Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
- Postoperative gut dysbiosis and its clinical implications, with an emphasis on probiotic strategies in gastric cancer patients undergoing gastrectomy: a narrative review
- Cheong Ah Oh
- Ann Clin Nutr Metab 2025;17(2):114-124. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0023
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review explores alterations in gut microbiota following gastrointestinal surgery, with a focus on gastrectomy for gastric cancer, and evaluates the therapeutic potential of probiotics in restoring microbial balance and reducing postoperative complications, including infections, inflammation, immune dysfunction, and cancer recurrence.
Current concept
Gastrointestinal surgery disrupts gut microbial homeostasis via surgical stress, oxygen exposure, altered bile flow, and perioperative antibiotic use. Gastrectomy, in particular, induces marked changes in the microbiota, including increased oral-origin and aerotolerant bacteria, decreased short-chain fatty acid–producing species, and elevated bile acid-transforming organisms. These alterations contribute to complications such as small intestinal bacterial overgrowth, surgical site infections, postoperative ileus, nutrient malabsorption, and potentially a higher risk of colorectal cancer. Probiotics—especially strains of Lactobacillus, Bifidobacterium, and Clostridium—have demonstrated beneficial effects by modulating the gut ecosystem, enhancing epithelial barrier integrity, and regulating immune and metabolic pathways. Randomized clinical trials support using probiotics in improving gastrointestinal recovery, reducing systemic inflammation, restoring microbial diversity, and shortening hospital stays after gastrectomy. Multi-strain probiotic formulations, particularly when administered perioperatively, show the greatest promise. However, safety concerns remain, especially for immunocompromised or critically ill patients, underscoring the need for rigorous clinical oversight and adherence to regulatory standards such as the European Food Safety Authority’s Qualified Presumption of Safety guidelines.
Conclusion
Postoperative dysbiosis is a modifiable factor in adverse surgical outcomes. Probiotic supplementation offers promising therapeutic potential in patients undergoing gastrectomy, though optimal strains, dosing, and timing remain to be determined. Tailored, evidence-based strategies may ultimately enhance both recovery and long-term outcomes after gastric cancer surgery.
- 8,542 View
- 55 Download

