Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
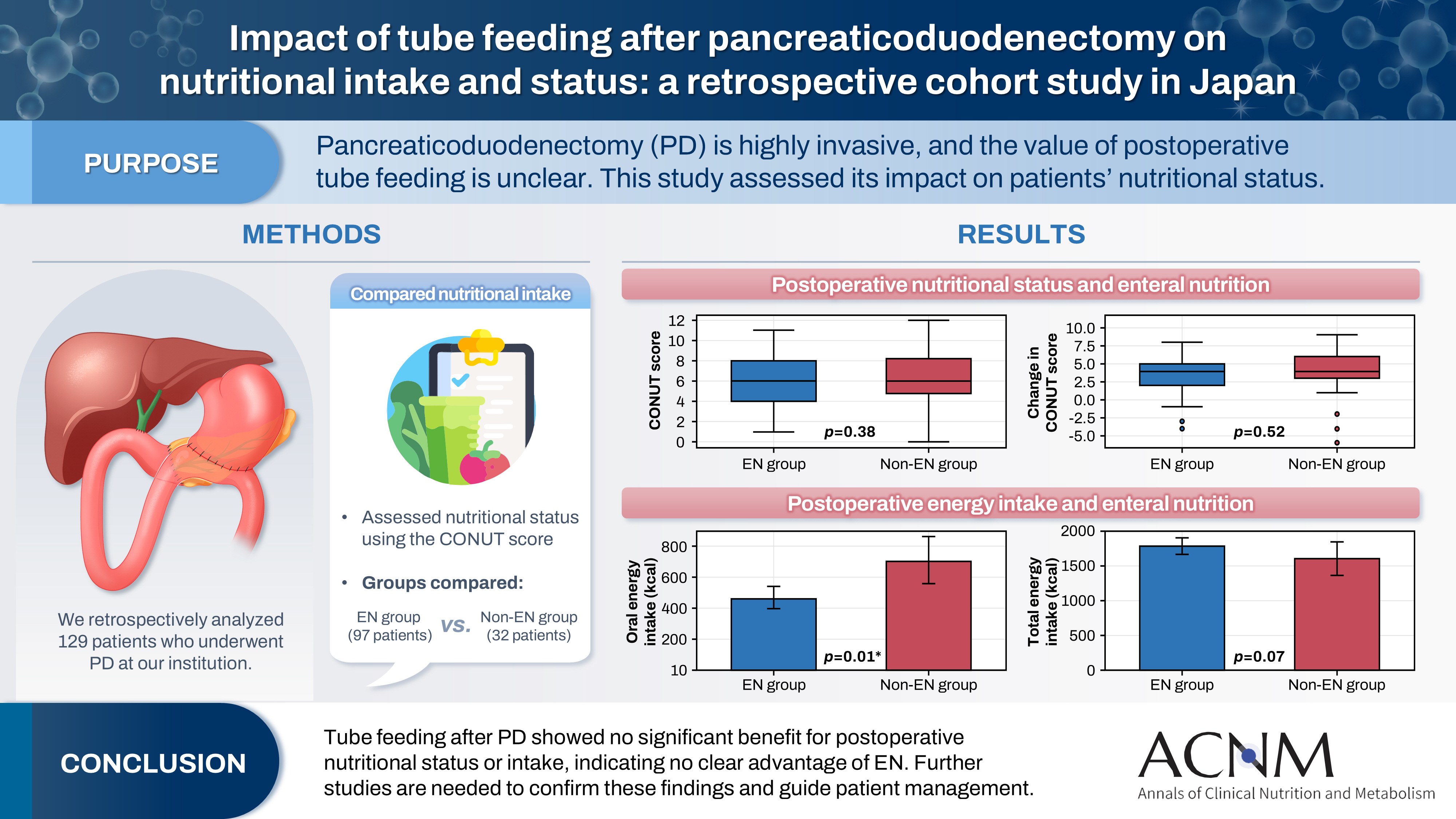
- Impact of tube feeding after pancreaticoduodenectomy on nutritional intake and status: a retrospective cohort study in Japan
- Masaharu Ishida, Masahiro Iseki, Shuichiro Hayashi, Aya Noguchi, Hideaki Sato, Shingo Yoshimachi, Akiko Kusaka, Mitsuhiro Shimura, Shuichi Aoki, Daisuke Douchi, Takayuki Miura, Shimpei Maeda, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(3):203-209. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0020
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 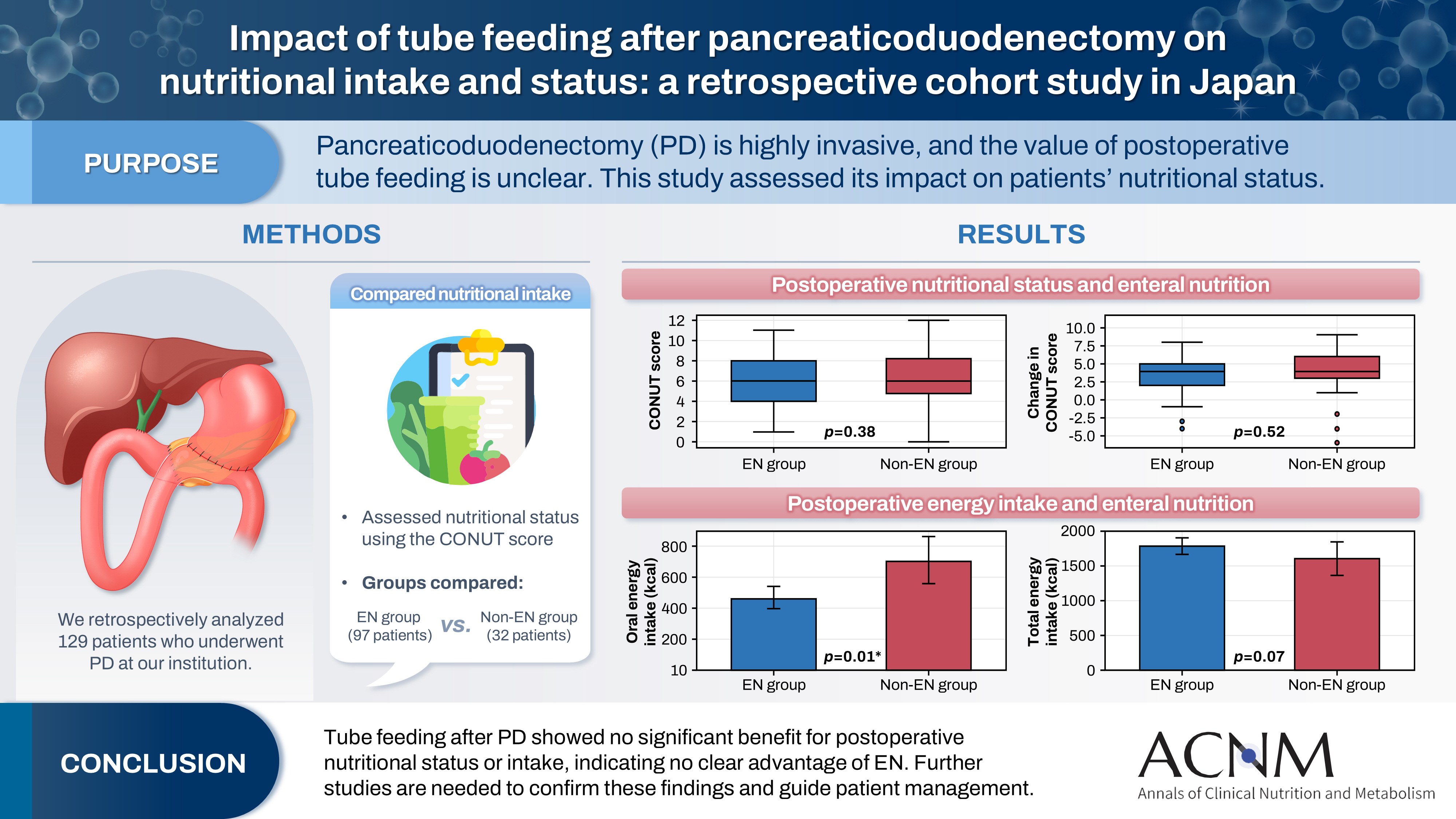
- Purpose
Pancreaticoduodenectomy (PD) is one of the most invasive procedures in gastrointestinal surgery. However, the clinical significance of postoperative tube feeding remains unclear. This study investigated the impact of enteral nutrition (EN) on the postoperative nutritional status of patients undergoing PD.
Methods
We retrospectively analyzed 129 patients who underwent PD at Tohoku University Hospital. Nutritional intake and status, evaluated using the Controlling Nutritional Status score, were compared between two groups: an EN group (97 patients) and a non-EN group (32 patients).
