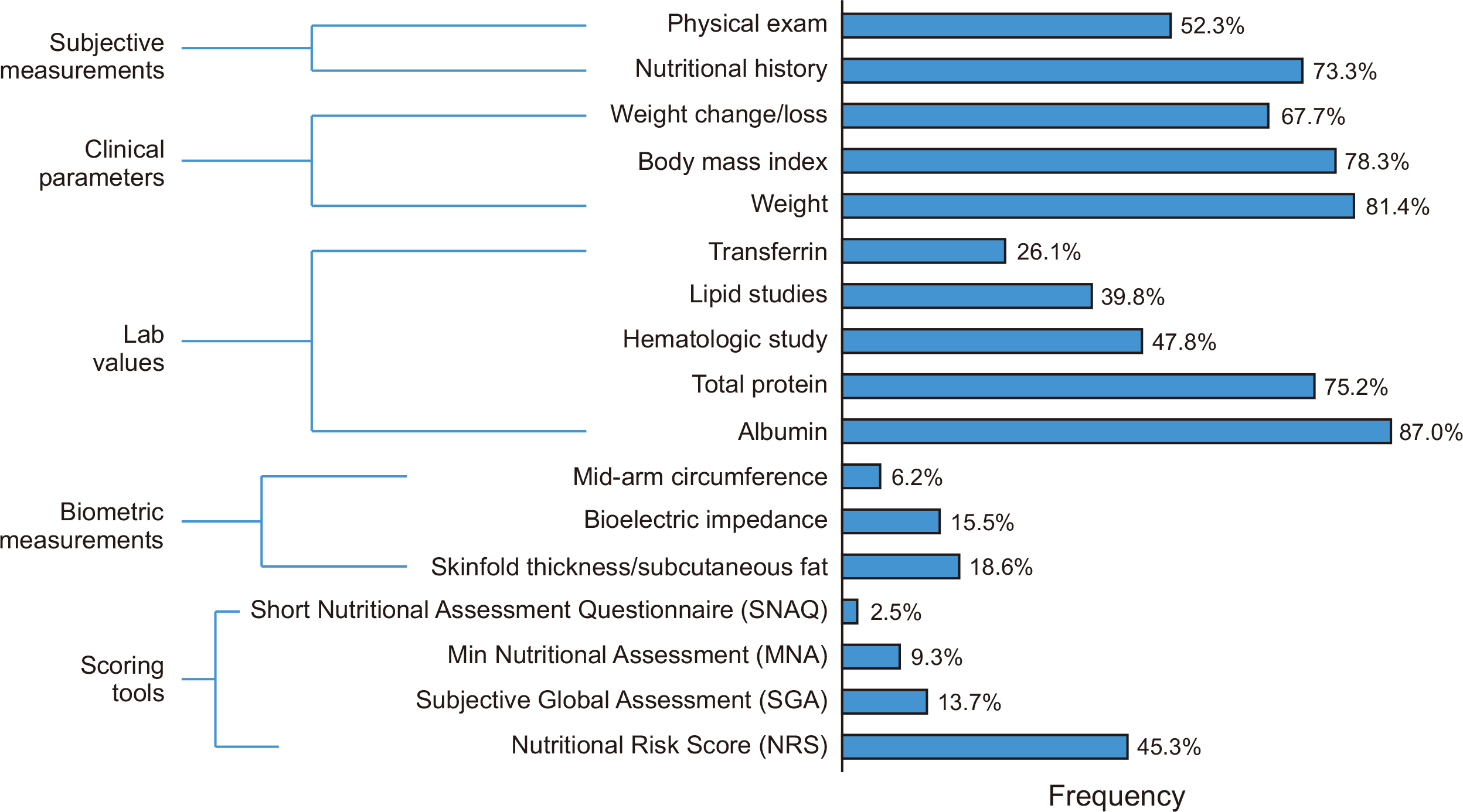
In nutritional screening, clinical parameters, subjective measures, and laboratory values are commonly used, with albumin being the most frequently used nutritional evaluation indicator. Biometric measurements and nutritional scoring systems are relatively less frequently used (
Fig. 3).
In terms of preoperative nutritional supplementation, protein drinks were the most commonly used method by surgeons. However, 29.2% of surgeons reported not using any nutritional supplementation in malnourished patients prior to surgery, with 48.9% of this group stating they had no intentions to use them in the future. Concerning the timing of nutritional supplementation, the majority (70.8%) preferred to conduct it postoperatively on the surgical ward. On the other hand, 9.7% of surgeons did not administer any supplementation, and 40% of them had no plans to initiate this in the future. Next, focusing on the duration of preoperative nutritional supplementation usage, 35.4% of surgeons administered supplements for a period ≤3 days, while 35.4% continued supplementation for 4–7 days. For monitoring of supplementation efficacy, laboratory values were most frequently used, by 58.4% of surgeons. However, 20.5% did not perform any monitoring (
Table 1).