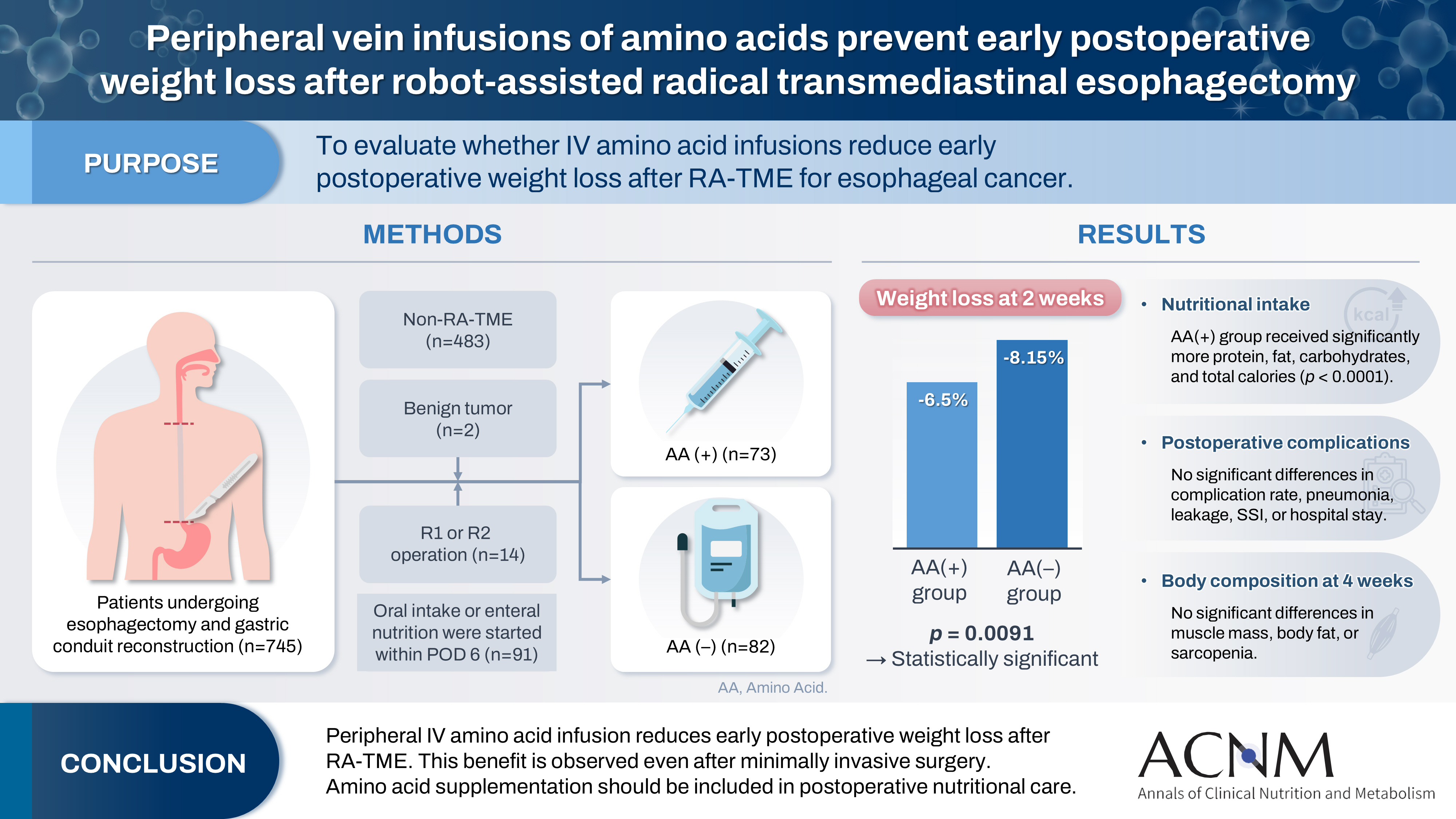
- Peripheral vein infusions of amino acids prevent early postoperative weight loss after robot-assisted radical transmediastinal esophagectomy: a retrospective study in Japan
- Tomonori Narita, Kazuhiko Fukatsu, Satoshi Murakoshi, Reo Inoue, Kenichi Kono, Midori Noguchi, Nana Matsumoto, Shoh Yajima, Koichi Yagi, Yoshifumi Baba
- Ann Clin Nutr Metab 2025;17(2):149-155. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0012
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 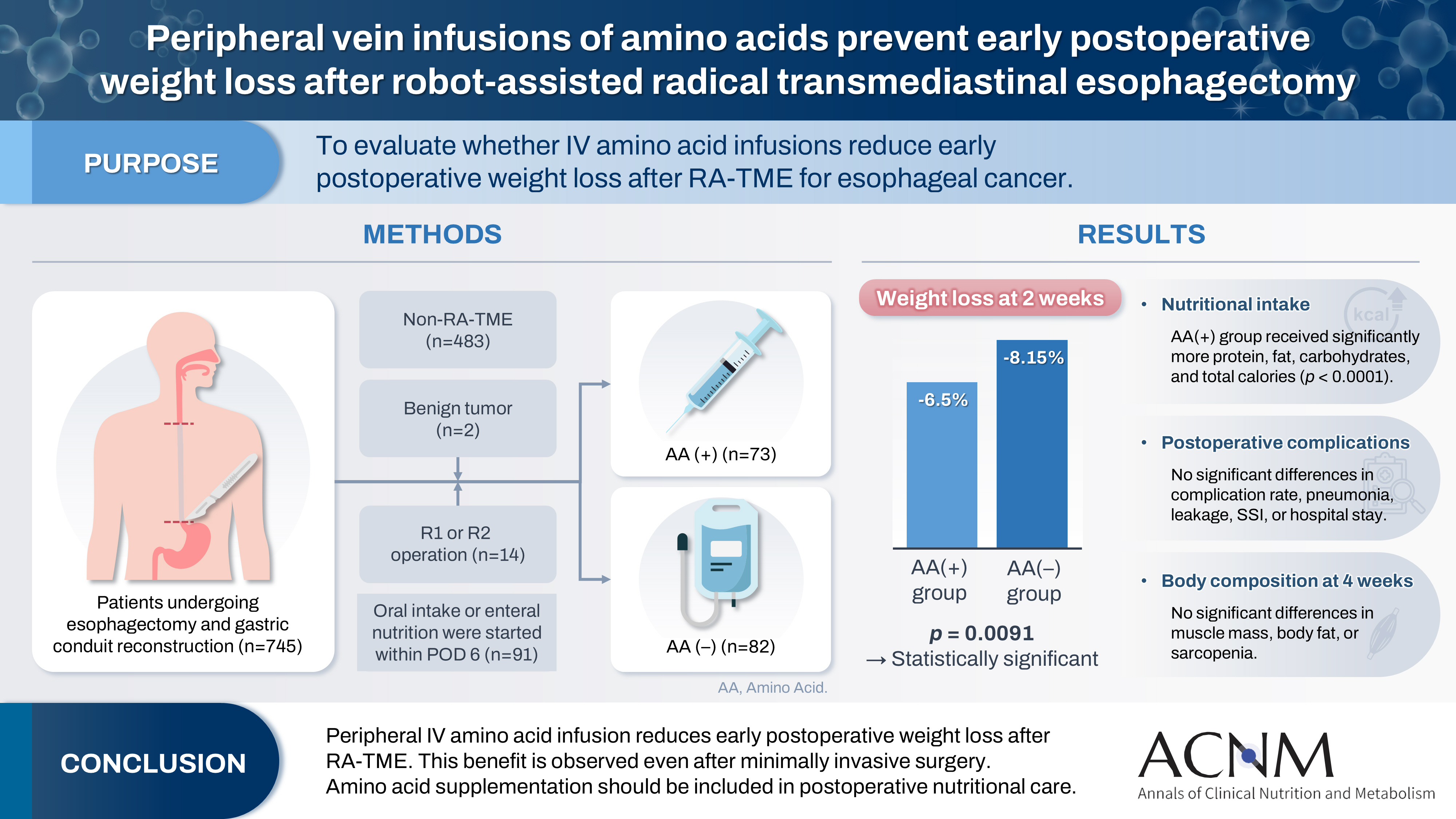
- Purpose
Postoperative body weight loss (PBWL) is linked to poor long-term outcomes following esophagectomy for esophageal cancer, making perioperative nutrition critically important. Although minimally invasive procedures such as robot-assisted radical transmediastinal esophagectomy (RA-TME) have become more prevalent, less attention has been paid to perioperative nutritional management. This study evaluates the impact of intravenous (IV) amino acid infusions on PBWL in patients undergoing RA-TME.
Methods
We retrospectively analyzed 155 patients who underwent RA-TME for esophageal or esophagogastric junction cancer at our hospital between 2011 and 2022. Patients were divided into two groups: AA(+) (n=73, received IV amino acids between postoperative days 1–6) and AA(–) (n=82, did not receive IV amino acids). Oral or enteral nutrition was withheld until postoperative day 6. We compared nutrient intake, postoperative outcomes, and nutritional status between groups.
Results
Patient backgrounds, surgical outcomes, and complication rates were similar in both groups. However, the AA(+) group received significantly greater energy and nutrient intake. PBWL at 2 weeks post-surgery was significantly lower in the AA(+) group than in the AA(–) group (6.50% vs. 8.15%, P=0.0091).
Conclusion
IV amino acid infusion may help mitigate early PBWL after RA-TME.
- 1,184 View
- 17 Download