Results
There were no significant differences between the two groups in age, sex, body mass index, underlying diseases, operative duration, blood loss, postoperative pancreatic fistula, postoperative complications, delayed gastric emptying, or length of hospital stay. Although the EN group showed improvements in nutritional status both at discharge and compared with preoperative values, none of these changes reached statistical significance. Oral caloric intake was significantly higher in the non-EN group (P=0.01). In contrast, total energy intake was higher in the EN group, but this difference did not reach statistical significance (P=0.07).
Conclusion
Tube feeding after PD did not significantly influence postoperative nutritional status or overall nutritional intake. These findings suggest that EN offers no clear advantage over other approaches; however, further research is warranted to validate these results, refine existing guidelines, and optimize postoperative patient management.
- 401 View
- 9 Download

- Perioperative outcomes of older adult patients with pancreatic cancer based on nutritional status: a retrospective cohort study
- Takanori Morikawa, Masaharu Ishida, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(1):66-74. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.001
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study investigated the effects of preoperative nutritional status on postoperative outcomes in older adult patients with pancreatic adenocarcinoma.
Methods
The background and perioperative factors of patients who underwent pancreatectomy for pancreatic adenocarcinoma between 2007 and 2020 were retrospectively analyzed.
Results
Patients aged 75 years or over (older adults) were significantly associated with hypertension, upfront surgery, and lower prognostic nutritional index. In addition, these patients had a significantly lower rate of portal vein resection, less blood loss, and shorter operation time than patients aged less than 75 years (non-older adults). During the postoperative course, older adult patients had a higher rate of pneumonia and lower overall survival than younger patients, although recurrence‐free survival was comparable. In addition, older adult patients showed preoperative malnutrition as a risk factor for postoperative in‐hospital death.
Conclusion
Surgical treatment for pancreatic cancer in older adult patients was performed safely. However, preoperative malnutrition is a risk factor for in‐hospital death and such patients require nutritional support and less‐invasive surgery. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,833 View
- 23 Download
- 1 Crossref

- Effects of nutritional status and support on the survival of COVID-19 patients in a single tertiary-center intensive care unit in Korea: a case-control study
- Na Gyeong Lee, Hye Jin Kim, Ji Gyeong Kang, Do Hyeon Jeon, Mi Seung Kwak, So Hyun Nam
- Ann Clin Nutr Metab 2023;15(1):30-37. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose: It is important to understand the nutritional status of critically ill COVID-19 patients and to provide adequate associated support. We attempted to determine how nutritional status and the amount of nutritional support provided to critically ill patients affect their survival.
Methods: We retrospectively reviewed the medical records of patients admitted to the intensive care unit of Dong-A University Hospital between January and December 2021. We divided the patients into survivors and those who died during COVID-19 treatment and compared and analyzed their clinical parameters, nutrition-related indicators, nutritional status, and nutritional support.
Results: Of 70 patients reviewed, 57 survived. Mortality was higher in the older group (P=0.006). The patients who underwent ventilator, extracorporeal membrane oxygenation, or continuous renal replacement therapy showed higher mortality. Nutritional status at the time of admission and the nutritional requirements did not differ among patient groups. However, the actual amounts of calories (P<0.001) and protein (P=0.019) supplied were lower in the mortality group. Serum C-reactive protein level was higher (P=0.002) and serum albumin level was lower in those who did not survive (P<0.001) compared with surviving patients at discharge.
Conclusion: We did not determine whether the initial nutritional status of patients with COVID-19 affected their survival due to various factors associated with the severity of the disease. However, given the similarities between disease severity and nutritional status at the time of admission, our results indicate that adequate nutritional support can contribute to survival in critically ill COVID-19 patients with pneumonia. -
Citations
Citations to this article as recorded by- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
So Hyun Nam
Ann Clin Nutr Metab.2025; 17(2): 97. CrossRef - The association between enteral nutrition with survival of critical patients with COVID‐19
Maryam Gholamalizadeh, Zahra Salimi, Khadijeh Abbasi Mobarakeh, Zahra Mahmoudi, Shirin Tajadod, Mahdi Mousavi Mele, Farkhondeh Alami, Bojlul Bahar, Saeid Doaei, Sara Khoshdooz, Masoume Rahvar, Somayeh Gholami, Masoume Pourtaleb
Immunity, Inflammation and Disease.2024;[Epub] CrossRef
- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
- 2,678 View
- 6 Download
- 2 Crossref

- Comparison of Post-Operative Nutritional Status according to the Extent of Gastrectomy and the Reconstruction Method in Patients with Gastric Cancer
- Kyung Hwan Kim, Jong Hyuk Yoon, Geum Jong Song, Myoung Won Son, Sung Yong Kim, Moo Jun Baek, Moon Soo Lee
- Ann Clin Nutr Metab 2021;13(2):34-42. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.34
-
 Abstract
Abstract
 PDF
PDF - Purpose: Malnutrition is the main complication after gastrectomy and the degree may vary depending on the extent of resection. This study sought to help determine an appropriate type of resection and provide methods for addressing malnutrition after gastrectomy.