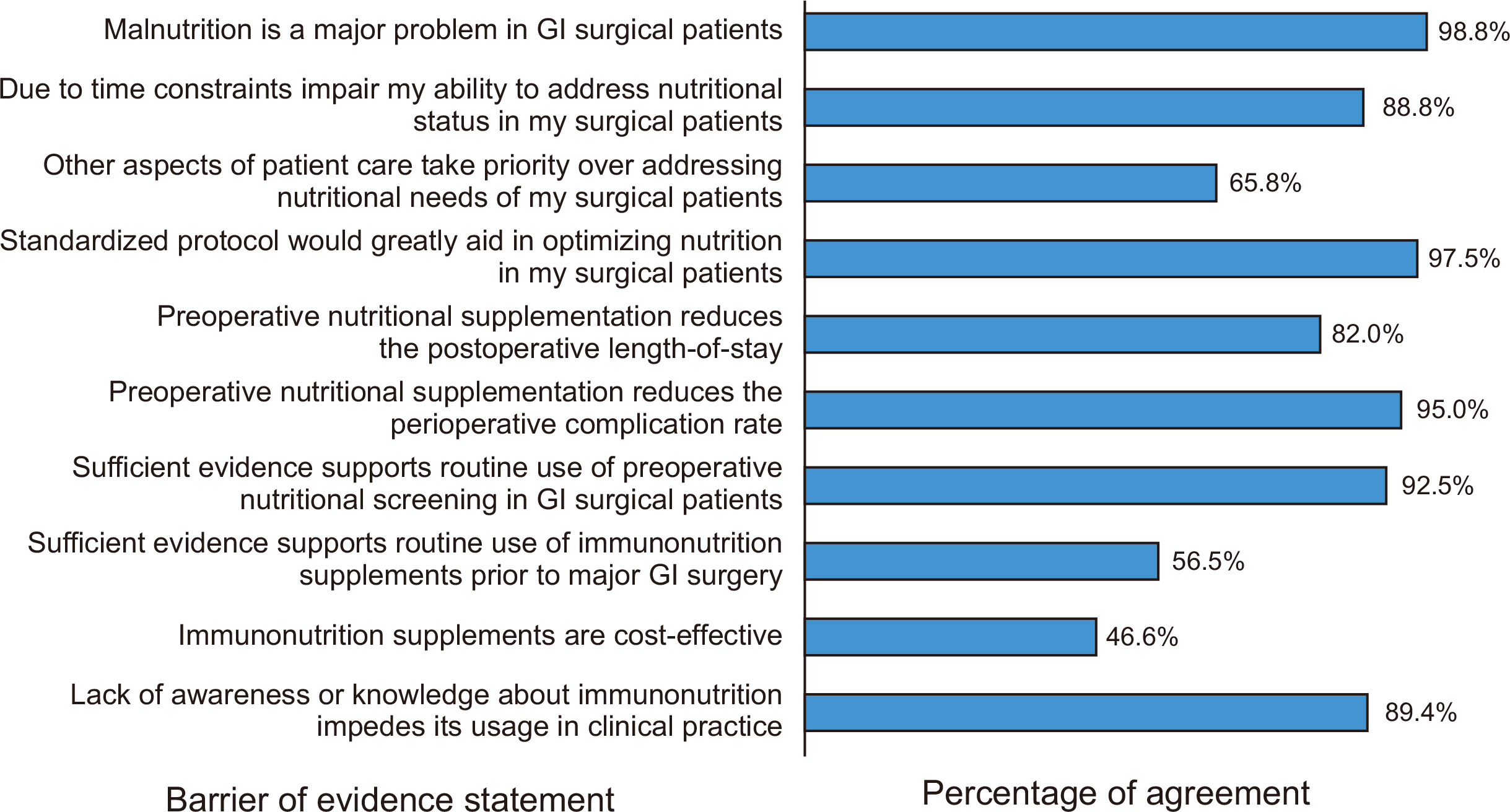
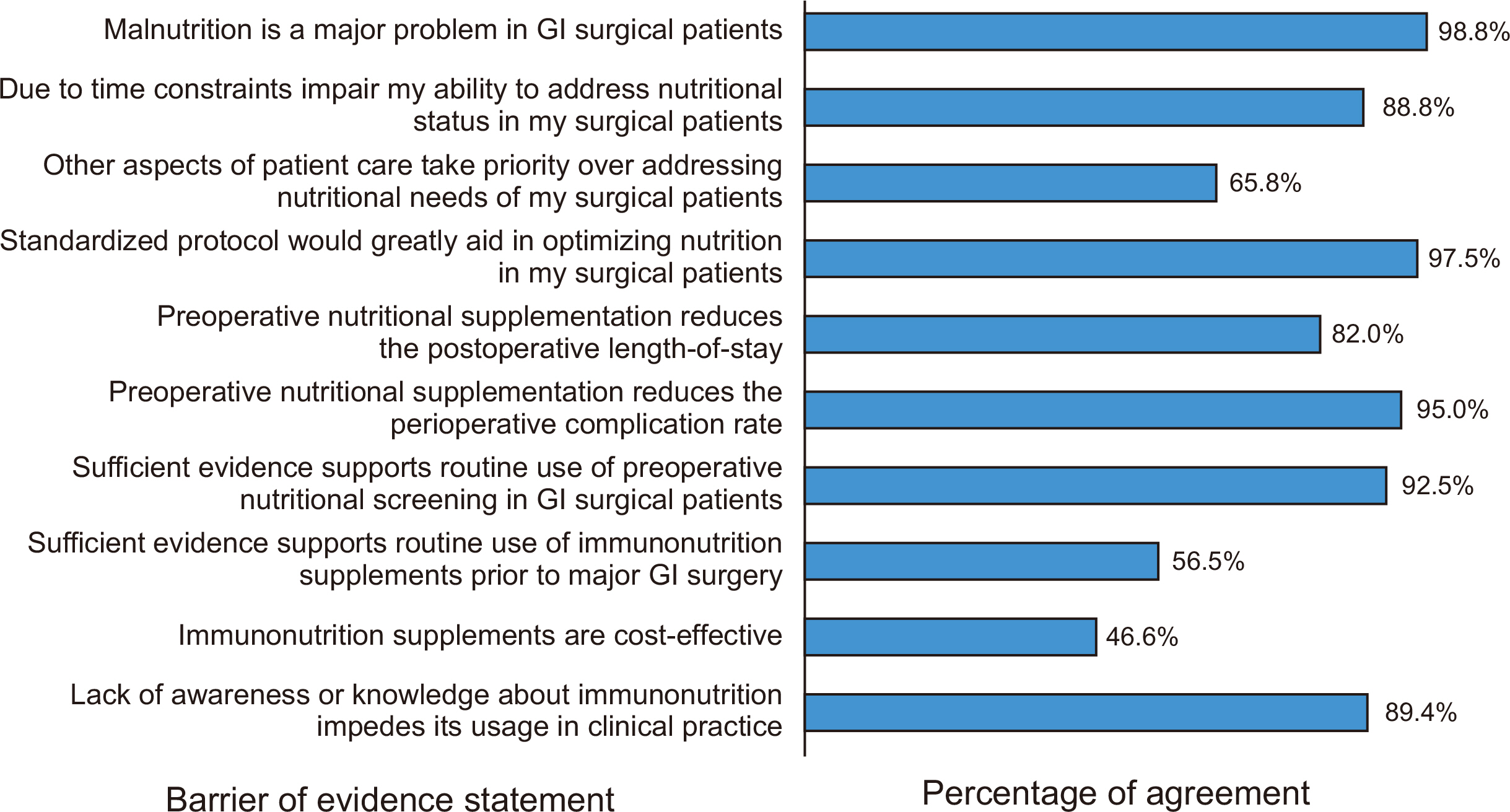
The survey revealed that nearly all physicians (98.8%) consider malnutrition a significant issue for patients undergoing GI surgery. However, 88.8% of these physicians indicated that their ability to address the nutritional status of their surgical patients is often compromised due to time constraints. Other aspects of patient care were also noted to take precedence over nutritional needs, as suggested by 65.8% of the respondents. A vast majority, 97.5% of physicians, underscored the potential benefits of a standardized protocol for optimizing nutrition in surgical patients. The belief that preoperative nutritional supplementation can reduce the postoperative length of stay was held by 82.0% of physicians, while 95.0% affirmed it could decrease the perioperative complication rate. Despite these beliefs, certain issues demonstrated less consensus. Although 92.5% of physicians agreed that there is sufficient evidence to support routine use of preoperative nutritional screening in GI surgical patients, only 56.5% endorsed the routine use of immunonutrition supplements prior to major surgery. Immunonutrition supplements were considered cost-effective by only 46.6% of the respondents. Moreover, 89.4% of the surveyed physicians admitted that a lack of awareness or knowledge about immunonutrition limits its application in clinical practice (
Fig. 4).
Discussion
Key results
A key finding of the study is that, despite the majority of surgeons recognizing the importance of malnutrition, which affects a staggering 98.8% of GI surgical patients, there is limited adoption of standardized nutritional protocols and preoperative supplementation in the Korean medical setting.
Interpretation/comparison with previous studies