- Pathogenesis, risk factors, and management of postoperative delayed gastric emptying after distal gastrectomy: a narrative review
- Cheong Ah Oh
- Ann Clin Nutr Metab 2025;17(1):9-17. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0007
-
 Abstract
Abstract
 PDF
PDF - Purpose
This narrative review elucidates the complex pathogenesis, key risk factors, and effective management strategies for postoperative delayed gastric emptying (DGE) following distal gastrectomy with D2 lymphadenectomy, a definitive procedure for middle and lower gastric cancer. It also explores opportunities for improved prevention and innovative treatment options.
Current concept
DGE significantly disrupts gastric motility and presents with symptoms such as early satiety, postprandial fullness, nausea, vomiting, and gastric atony. Although rarely fatal, DGE hampers oral intake, prolongs hospital stays, and diminishes quality of life. Current evidence indicates that DGE is a multifactorial disorder resulting from an interplay of vagal nerve disruption, damage to smooth muscle and interstitial cells of Cajal, imbalances in gastrointestinal hormones, and postoperative gut microbiome dysbiosis. Patient-specific factors, including advanced age, poor nutritional status, diabetes, and preoperative pyloric obstruction, along with surgical factors (most notably Billroth II reconstruction), further increase the risk of DGE. Management involves dietary modifications, prokinetic agents (such as metoclopramide and selective 5-HT4 agonists like prucalopride), and gastric decompression.
Conclusion
DGE is a challenging complication following gastrectomy that demands a deeper understanding of its underlying mechanisms to improve patient outcomes. Emerging therapies, including microbiota modulation and advanced pharmacological agents, offer promising new treatment avenues.
- 10,053 View
- 112 Download

- Association between decreased dietary intake during hospitalization and long-term weight loss in postoperative gastric cancer patients over 75 years of age: a retrospective cohort study
- Daiki Tabe, Isao Miyajima, Akira Tsukada
- Ann Clin Nutr Metab 2025;17(1):75-84. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0004
-
 Abstract
Abstract
 PDF
PDF - Purpose
Weight loss following gastrectomy is a significant concern, and maintaining adequate nutrition is necessary, especially given the growing number of older adult patients. This study examined the relationship between postoperative food intake and long-term weight loss in postgastrectomy patients aged ≥75 years.
Methods
Out of 88 patients who underwent gastrectomy for gastric cancer at our institute, 46 were aged ≥75 years. These patients were divided into two groups: one with an average energy intake exceeding 50% of the basal metabolic rate and one with an intake below 50% of the basal metabolic rate. The percentage change in body weight up to 6 months post-surgery was compared between the groups.
Results
In the group with higher dietary intake, the rate of weight change at 3 and 6 months postoperatively was lower, and fewer patients received postoperative adjuvant chemotherapy.
Conclusion
Poor postoperative food intake may serve as a predictor of weight loss up to 3 months following surgery in postgastrectomy patients aged ≥75 years. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,075 View
- 26 Download
- 1 Crossref