Materials and Methods: We retrospectively reviewed medical records of patients with gastric cancer who underwent radical resection at the Soonchunhyang University Cheonan Hospital between December 2012 and December 2013. A total of 100 patients were screened, and all patients were followed for 1 to 3 years. Among this group, 12 underwent total gastrectomy, 5 underwent proximal gastrectomy, 46 underwent distal gastrectomy with Billroth I anastomosis, and 37 with Billroth II anastomosis. The nutritional status assessment included body weight, body mass index, serum albumin, serum hemoglobin, vitamin B12, ferritin, and Nutritional Risk Index (NRI).
Results: Patients who underwent total gastrectomy had lower hemoglobin and vitamin B12 levels compared to patients who underwent distal gastrectomy. The NRI was statistically significantly lower in patients who underwent total gastrectomy than patients who underwent distal gastrectomy. Patients who underwent total gastrectomy had lower vitamin B12 than patients who underwent proximal gastrectomy till the second year after gastrectomy. Regarding postdistal gastrectomy reconstruction, there was no statistically significant difference between the Billroth I and Billroth II groups.
Conclusion: This study showed that patients who underwent total gastrectomy were more susceptible to malnutrition than those who underwent distal or proximal gastrectomy. Patients who undergo gastrectomy should be monitored carefully for nutritional status and given appropriate nutritional support in the post-operative period. -
Citations
Citations to this article as recorded by- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
Ji-Hyeon Park, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Jong Won Kim, Ki Bum Park, In Cho, Sun-Hwi Hwang, Dong-Wook Kim, Su Mi Kim, Seung-Wan Ryu, Seong Chan Gong, Pil Young Jung, Hoon Ryu, Sung Geun Kim, Chang In Choi, Dae-Hwan Kim, Sung-IL Choi, Ji
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 55. CrossRef
- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
- 3,174 View
- 11 Download
- 1 Crossref

- Nutritional Status of Patients with Hepatobiliary-Pancreatic Surgical Disease
- Sang Soo Eom, Yong Chan Shin, Chang-Sup Lim, In Woong Han, Woohyun Jung, Yoonhyeong Byun, Dong Wook Choi, Jin Seok Heo, Hongbeom Kim
- Surg Metab Nutr 2020;11(2):46-52. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study examined the nutritional status of patients with hepatobiliary-pancreatic diseases before surgery to establish basic reference data.
Materials and Methods: This study evaluated retrospectively 2,322 patients admitted for hepatobiliary-pancreatic surgery between 2014 and 2016 at four Korean medical institutions using the body mass index (BMI) score. The prognostic nutrition index (PNI) was calculated in patients diagnosed with malignant diseases.
Results: The mean BMI was 24.0 kg/m2 (range, 13.2~39.1 kg/m2). The patients were classified as low BMI (<21.5 kg/ m2, below 25 percentile), intermediate BMI (21.5~25.5 kg/m2), and high BMI (>25.5 kg/m2, above 75 percentile). There were significant differences in the age, sex distribution, ASA classification, type of hospitalization, biliary drainage, organ, and pathology diagnosis between the pairs among the low, intermediate, and high BMI groups. Among the three BMI groups, the complication rate of the low BMI group was highest (34.4% vs. 29.7% vs. 25.8% P=0.005). The median lengths of hospital stay in the low, intermediate, and high BMI groups were 9, 9, and 7 days, respectively (P<0.001). Multivariate analysis revealed the risk factors of the low BMI group to be a higher ASA classification, biliary drainage, pancreatic disease, and malignant disease. The group with PNI<45 had significantly longer hospital stays than the group with PNI≥45 (P<0.001).