In this groundbreaking national survey examining perioperative nutritional practices and attitudes among GI oncologic surgeons in Korea, several significant findings were revealed. This study is particularly significant as it is the first of its kind to be conducted in Korea, while previous research on this topic has been centered in the United States [
9]. Our results indicate that most hospitals in Korea (67.1%) implement formal nutritional screening programs, with no significant difference observed between tertiary hospitals and general hospitals. However, a minority of GI oncologic surgeons in Korea demonstrated limited interest in nutritional screening or did not perform it at all. In addition, 33.5% of surgeons provided nutritional supplementation to <10% of their patients, suggesting that not all patients require nutritional supplementation, but that the percentage of patients receiving supplementation is low. Studies conducted in the United States have demonstrated a higher implementation rate of nutritional protocols and preoperative supplementation [
9]. The discrepancy in practice could be attributed to a lack of awareness or knowledge about general nutritional screening and supplementation, including both regular nutrition and immunonutrition, among Korean surgeons. However, the studies conducted in the United States primarily focused on physicians involved in training academic fellowship programs, which might have led to higher interest and implementation rates of nutritional screening and supplementation among the targeted population [
9]. Based on our study, despite the widespread presence of nutritional screening programs in Korean hospitals, there remains a gap in optimal nutritional screening and supplementation given the high prevalence of malnutrition in GI surgical patients.