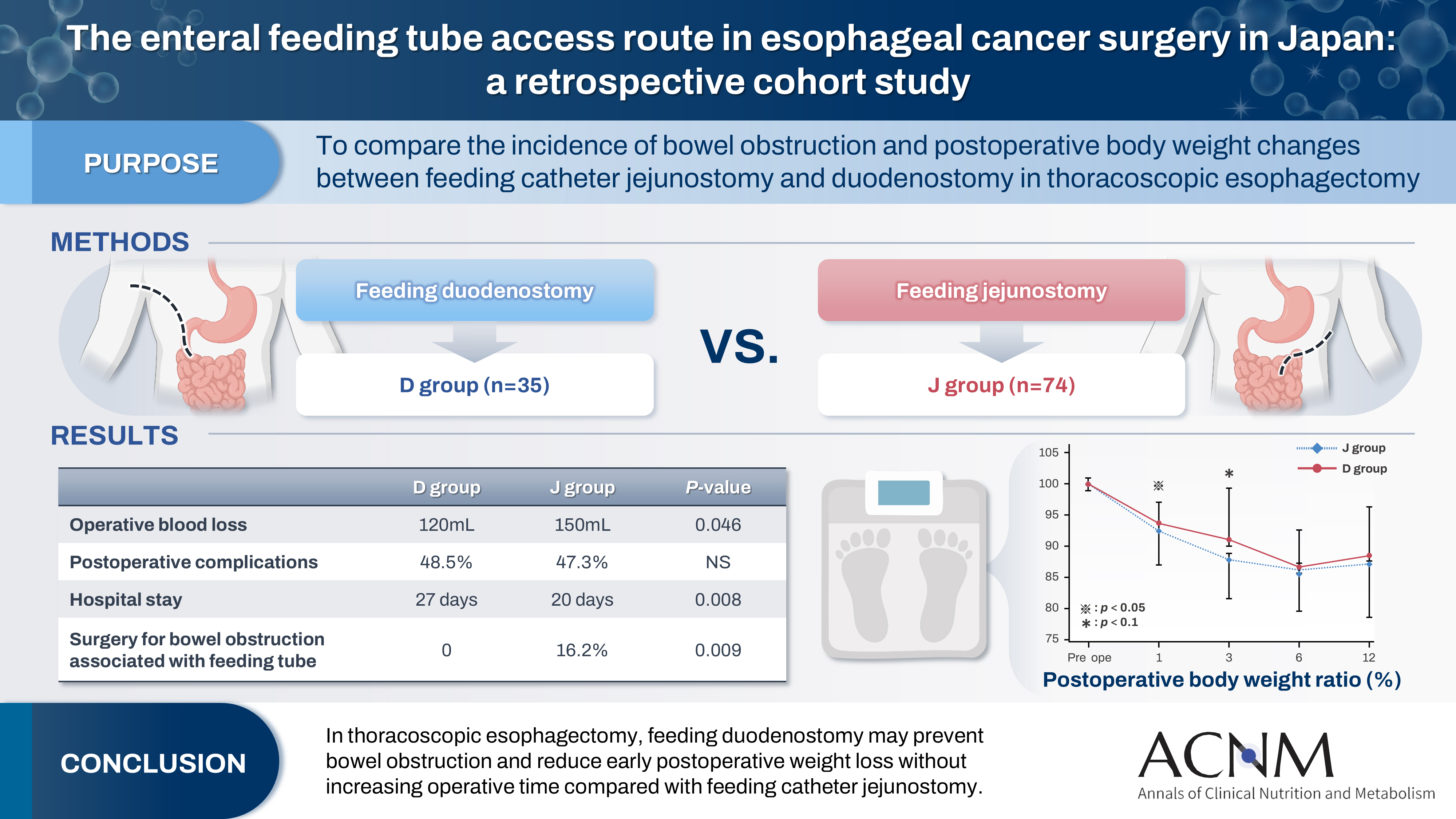
- The enteral feeding tube access route in esophageal cancer surgery in Japan: a retrospective cohort study
- Hiroyuki Kitagawa, Keiichiro Yokota, Tsutomu Namikawa, Kazuhiro Hanazaki
- Ann Clin Nutr Metab 2025;17(1):58-65. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0003
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 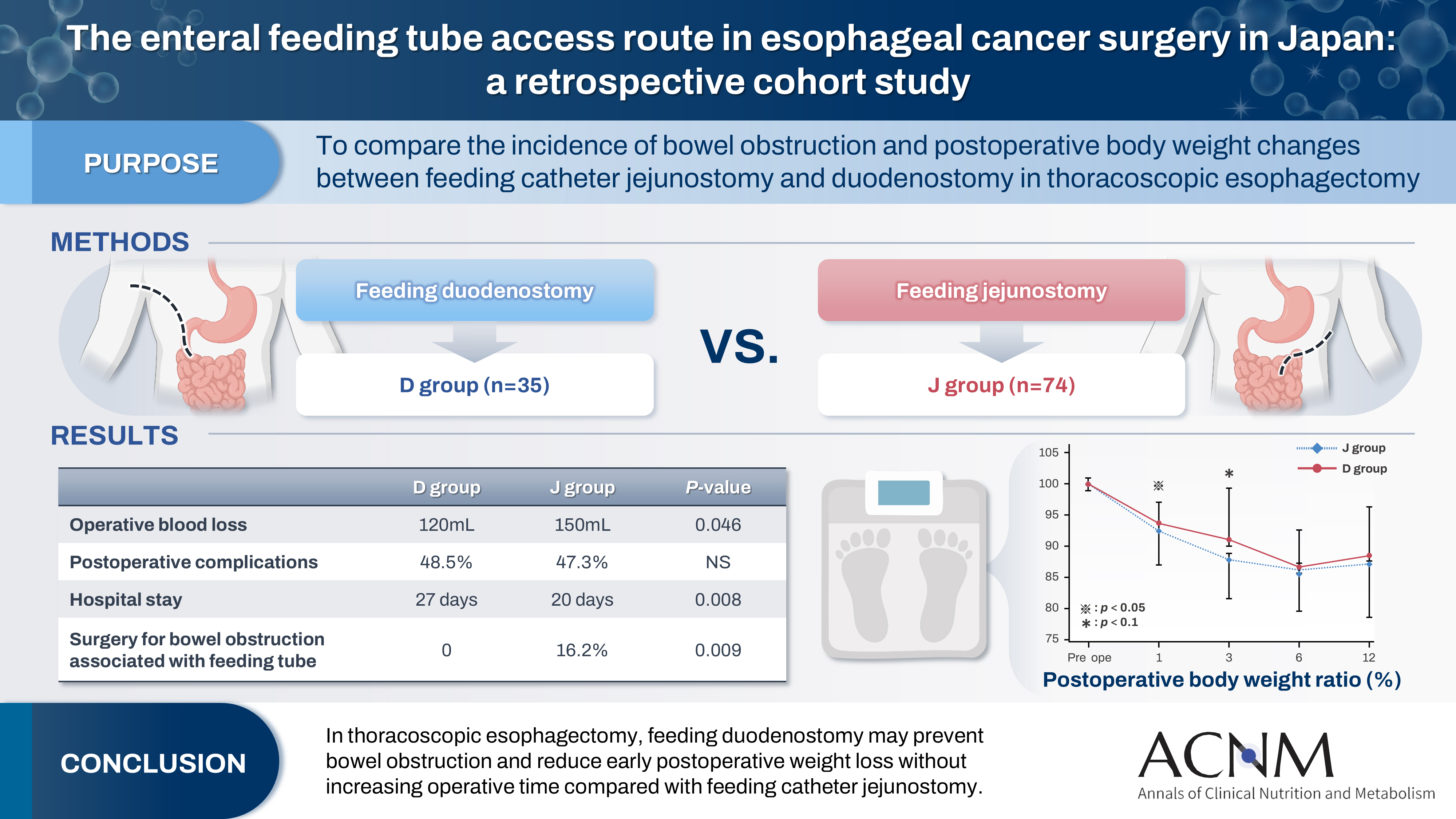
- Purpose
Feeding catheter jejunostomy is a useful access route for early enteral nutrition during esophageal cancer surgery. However, it may lead to postoperative bowel obstruction associated with feeding jejunostomy (BOFJ). To prevent BOFJ, we introduced feeding catheter duodenostomy via the round ligament in 2018. This study aimed to compare the incidence of BOFJ and postoperative body weight changes between feeding catheter jejunostomy and duodenostomy.
Methods
A total of 109 patients who underwent thoracoscopic esophagectomy and gastric tube reconstruction for esophageal cancer at Kochi Medical School Hospital between March 2013 and November 2020 were included. Preoperative patient characteristics (age, sex, preoperative weight, body mass index, cancer stage, and preoperative treatment), surgical outcomes (operative time, blood loss, and postoperative complications [wound infection, pneumonia, anastomotic leakage, BOFJ]), and body weight changes at 1, 3, 6, and 12 months post-surgery were compared between the jejunostomy (J) and duodenostomy (D) groups.
Results
The D group consisted of 35 patients. No significant differences were observed between the groups regarding age, sex, weight, body mass index, cancer stage, operative time, postoperative complications, or duration of tube placement. However, the D group had a significantly lower rate of preoperative chemotherapy (45.7% vs. 78.4%, P=0.001) and lower operative blood loss (120 mL vs. 150 mL, P=0.046) than the J group. All 12 cases of BOFJ occurred in the J group. Furthermore, the D group experienced a significantly lower weight loss ratio at 1 month postoperatively (93.9% vs. 91.8%, P=0.039).
Conclusion
In thoracoscopic esophagectomy, feeding duodenostomy may prevent bowel obstruction and reduce early postoperative weight loss without increasing operative time compared with feeding catheter jejunostomy. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 2,484 View
- 30 Download
- 1 Crossref