Conclusion: Patients with a low BMI had a higher ASA classification, preoperative biliary drainage, pancreatic disease, and malignant disease. The low PNI group had significantly longer hospital stays than the high PNI group. Screening of the preoperative nutritional status is necessary for assessing the risk of malnutrition and its treatment. -
Citations
Citations to this article as recorded by- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
Hengwei Jin, Xu Sun, Chang Fu, Changqing Fan, Junhong Chen, Ziyu Zhang, Yibo Yang, Xiaoyu Fan, Ye He, Siyuan Yin, Kai Liu
Surgical Endoscopy.2025; 39(8): 5107. CrossRef
- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
- 1,243 View
- 18 Download
- 1 Crossref

- Recovery Pattern of the Nutritional Status after Surgical Treatment for Pancreatic Head Disease: Compared with Malignancy and Non-malignancy
- Eunjung Kim, Youngmin Han, Hongbeom Kim, Wooil Kwon, Sun-Whe Kim, Jin-Young Jang
- Surg Metab Nutr 2018;9(2):51-58. Published online December 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.2.51
-
 Abstract
Abstract
 PDF
PDF Purpose:
Malnutrition affects the clinical outcomes of pancreatic disease. On the other hand, the changes in the nutritional status stratified by malignant and non-malignant diseases after surgery still need to be determined. The aim was to confirm the changing nutritional status and clinical outcomes after a pancreatoduodenectomy according to malignant and non-malignant disease.
Materials and Methods:
Data were collected prospectively from 157 patients between 2009 and 2015. The nutritional status was classified as well-nourished, at-risk of malnutrition, and malnourished by a Mini Nutrition Assessment. The clinical outcomes were assessed using the postoperative complication, hospital stay, biochemical nutritional markers, and quality-of-life (QOL).
Results:
Preoperatively, the proportion of malnourished status in the malignant disease group (group B) were 66.7% and 33.3% in the non-malignancy group (group A). The malnutrition rate in group B was higher than that in group A at 3, 6, and 12 months after surgery (58.1% vs. 41.9%, 90.0% vs. 10.0, 77.8% vs. 22.2%, respectively). The preoperative QOL was significantly lower in group B than in group A (P<.001); however, the QOL was comparable between the two groups after surgery. The body mass index was unrecovered after surgery in all groups.
Conclusion:
Patients with malignant pancreatic disease are more likely to suffer from a poor nutritional status than those with non-malignant pancreatic disease. One year after the pancreatoduodenctomy, the at-risk of malnutrition and malnourished rate were found to be over 70% in all patients. Therefore, more efforts will be needed to improve the nutritional status in pancreatic head disease.
-
Citations
Citations to this article as recorded by- Factors Affecting Nutritional Index and Length of Stay in Pancreatic Cancer in the Older Adults
So Young Jun, Mo Na Choi, Joon Seong Park, Hyang Kyu Lee
Asian Oncology Nursing.2023; 23(3): 91. CrossRef
- Factors Affecting Nutritional Index and Length of Stay in Pancreatic Cancer in the Older Adults
- 914 View
- 3 Download
- 1 Crossref

- Analysis of Current Status and Predisposing Factors for Nutritional Support of Patients in Surgical Intensive Care Unit
- Byung Chul Kim, In Kyu Lee, Eun Young Kim
- Surg Metab Nutr 2016;7(2):32-38. Published online December 30, 2016
- DOI: https://doi.org/10.18858/smn.2016.7.2.32
-
 Abstract
Abstract
 PDF
PDF Purpose:
Enteral feeding is strongly recommended for critically ill patients since it can enhance the immunologic function, which serves as a host defense mechanism against inflammation or metabolic response to stress. Herein, we investigated nutritional status and estimated the adequacy of the nutritional supply for acutely ill patients admitted to the surgical intensive care unit (SICU) after a major operation.
Materials and Methods:
From February to October 2016, patients admitted and stayed over 48 hours after major surgical procedures at SICU in Seoul St. Mary’s Hospital were reviewed. The nutritional parameters and surgical outcomes were compared according to the status of nutritional support.
Results:
A total of 220 patients composed of 130 males (59.1%) and 90 females (40.9%) were enrolled, and mean age was 61.4±13.6 years. All patients were classified into two groups according to nutritional status, which was assessed by the ratio of total delivered calories to total required calories (D/R); group A (54 cases, 24.5%, D/R≥0.7) versus group B (166 cases, 75.5%, D/R<0.7). In multivariate analysis, incision in the lower abdomen (Odds Ratio 2.277, P=0.078), absence of NST consultation (Odds Ratio 2.728, P=0.011), and not receive minimal invasive surgery (Odds Ratio 3.518, P=0.001) were independent risk factors associated with poor nutritional status.
Conclusion:
Clinicians should pay more attention to patients who had an incision in the lower abdomen or did not receive minimal invasive surgery or NST consultation, which would be predisposing factors for nutritional insufficiency resulting in postoperative morbidities.
-
Citations
Citations to this article as recorded by- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 66. CrossRef
- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
- 869 View
- 0 Download
- 1 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