Our study findings indicate that, in the Korean context, dieticians are primarily responsible for conducting nutritional screenings, followed by surgeons. However, there is significant participation by paramedical personnel, particularly dietitians, in these screenings. This is an interesting departure from practices in other countries; studies from the United States and Europe, for example, often report a more centralized role for dietitians and nutritional support teams in the preoperative nutritional screening process [
12,
13]. Despite the differences in approach, involvement of multiple healthcare professionals in nutritional screening could contribute to a more comprehensive understanding of the patient’s nutritional status. By integrating the perspectives of different specialists, this multidisciplinary approach can potentially optimize patient outcomes, as each professional brings unique insights and expertise [
14]. While surgeons play an important role, dietitians have a larger role in nutritional screening in Korea. This seems to reflect the unique healthcare realities in the country. Given the high patient load and the pressing nature of GI oncologic conditions, surgeons might be best positioned to undertake this crucial task swiftly and efficiently. However, it is also important to consider the potential limitations of this approach. Although surgeons are undoubtedly highly skilled, their primary training and focus do not involve nutrition. This could potentially lead to gaps in nutritional screening and the potential for patient malnutrition [
15]. In light of these considerations, the Korean system appears to have adopted a pragmatic approach to perioperative nutritional screening. While it may not strictly adhere to the models followed in other countries, the Korean system seems to function effectively within its unique healthcare context.
Albumin was the most frequently used indicator for nutritional evaluations. While this biomarker is commonly used in nutritional screening, there are some challenges related to its utilization [
16]. For instance, albumin level may be influenced by factors other than nutrition, such as inflammation or liver function. Therefore, relying solely on albumin for nutritional screening may not provide a complete picture of a patient’s nutritional status [
17]. Notably, our survey revealed that more than half of the surgeons were not interested in or provided nutritional supplementation to <10% of their patients. This trend could possibly be attributed to a lack of understanding of the role of nutrition in surgical recovery [
10], an underestimation of the prevalence of malnutrition in surgical patients [
18], or concerns regarding the cost-effectiveness of supplementation [
19]. A substantial portion of the surgeons (40%) who did not provide perioperative nutritional supplementation indicated no intention of beginning to offer such in the future. This underscores the need for further education and institutional protocols to ensure that all surgeons recognize the value and necessity of perioperative nutritional support. Nutritional deficiency before surgery can lead to poorer surgical outcomes, including increases in morbidity, mortality, and hospital stay [
10]. Preoperative supplementation, particularly with specialized immunonutrition, has been shown to decrease postoperative complications in malnourished GI cancer patients [
1]. Despite the apparent benefits, our study reveals a reluctance to incorporate these findings into practice, which reflects similar trends observed in other studies [
20]. The survey also revealed that a significant portion of surgeons do not track the success of nutritional supplementation. Monitoring the efficacy of supplementation, through means such as clinical parameters, is crucial to assess and adapt the nutritional plan as needed [
21]. The lack of follow-up is indicative of the larger problem of recognizing nutrition as a critical aspect of perioperative care. These findings suggest a need for further education and institutional policy changes. Raising awareness and understanding about the importance of nutrition in surgical care among surgeons and implementing standardized protocols for nutritional screening and supplementation could address the issues highlighted in our study [
22-
25]. Our results showed that, despite the recognition of malnutrition as a significant issue in GI surgical patients by a majority of physicians, barriers such as time constraints and prioritization of other aspects of patient care hinder effective management of this issue. There is a strong consensus on the potential benefits of standardized nutritional protocols. Most physicians believe in the positive impact of preoperative nutritional supplementation on reducing the postoperative length-of-stay and perioperative complication rate. However, less than half of the respondents consider immunonutrition supplements to be cost-effective, and a significant majority reported a lack of knowledge about these supplements. These findings underscore the need for further education and policy changes to improve nutritional care in the perioperative setting. These findings are consistent with findings of similar surveys conducted in the United States [
9].
The number of respondents is not enough and it is not a randomized study; therefore, a larger size randomized sampling is required for further studies.
Generalizability
It may be a status in Korea, but is it challenging to generalize the results to other countries.
Conclusion
Our survey findings highlight areas that could benefit from more attention and consideration in nutritional screening and supplementation among GI oncology surgeons in Korea. Even with the existence of formal screening programs, there appears to be room for improvement in awareness and interest. Additional challenges include time constraints and competing care priorities. Less than half of our survey respondents consider immunonutrition supplements to be cost-effective, with many admit a lack of knowledge about them. These findings suggest the need for further educational interventions, increased awareness, and the development of standardized protocols to better integrate nutritional care into perioperative practice.
Supplementary materials
Supplement 1. Survey questionnaire for the measurement on the perioperative nutritional practices and attitudes for gastrointestinal oncology surgeons (in Korean).
Acknowledgments
None.
Authors’ contribution
Conceptualization: JMS, MGC. Data curation: MGC, DHK. Formal analysis: DHK. Funding acquisition: JMS, MGC. Investigation: DHK. Methodology: JMS, MGC. Project administration: MGC. Resources: JMS, MGC. Software: DHK. Supervision: JMS. Validation: JMS, MGC. Visualization: DHK. Writing – original draft: MGC, DHK. Writing – review & editing: all authors.
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Funding
This study received financial support from the Korean Society of Surgical Metabolism and Nutrition.
Data availability
Contact the corresponding author for data availability.
Fig. 1(A) The proportion of patients with gastrointestinal tumors undergoing nutritional screening. (B) The proportion of patients with gastrointestinal tumors receiving nutritional support.