- Development of a pre- and re-habilitation protocol for gastrointestinal cancer surgery
- Eun Young Kim, Jung Hoon Bae, Jiseon Kim, Eun Joo Yang, Sang-Jae Park, In Kyu Lee, on behalf of the Task Force Team for Development and Trial Application of Pre/Rehabilitation Protocol in GI Cancer Surgery
- Ann Clin Nutr Metab 2025;17(1):25-40. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0001
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
Surgical resection is the primary curative treatment for gastrointestinal (GI) cancer; however, it is associated with high postoperative complication rates and impaired recovery. Frailty, malnutrition, and sarcopenia increase morbidity and mortality, underscoring the need for perioperative rehabilitation programs. Standardized rehabilitation protocols during the perioperative period are currently lacking in Korea. We aimed to develop an evidence-based rehabilitation protocol for GI cancer patients to enhance postoperative outcomes and facilitate clinical implementation.
Methods
A multidisciplinary task force team comprising experts in surgery, clinical nutrition, and rehabilitation medicine conducted a systematic literature search and comprehensive review from 2012 to 2022 to develop a standardized pre- and re-habilitation protocol for GI cancer surgery. The protocol underwent external validation and subsequent refinements before being finalized through expert consensus.
Results
The protocol development process was organized into four consecutive phases: keyword selection, literature review and case report form development, initial protocol drafting, and external validation leading to the final version of the protocol. The final version of the rehabilitation protocol is presented in the main text and included as Supplements.
Conclusion
This protocol provides a standardized clinical guideline based on the latest evidence-based pre- and re-habilitation strategies and is designed for seamless integration into routine clinical practice. By facilitating proactive rehabilitation interventions, it aims to improve outcomes in GI cancer patients who are at high risk of postoperative complications, functional decline, and malnutrition.
- 3,225 View
- 100 Download

- The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
- Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(2):22-42. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.22
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition was established to develop ERAS guidelines tailored to the Korean context. This guideline focuses on creating the most current evidence-based practice guidelines for ERAS based on systematic reviews. All key questions targeted randomized controlled trials (RCTs) exclusively. If fewer than two RCTs were available, studies using propensity score matching were also included. Recommendations for each key question were marked with strength of recommendation and level of evidence following internal and external review processes by the committee.
-
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Optimizing postoperative pain management in minimally invasive colorectal surgery
Soo Young Lee
Annals of Coloproctology.2024; 40(6): 525. CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 9,467 View
- 124 Download
- 2 Crossref

- Perioperative nutritional practices and attitudes among gastrointestinal oncologic surgeons in Korea: a nation-wide survey study
- Dae Hoon Kim, Jeong-Meen Seo, Min-Gew Choi
- Ann Clin Nutr Metab 2023;15(3):81-87. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.81
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: This study aimed to investigate the current perioperative nutritional practices and attitudes among gastrointestinal (GI) oncologic surgeons in Korea. Evidence-based perioperative nutritional practices are not well-established in this field.
Methods: A nationwide survey was conducted with 24 items, targeting GI oncologic surgical faculty members from March 2022 to April 2022 through social networking service messaging and email. Whole target number was 3,421.
Results: Out of responding 161 GI surgeons, 83.9% were male and 16.1% were female, and about 49.7% were in their 40s. When asked about their hospital policies, 67.1% reported the existence of formal nutritional screening programs. However, the execution and analysis of these programs varied considerably. Most surgeons conducted preoperative nutritional screening, with albumin testing the most frequently performed. In addition, nutritional supplementation—primarily protein drinks—was given before surgery. The duration for which these supplements were used varied from ≤3 days to 4–7 days. Most respondents recognized the importance of addressing nutritional deficiencies in patients with GI tumors; however, when asked about immunonutrition, 89.4% of surgeons admitted having limited knowledge.
Conclusion: Although there is recognition of the importance of evidence-based nutrition practices in GI and oncologic surgery programs, this study reveals limited implementation of such practices. This study highlights a considerable opportunity to leverage existing positive surgeon beliefs and published data on the benefits of perioperative nutrition to enhance surgical nutrition practices and to improve patient outcomes in Korea.
- 1,421 View
- 10 Download

