Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 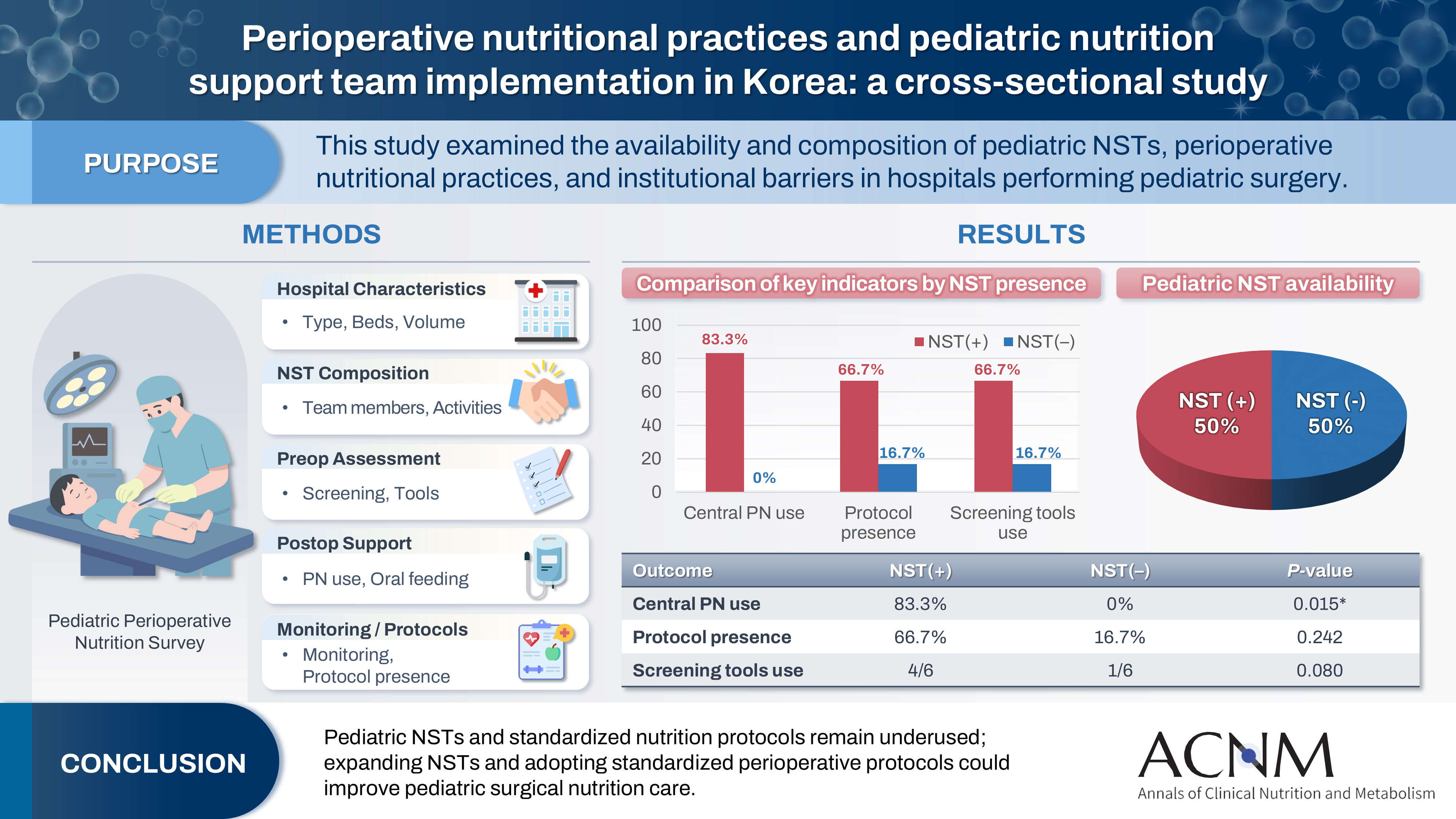
- Purpose
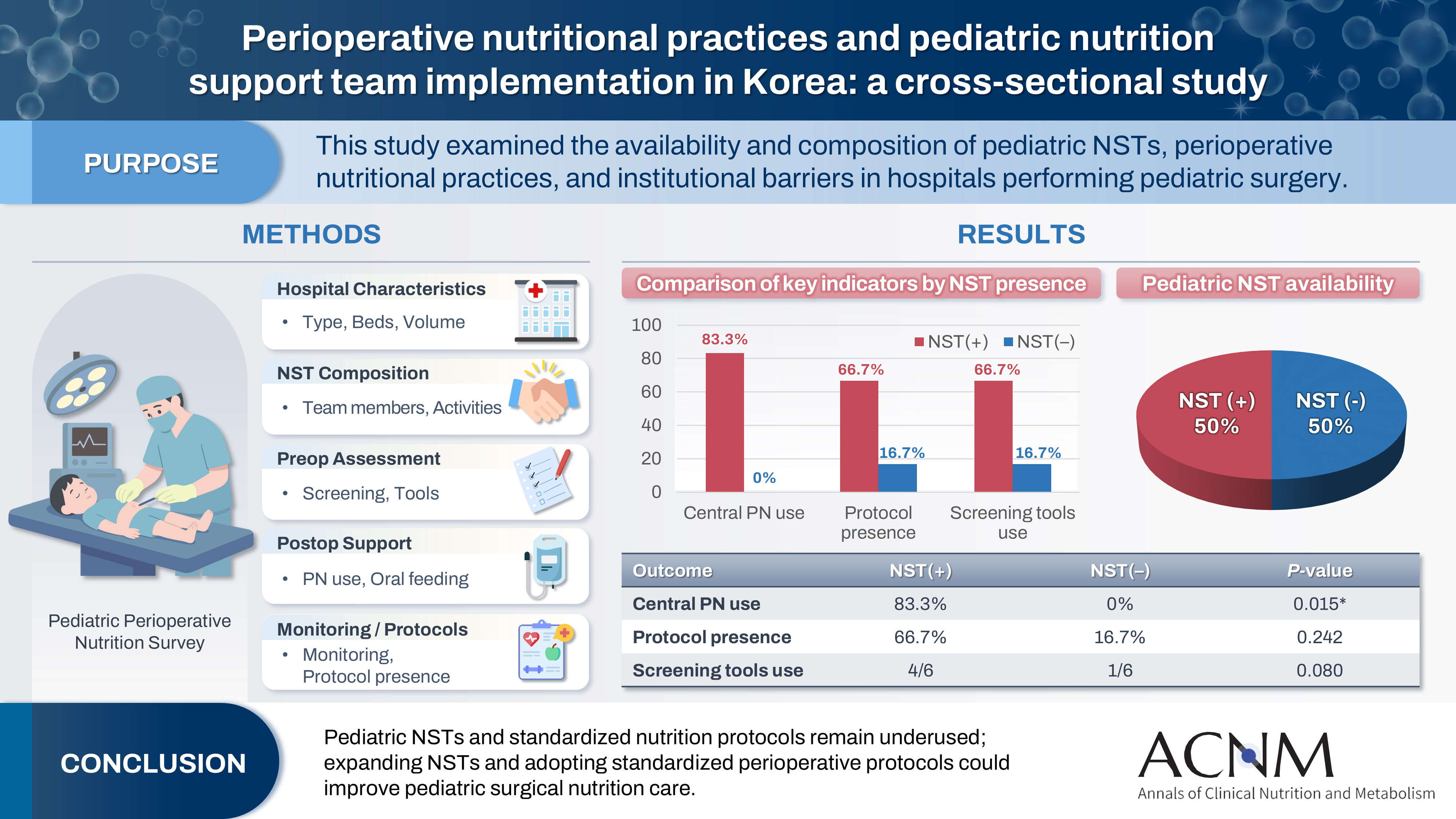
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 687 View
- 11 Download

- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
- So Hyun Nam
- Ann Clin Nutr Metab 2025;17(2):97-103. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0026
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
This study aimed to evaluate the current practices, activities, and challenges of nutrition support teams (NSTs) in Korea. The assessment was conducted as part of the 4th NST Leadership Program of the Korean Society of Surgical Metabolism and Nutrition held in 2025, which seeks to foster leadership and enhance team functionality.