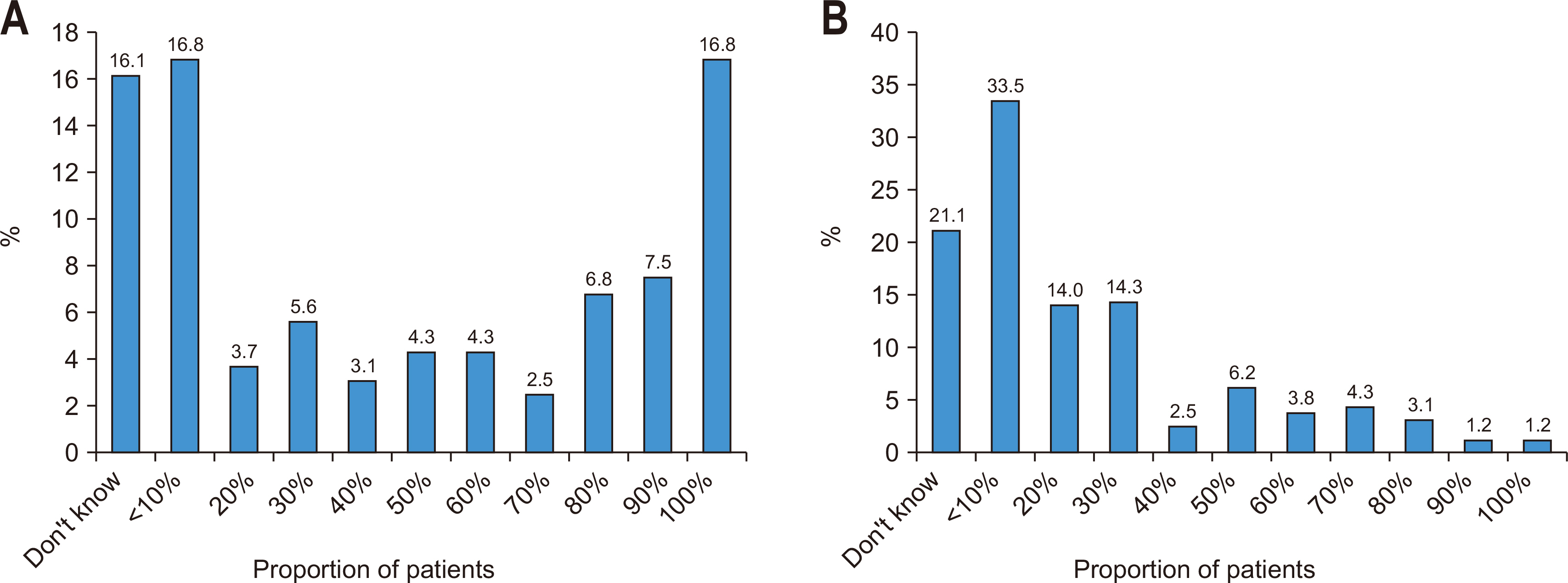
Fig. 2Director of nutrition screening is responsible for nutritional screening in clinical practice based on the frequency of each representative selected by respondents responsible for nutritional screening.
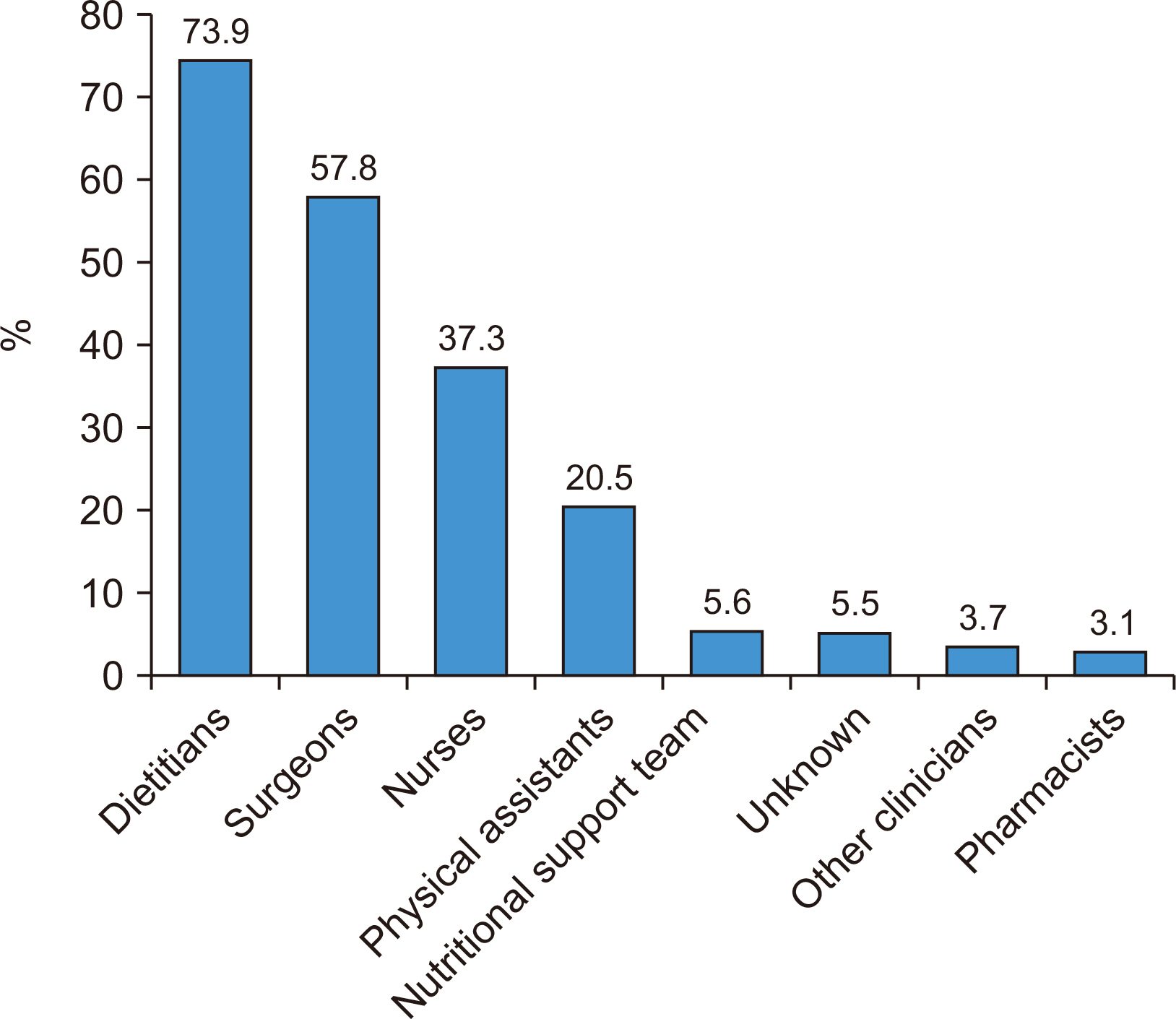