- Role of preoperative immunonutrition in patients with colorectal cancer: a narrative review
- Soo Young Lee, Hyeung-min Park, Chang Hyun Kim, Hyeong Rok Kim
- Ann Clin Nutr Metab 2023;15(2):46-50. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: Colorectal cancer surgery presents challenges due to surgical stress and immunosuppression, leading to postoperative complications. Nutrition is crucial for colorectal cancer patients who are prone to malnutrition. This study aims to provide a comprehensive review of the role of preoperative immunonutrition in colorectal cancer surgery.
Current concept: Preoperative immunonutrition, consisting of immunonutrients such as arginine, ω-3 fatty acids, and nucleotides, has emerged as a potential strategy to enhance surgical outcomes by modulating immune responses and reducing complications. Current guidelines recommend preoperative oral nutritional supplements for major abdominal surgery and immunonutrition for nutritionally high-risk patients. Meta-analysis have demonstrated significant decreases in infectious complications and hospital stay durations with preoperative immunonutrition. However, limitations such as publication bias and heterogeneity in the previous studies should be considered. Further research should focus on the optimal timing, duration, and amount of immunonutrition; the patient populations that would benefit most; and the integration of immunonutrition into enhanced recovery after surgery protocols.
Conclusion: While preoperative immunonutrition shows promise, additional research is crucial to refine protocols and establish optimal clinical practice utilization. -
Citations
Citations to this article as recorded by- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Coloproctology.2025; 41(1): 3. CrossRef - Efficacy of preoperative immunonutrition in malnourished patients undergoing colorectal cancer surgery: a study protocol for a multicenter randomized clinical trial
Soo Young Lee, Chang Hyun Kim, Gi Won Ha, Soo Yeun Park, In Jun Yang, Jin Soo Kim, Gyung Mo Son, Sung Il Kang, Sung Uk Bae
Trials.2025;[Epub] CrossRef - The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Clinical Nutrition and Metabolism.2024; 16(2): 22. CrossRef
- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
- 14,962 View
- 89 Download
- 3 Crossref

- Refeeding Syndrome after Gastrectomy in a Patient with Hypophosphatemia: A Case Report
- Cheong Ah Oh
- Ann Clin Nutr Metab 2022;14(2):88-92. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.88
-
 Abstract
Abstract
 PDF
PDF - This study describes an 81-year-old male who was highly suspicious for refeeding syndrome (RFS) after a retrospective review of his postoperative clinical progression. This highlights the importance of clinicians’ awareness of the possibility of RFS development in surgical patients with any RFS risk factors.
- 2,428 View
- 21 Download

- Body Compositions of Elderly and Non-Elderly Patients Following Gastrectomy for Gastric Cancer
- Ji Hoon Kang, Mi Ran Jung, Sung Eun Kim, Oh Jeong
- Ann Clin Nutr Metab 2022;14(2):81-87. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.81
-
 Abstract
Abstract
 PDF
PDF - Purpose: Radical gastric resection is the mainstay of treatment in gastric cancer. However, patients can suffer from eating restrictions, weight loss, and malnutrition after gastrectomy, to which elderly patients are more vulnerable. We compared body composition changes in elderly patients and non-elderly patients after gastrectomy.
Materials and Methods: This prospective study enrolled patients who underwent gastrectomy for gastric carcinoma between 2019 and 2021. Body composition was measured using bioelectrical impedance analysis (InBody S10) before surgery and up to 12 months after surgery. Patients were divided into an elderly group (>70 years) and a non-elderly group (≤70 years), and body composition changes were compared between the two groups using the linear mixed model.
Results: There were 69 patients in the elderly group and 164 patients in the non-elderly group. The groups showed no significant differences in gastric resection or pathologic stage. Overall, body composition, including total body water, body weight, lean body mass, skeletal muscle mass, and fat mass, decreased immediately after surgery and gradually improved until postoperative 12 months. A linear mixed model showed no significant time×group interactions for any body composition factors between groups.
Conclusion: Body composition changes did not significantly differ between elderly patients and non-elderly patients after gastrectomy.
- 1,409 View
- 4 Download

- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
- Ji-Hyeon Park, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Jong Won Kim, Ki Bum Park, In Cho, Sun-Hwi Hwang, Dong-Wook Kim, Su Mi Kim, Seung-Wan Ryu, Seong Chan Gong, Pil Young Jung, Hoon Ryu, Sung Geun Kim, Chang In Choi, Dae-Hwan Kim, Sung-IL Choi, Ji-Ho Park, Dong Jin Park, Gyu-Yeol Kim, Yunhee Choi, Hyuk-Joon Lee
- Ann Clin Nutr Metab 2022;14(2):55-65. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.55
-
 Abstract
Abstract
 PDF
PDF - Purpose: To develop an individualized model for predicting the extent of unintentional weight loss following gastrectomy in patients with gastric cancer based on related risk factors and to externally validate this model using multicenter clinical data in Korea.
Materials and Methods: Among gastric cancer patients who underwent curative gastrectomy at 14 different gastric cancer centers, clinical data from patients with more than one weight measurement during the three-year follow-up period were retrospectively collected. Risk factors associated with weight loss in gastric cancer patients after gastrectomy were analyzed, and a predictive model was developed. Internal and external validation were performed.
Results: The data from 2,649 patients were divided into a derivation set (n=1,420 from Seoul National University Hospital) and validation set (n=1,229 from 13 different gastric cancers). Postoperative duration (six vs. 12, 24, or 36 months), sex (female vs. male), age, preoperative body mass index, type of surgery (pylorus-preserving vs. total, distal or proximal gastrectomy), and cancer stage (I vs. II or III) were included in the final prediction model. The model showed approximately 20% accuracy in predicting weight loss at each period: R2 at six, 12, 24 and 36 months after gastrectomy in internal validation=0.20, 0.21, 0.17, and 0.18, respectively, and in external validation=0.20, 0.22, 0.18, and 0.18, respectively. Calibration slopes of internal and external validation were 0.95 and 1.0, respectively.
Conclusion: Although predictive accuracy of the model did not reach an acceptable level, repeated external validation measurements showed high reliability. The model may serve as a basic reference in clinical practice. -
Citations
Citations to this article as recorded by- Development and Feasibility Assessment of Mobile Application-Based Digital Therapeutics for Postoperative Supportive Care in Gastric Cancer Patients Following Gastrectomy
Ji-Hyeon Park, Hyuk-Joon Lee, JeeSun Kim, Yo-Seok Cho, Sunjoo Lee, Seongmin Park, Hwinyeong Choe, Eunhwa Song, Youngran Kim, Seong-Ho Kong, Do Joong Park, Byung-Ho Nam, Han-Kwang Yang
Journal of Gastric Cancer.2024; 24(4): 420. CrossRef
- Development and Feasibility Assessment of Mobile Application-Based Digital Therapeutics for Postoperative Supportive Care in Gastric Cancer Patients Following Gastrectomy
- 2,365 View
- 21 Download
- 1 Crossref