Methods
A nationwide survey was conducted in February 2025 among 54 NST members from 44 institutions. The survey explored team composition, consultation volume, educational programs, barriers to implementation, institutional support, and reimbursement challenges.
Results
Of the 44 participating hospitals, most (86.4%) operated a single NST, with multidisciplinary physician involvement from over three specialties in 77.2% of cases. Inpatient referrals to NSTs were generally low, with less than 10% at 63% of institutions. Only 40.9% had an individual office, and formal incentive systems were reported in 18.1% of hospitals. Educational programs for in-hospital staff were limited (29.5%), and less than half conducted regular academic meetings. Rates of adoption of NST recommendations varied widely, with barriers including a lack of engagement from attending physicians, failure to review the recommendations, and department-specific clinical policies. Efforts to promote NST activation included computerized prescription systems, automated referral workflows, staff education, and quality improvement initiatives. Participants focused on sharing effective NST cases, building incentives, exchanging clinical insights, clarifying team roles and leadership, and developing unified practice guidelines.
Conclusion
NSTs in Korea are well established but face ongoing challenges in collaboration and sustainability. Continued leadership and policy support are crucial for enhancing team performance and improving patient outcomes. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 5,100 View
- 75 Download
- 1 Crossref

- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
- Seung Hwan Lee, Jae Gil Lee, Min Kwan Kwon, Jiyeon Kim, Mina Kim, Jeongyun Park, Jee Young Lee, Ye Won Sung, Bomi Kim, Seong Eun Kim, Ji Yoon Cho, A Young Lim, In Gyu Kwon, Miyoung Choi, KSPEN Guideline Committee
- Ann Clin Nutr Metab 2024;16(3):89-111. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.89
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Nutritional support for adult critically ill patients is essential due to the high risk of malnutrition, which can lead to severe complications. This paper aims to develop evidence-based guidelines to optimize nutritional support in intensive care units (ICUs).
Methods: The Grading Recommendations, Assessment, Development and Evaluation process was used to develop and summarize the evidence on which the recommendations were based. Clinical outcomes were assessed for seven key questions.
Results: We recommend the following: (1) initiate enteral nutrition (EN) within 48 hours after treatment as it is associated with improved outcomes, including reduced infection rates and shorter ICU stays; (2) early EN is preferred over early parenteral nutrition due to better clinical outcomes; (3) the use of supplementary parenteral nutrition to meet energy targets during the first week of ICU admission in patients receiving early EN is conditionally recommended based on patient-specific needs; (4) limited caloric support should be supplied to prevent overfeeding and related complications, particularly in the early phase of critical illness; (5) higher protein intake is suggested to improve clinical outcomes, such as muscle preservation and overall recovery; (6) additional enteral or parenteral glutamine is conditionally recommended against due to the lack of significant benefit and potential harm; and (7) fish oil-containing lipid emulsions is conditionally recommended due to their potential to enhance clinical outcomes, including reduced infection rates and shorter ICU stays.
Conclusion: These evidence-based recommendations can improve clinical outcomes and support healthcare providers in making informed decisions about nutritional interventions in the ICU. -
Citations
Citations to this article as recorded by- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
Paraskevi Papanikolaou, Xenophon Theodoridis, Androniki Papaemmanouil, Niki N. Papageorgiou, Alexandra Tsankof, Anna-Bettina Haidich, Christos Savopoulos, Konstantinos Tziomalos
Journal of Clinical Medicine.2025; 14(3): 991. CrossRef
- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
- 23,351 View
- 537 Download
- 1 Crossref

- Early nutritional support for inpatients reduces admission rates to intensive care units in Korea: a single-center case-control study
- Hyun Suk Kim, Jae Do Yang, Se Wung Han, Mi Rin Lee, Da-Sol Kim, Sejin Lee, Seon-Hyeong Kim, Chan-Young Kim
- Ann Clin Nutr Metab 2024;16(2):57-65. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.57
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Early nutritional support (ENS) for critically ill patients is promoted by many studies. However, there is a lack of data evaluating its necessity in general wards. This study aims to determine the impact of ENS on patients in general wards.