Fig. 3Nutritional screening methods used to conduct nutrition testing in clinical practice are presented as the frequency of each method selected by survey respondents.
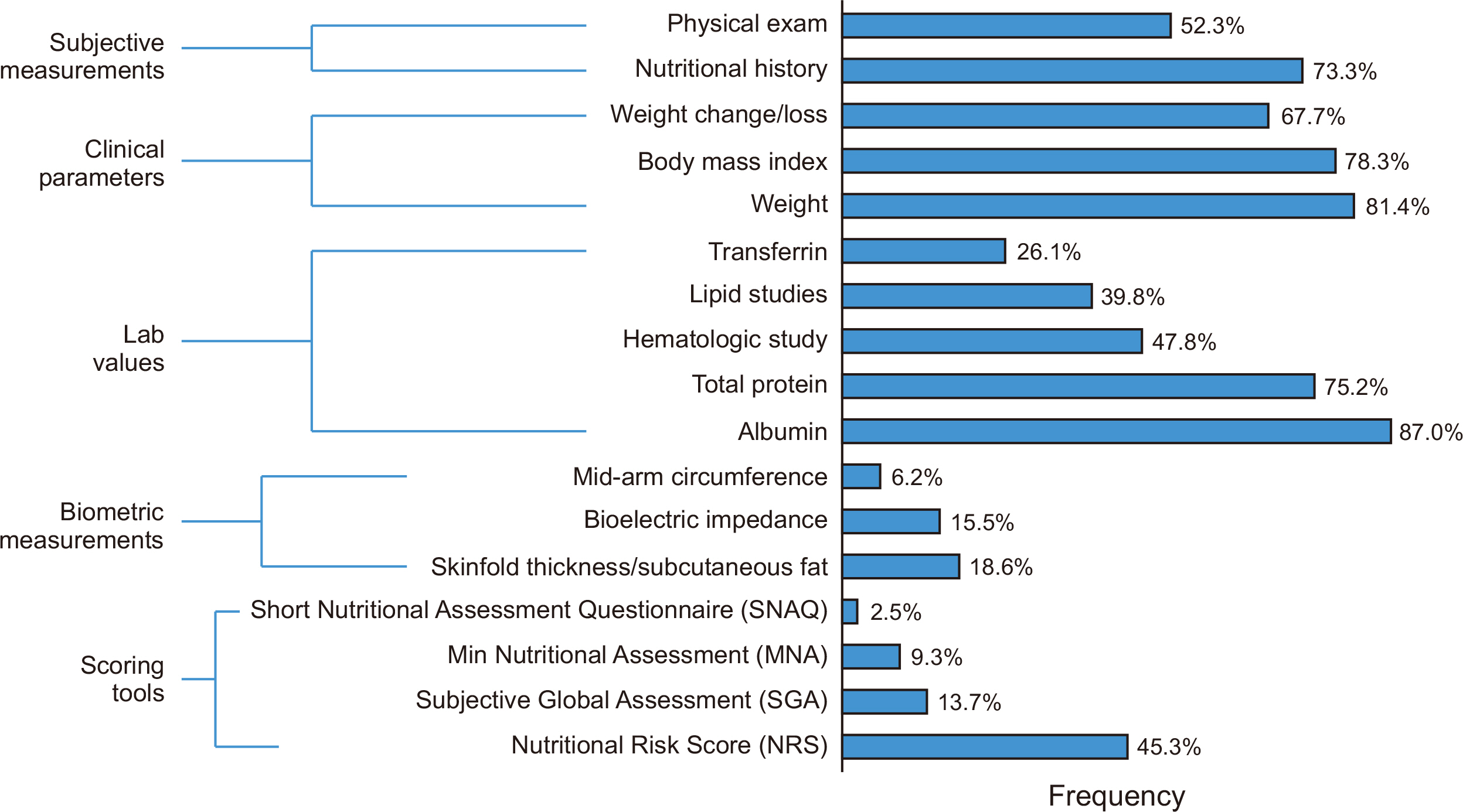
Fig. 4
Screening of gastroenterological surgeons’ attitudes and barriers to the use of immunonutrition supplementation.