- Long-Term Changes of Body Mass Index and Nutritional Biochemical Markers in the Obese Elderly with Gastric Cancer
- Eunjung Kim, Ji-Hyeon Park, Eun-Mi Seol, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Hyuk-Joon Lee
- Ann Clin Nutr Metab 2021;13(2):52-61. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.52
- 1,307 View
- 4 Download

- Longitudinal Change in Health-Related Quality of Life after Total Gastrectomy: Approach Based on the Minimally Important Difference
- Sang Chun Park, Oh Jeong, Ji Hoon Kang, Mi Ran Jung
- Ann Clin Nutr Metab 2021;13(2):43-51. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.43
-
 Abstract
Abstract
 PDF
PDF - Purpose: The post-operative quality of life (QoL) is a significant concern for patients undergoing gastrectomy. Unlike subtotal gastrectomy, the detailed aspects of QoL involving the ability to perform everyday activities that reflect physical, psychological, and social well-being; and satisfaction with levels of functioning and control of the disease after total gastrectomy remain poorly investigated.
Materials and Methods: We enrolled 170 patients who underwent total gastrectomy for gastric carcinoma and completed the European Organisation for Research and Treatment of Cancer (EORTC) Quality-of-Life questionnaires (QLQ) C30 and STO22 preoperatively and post-operatively at 1, 6, and 12 months. We investigated the QoL change in terms of the minimally important difference (MID), which refers to a score change patients would perceive as clinically important (effect size >0.5).
Results: At 1-month post-surgery, MID in global health, physical, social, role, emotional, and cognitive functions was observed at 44.0%, 68.0%, 42.7%, 38.7%, 32.0%, and 16.0% respectively. Of QLQ-C30 symptoms, MID was frequently observed in appetite (52.9%). Of the QLQ-STO22 symptoms, MID was frequently observed in eating restrictions (74.1%), dysphagia (63.5%), pain (51.8%), and anxiety (50.6%). At 12 months post-surgery, MID in global health, physical, role, cognitive, social, and emotional functions was 32.9%, 58.8%, 42.4%, 40.0%, 36.5%, and 17.6%, respectively. Of QLQ-C30 symptoms, MID was frequently observed in diarrhea (52.9%). Of the QLQ-STO22 symptoms, MID was frequently observed in eating restrictions (63.5%), dysphagia (52.9%), body image (55.3%), pain (55.3%), and anxiety (51.8%). Male sex, comorbidity, D2 lymphadenectomy, and post-operative morbidity were associated with MID in global health at 12 months post-surgery.
Conclusion: This study provides information about the detailed aspects of impairment in various functions and symptoms of QoL after total gastrectomy. This information can be used to develop a tailor-made management plan for QoL. -
Citations
Citations to this article as recorded by- Experiences After Endoscopic Resection in Patients With Early Gastric Cancer in Korea: A Qualitative Study
Yoon Kyung Kim, Chun-Ja Kim, Eunyoung Park, Ji Yea Lee, Kee-Myung Lee, Elizabeth A. Schlenk
Journal of Transcultural Nursing.2025; 36(5): 593. CrossRef - Proximal gastrectomy with tubular stomach reconstruction vs total gastrectomy for proximal gastric cancer following neoadjuvant chemotherapy: A multicenter retrospective study
Yi-Ming Lu, Peng Jin, Hai-Kuo Wang, Xin-Xin Shao, Hai-Tao Hu, Yu-Juan Jiang, Wang-Yao Li, Yan-Tao Tian
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Experiences After Endoscopic Resection in Patients With Early Gastric Cancer in Korea: A Qualitative Study
- 2,982 View
- 9 Download
- 2 Crossref

- Comparison of Post-Operative Nutritional Status according to the Extent of Gastrectomy and the Reconstruction Method in Patients with Gastric Cancer
- Kyung Hwan Kim, Jong Hyuk Yoon, Geum Jong Song, Myoung Won Son, Sung Yong Kim, Moo Jun Baek, Moon Soo Lee
- Ann Clin Nutr Metab 2021;13(2):34-42. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.34
-
 Abstract
Abstract
 PDF
PDF - Purpose: Malnutrition is the main complication after gastrectomy and the degree may vary depending on the extent of resection. This study sought to help determine an appropriate type of resection and provide methods for addressing malnutrition after gastrectomy.
Materials and Methods: We retrospectively reviewed medical records of patients with gastric cancer who underwent radical resection at the Soonchunhyang University Cheonan Hospital between December 2012 and December 2013. A total of 100 patients were screened, and all patients were followed for 1 to 3 years. Among this group, 12 underwent total gastrectomy, 5 underwent proximal gastrectomy, 46 underwent distal gastrectomy with Billroth I anastomosis, and 37 with Billroth II anastomosis. The nutritional status assessment included body weight, body mass index, serum albumin, serum hemoglobin, vitamin B12, ferritin, and Nutritional Risk Index (NRI).
Results: Patients who underwent total gastrectomy had lower hemoglobin and vitamin B12 levels compared to patients who underwent distal gastrectomy. The NRI was statistically significantly lower in patients who underwent total gastrectomy than patients who underwent distal gastrectomy. Patients who underwent total gastrectomy had lower vitamin B12 than patients who underwent proximal gastrectomy till the second year after gastrectomy. Regarding postdistal gastrectomy reconstruction, there was no statistically significant difference between the Billroth I and Billroth II groups.
Conclusion: This study showed that patients who underwent total gastrectomy were more susceptible to malnutrition than those who underwent distal or proximal gastrectomy. Patients who undergo gastrectomy should be monitored carefully for nutritional status and given appropriate nutritional support in the post-operative period. -
Citations
Citations to this article as recorded by- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
Ji-Hyeon Park, Seong-Ho Kong, Do Joong Park, Han-Kwang Yang, Jong Won Kim, Ki Bum Park, In Cho, Sun-Hwi Hwang, Dong-Wook Kim, Su Mi Kim, Seung-Wan Ryu, Seong Chan Gong, Pil Young Jung, Hoon Ryu, Sung Geun Kim, Chang In Choi, Dae-Hwan Kim, Sung-IL Choi, Ji
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 55. CrossRef
- Development and Internal/External Validation of a Prediction Model for Weight Loss Following Gastric Cancer Surgery: A Multicenter Retrospective Study
- 3,162 View
- 11 Download
- 1 Crossref

- Preoperative Neutrophil to Lymphocyte Ratio and Albumin Level as Predictors for Postoperative Complication in Patients with Colorectal Cancer
- Kyung Pil Kang, Young Hun Kim, Kyung Jong Kim PhD.
- Surg Metab Nutr 2020;11(2):66-72. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.66
-
 Abstract
Abstract
 PDF
PDF - Purpose: Systematic inflammatory response biomarkers are recognized as potential prognostic factors for colorectal cancer (CRC). Recently, the neutrophil-to-lymphocyte ratio (NLR) has emerged as a possible marker for predicting the outcomes of patients with CRC. The purpose of the current study was to determine if NLR could function as a predictive marker of postoperative complications in patients with colorectal cancer who were treated surgically.
Materials and Methods: One hundred and seven patients who underwent radical surgery for colorectal cancer were enrolled in the study. The NLR values were determined from the complete blood counts within one month before surgery. Values of less than or greater than 3 were defined as low (NLR-low) or high (NLR-high), respectively. Statistical comparisons were made between the NLR and the clinical-pathological variables.
Results: Sixty-eight patients met the criteria of NLR-low, and 39 patients were categorized as NLR-high. The NLR status was significantly correlated with T-stage, perineural invasion, and an increased likelihood of complications. Univariate analysis indicated that both low albumin and meeting the criteria for the NLR-high group correlated with an increased occurrence of complications (P=0.004, P=0.004, respectively). Multivariate analysis identified NLR-high and low albumin levels as independent predictors for complications (P=0.007, odd ratio=6.405, P=0.016, odd ratio=9.641, respectively)
Conclusion: The current results suggest that the preoperative NLR levels could be useful tools for predicting the occurrence of postoperative complications.
- 1,353 View
- 3 Download

- Pharmacologic Therapy for Cancer Anorexia-Cachexia Syndrome
- Seonkyeong Yoon, Hyunah Kim
- J Clin Nutr 2015;7(2):36-41. Published online August 31, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.2.36
-
 Abstract
Abstract
 PDF
PDF Cancer-related anorexia-cachexia syndrome (CACS) is a hypercatabolic state, characterized by reduced appetite and weight loss due to ongoing loss of skeletal muscle mass and adipose tissue. CACS occurs mainly in patients with advanced cancer; thus, weight loss in CACS is often associated with poor prognosis and decreased survival. A large number of studies have been conducted on various pharmacologic agents for palliation of cancer-related anorexia. The purpose of this article is to review the pre-existing pharmacologic agents used for CACS and to evaluate the evidence from current studies on each pharmacologic agent. First, appetite stimulants such as corticosteroids, progestins, cyproheptadine, and cannabinoid have been shown to be beneficial by improving appetite and helping with weight changes even if they had no effect on survival rate. Several other agents with anti-inflammatory effects (
e.g. , eicosapentaenoic acid, thalidomide, and melatonin), prokinetic agents (e.g. , metoclopramide), anabolic agents (e.g. , androgens and growth hormone), antipsychotics (e.g. , mirtazapine and olanzapine), and antiemetics have also been studied in patients in CACS; however further investigations would be required to confirm the beneficial effects.-
Citations
Citations to this article as recorded by- Bojungikgi-tang for Anorexia in Lung Cancer Patients with Treated with Chemotherapy: A Single-arm, Open-label, Single-center Trial
Im-Hak Cho, Seong-Hoon Yoon, So-Yeon Kim, Byoung-Kab Kang, Chang-Seob Seo, Young-Eun Choi, Hyeun Kyoo Shin, Jun-Yong Choi
Journal of Korean Medicine.2023; 44(4): 26. CrossRef
- Bojungikgi-tang for Anorexia in Lung Cancer Patients with Treated with Chemotherapy: A Single-arm, Open-label, Single-center Trial
- 2,575 View
- 1 Download
- 1 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