GI = gastrointestinal.
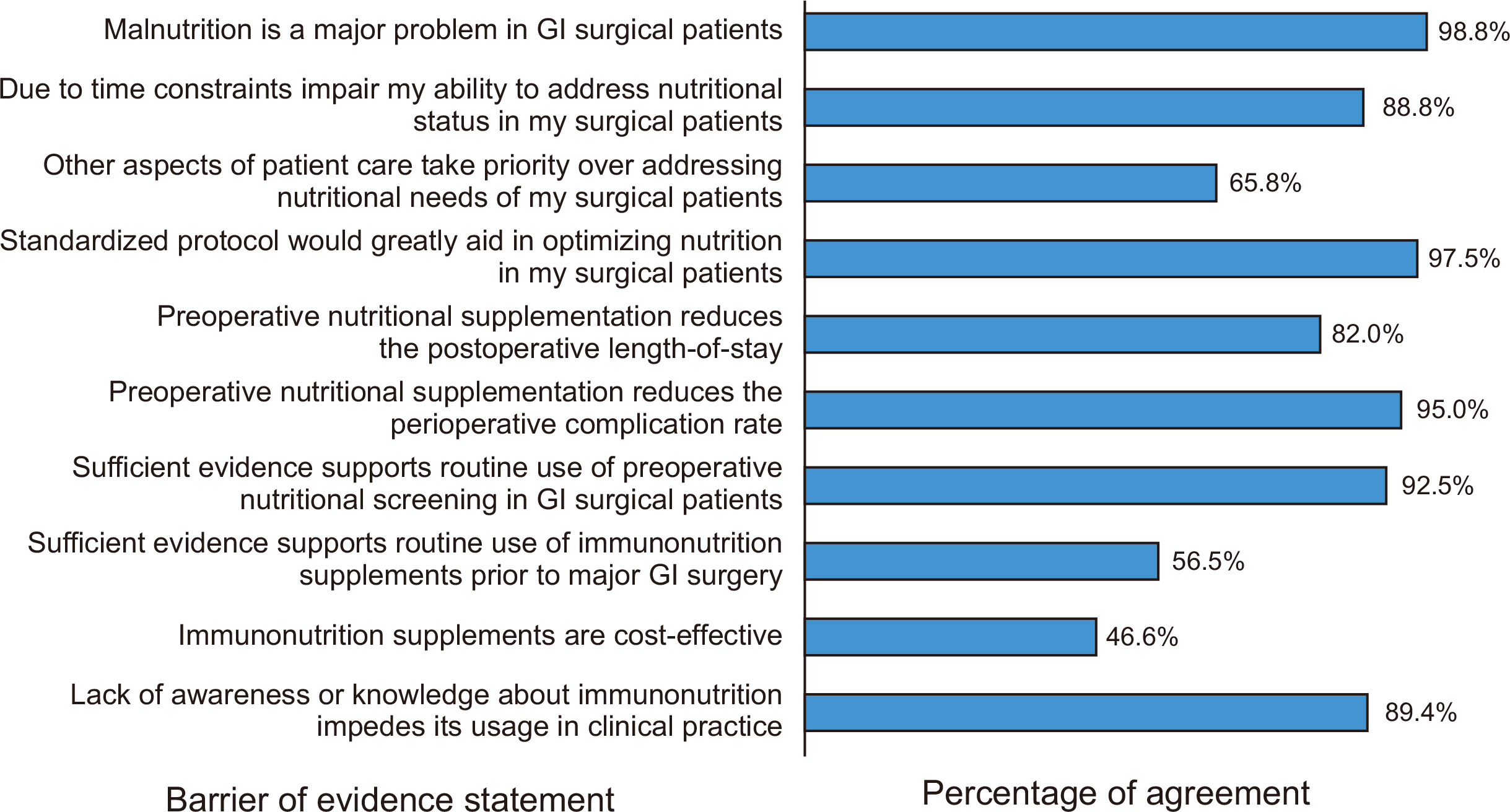
Table 1Description of nutritional supplementation practices when supplemental nutrition is implemented
|
What supplements are used preoperatively? |
When are supplements given? |
Duration of preoperative supplements |
How is supplementation efficacy monitored? |
|
Protein drinks: 54% |
Preoperatively in outpatient clinic: 10.4% |
≤3 days: 35.4% |
Clinical parameters: 51.6% |
|
Immunonutrition: 18.6% |
Preoperatively on the surgical ward: 65.6% |
4–7 days: 35.4% |
Physical exam: 36.6% |
|
Total parenteral nutrition: 6.2% |
Postoperatively on the surgical ward: 70.8% |
8–10 days: 1.9% |
Lab values: 58.4% |
|
No supplement used: 29.2% |
Postoperatively in the ICU: 10.4% |
≥11 days: 3.1% |
Nutritional or diary history: 36% |
|
Supplementation is not given: 9.7% |
No preoperative supplementation: 24.2% |
Biometrical measurement: 5.6% |
|
|
|
Success is not tracked: 20.5% |
References
- 1. Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-8. ArticlePubMed
- 2. Ho JW, Wu AH, Lee MW, Lau SY, Lam PS, Lau WS, et al. Malnutrition risk predicts surgical outcomes in patients undergoing gastrointestinal operations: results of a prospective study. Clin Nutr 2015;34:679-84. ArticlePubMed
- 3. Gallagher-Allred CR, Voss AC, Finn SC, McCamish MA. Malnutrition and clinical outcomes: the case for medical nutrition therapy. J Am Diet Assoc 1996;96:361-6. 369. quiz 367-8. PubMed
- 4. Golladay GJ, Satpathy J, Jiranek WA. Patient optimization-strategies that work: malnutrition. J Arthroplasty 2016;31:1631-4. ArticlePubMed
- 5. Ghaly P, Iliopoulos J, Ahmad M. The role of nutrition in wound healing: an overview. Br J Nurs 2021;30:S38-42. ArticlePubMed
- 6. Drover JW, Cahill NE, Kutsogiannis J, Pagliarello G, Wischmeyer P, Wang M, et al. Nutrition therapy for the critically ill surgical patient: we need to do better! JPEN J Parenter Enteral Nutr 2010;34:644-52. PubMed
- 7. Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L. Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr 2007;26:698-709. ArticlePubMed
- 8. Grass F, Cerantola Y, Schäfer M, Müller S, Demartines N, Hübner M. Perioperative nutrition is still a surgical orphan: results of a Swiss-Austrian survey. Eur J Clin Nutr 2011;65:642-7. ArticlePubMedPDF
- 9. Williams JD, Wischmeyer PE. Assessment of perioperative nutrition practices and attitudes-a national survey of colorectal and GI surgical oncology programs. Am J Surg 2017;213:1010-8. ArticlePubMed
- 10. Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, et al. ESPEN guideline: clinical nutrition in surgery. Clin Nutr 2017;36:623-50. ArticlePubMed
- 11. Mueller C, Compher C, Ellen DM. American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors. A.S.P.E.N. clinical guidelines: nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enteral Nutr 2011;35:16-24. PubMed
- 12. Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improving quality of care: an interdisciplinary call to action to address adult hospital malnutrition. JPEN J Parenter Enteral Nutr 2013;37:482-97. ArticlePubMed
- 13. Jensen GL, Mirtallo J, Compher C, Dhaliwal R, Forbes A, Grijalba RF, et al. International Consensus Guideline Committee. Adult starvation and disease-related malnutrition: a proposal for etiology-based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. JPEN J Parenter Enteral Nutr 2010;34:156-9. PubMed
- 14. Nicolo M, Heyland DK, Chittams J, Sammarco T, Compher C. Clinical outcomes related to protein delivery in a critically ill population: a multicenter, multinational observation study. JPEN J Parenter Enteral Nutr 2016;40:45-51. PubMed
- 15. Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 2019;38:1-9. PubMed
- 16. Goldwasser P, Feldman J. Association of serum albumin and mortality risk. J Clin Epidemiol 1997;50:693-703. ArticlePubMed
- 17. Fuhrman MP. The albumin-nutrition connection: separating myth from fact. Nutrition 2002;18:199-200. ArticlePubMed
- 18. Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 2009;35:1728-37. ArticlePubMedPDF
- 19. Elia M, Normand C, Norman K, Laviano A. A systematic review of the cost and cost effectiveness of using standard oral nutritional supplements in the hospital setting. Clin Nutr 2016;35:370-80. ArticlePubMed
- 20. Gillis C, Buhler K, Bresee L, Carli F, Gramlich L, Culos-Reed N, et al. Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology 2018;155:391-410.e4. ArticlePubMed
- 21. Hendifar AE, Petzel MQB, Zimmers TA, Denlinger CS, Matrisian LM, Picozzi VJ, et al. Precision Promise Consortium. Pancreas cancer-associated weight loss. Oncologist 2019;24:691-701. ArticlePubMedPDF
- 22. Williams DGA, Molinger J, Wischmeyer PE. The malnourished surgery patient: a silent epidemic in perioperative outcomes? Curr Opin Anaesthesiol 2019;32:405-11. PubMedPMC
- 23. Garth AK, Newsome CM, Simmance N, Crowe TC. Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J Hum Nutr Diet 2010;23:393-401. ArticlePubMed
- 24. Gianotti L, Braga M, Nespoli L, Radaelli G, Beneduce A, Di Carlo V. A randomized controlled trial of preoperative oral supplementation with a specialized diet in patients with gastrointestinal cancer. Gastroenterology 2002;122:1763-70. ArticlePubMed
- 25. Klek S, Szybinski P, Szczepanek K. Perioperative immunonutrition in surgical cancer patients: a summary of a decade of research. World J Surg 2014;38:803-12. ArticlePubMedPDF

 , Jeong-Meen Seo3
, Jeong-Meen Seo3 , Min-Gew Choi3
, Min-Gew Choi3


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN Cite
Cite