Methods: Patients aged 18 and above, admitted to the Jeonbuk National University Hospital in Jeonju from January 2020 to December 2020, who were eligible for nutritional support and hospitalized for at least 7 days were included in the study. We divided the patients into two groups: the ENS group, who received nutritional support within 48 hours of admission, and the control group, who received it after 48 hours.
Results: Among 1,077 patients, 146 met the inclusion criteria. The ENS group (n=38) and the control group (n=108) were compared retrospectively. There was a significant age difference between the two groups (P=0.028). The admission ratio to the intensive care unit (ICU) in the ENS group was significantly lower than that in the control group (10.2% vs. 26.3%, P=0.019). The calorie support rate (%) and protein support rate (%) in the ENS group were significantly higher than in the control group (50.12%±23.30% vs. 38.56%±18.02%, P=0.006; 44.61%±25.07% vs. 32.07%±22.76%, P=0.002, respectively). After propensity score matching, the ENS was significantly associated with ICU low admissions (odds ratio 0.08, 95% confidence interval 0.01–0.69, P=0.022).
Conclusion: A future multi-center study considering underlying diseases is needed to provide additional scientific evidence to support the effects of ENS.
- 2,245 View
- 24 Download

- Consultation pattern changes of parenteral nutrition with a multidisciplinary nutrition support team in a recently opened hospital in Korea: a retrospective cohort study
- Kyoung Won Yoon, Hyo Jin Kim, Yujeong Im, Seul Gi Nam, Joo Yeon Lee, Hyo Gee Lee, Joong-Min Park
- Ann Clin Nutr Metab 2023;15(2):57-63. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose: Parenteral nutrition (PN) is essential for the treatment of patients with malnutrition. The provision of central PN should be recommended by a nutrition support team (NST) made up of a team of experts, even in a newly established hospital. This study sought to evaluate the effectiveness of PN delivered by a multidisciplinary NST in a recently opened hospital.
Methods: This was a retrospective study of the effectiveness of a central PN recommendation pop-up message by the electronic medical record (EMR) software to prompt physicians to either calculate the required calorie and protein intake or consult with the NST. The study period was divided into pre-NST and post-NST based on the time of recruitment of NST-dedicated personnel.
Results: Patients in the 12-week pre-NST period (n=50) and 12-week post-NST period (n=74) were compared retrospectively. Baseline characteristics were not significantly different between the two groups, except for the median Acute Physiology and Chronic Health Evaluation II score (pre-NST group, 8 [interquartile range, IQR 5–15.5] vs. post-NST group, 15 [IQR 9–24], P=0.012) of the 45 patients total admitted to the intensive care unit. The percentage of patients for whom physicians requested a consultation with the NST for central PN was significantly higher in the post-NST group (52.0% vs. 75.7%, P=0.011). There was no significant difference in achievement of nutrition targets or mortality.
Conclusion: Building a multidisciplinary NST may increase awareness of nutritional status and affect the behavior of physicians in recently-opened hospitals.
- 1,777 View
- 10 Download

- Effects of nutritional status and support on the survival of COVID-19 patients in a single tertiary-center intensive care unit in Korea: a case-control study
- Na Gyeong Lee, Hye Jin Kim, Ji Gyeong Kang, Do Hyeon Jeon, Mi Seung Kwak, So Hyun Nam
- Ann Clin Nutr Metab 2023;15(1):30-37. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.30
-
 Abstract
Abstract
 PDF
PDF - Purpose: It is important to understand the nutritional status of critically ill COVID-19 patients and to provide adequate associated support. We attempted to determine how nutritional status and the amount of nutritional support provided to critically ill patients affect their survival.
Methods: We retrospectively reviewed the medical records of patients admitted to the intensive care unit of Dong-A University Hospital between January and December 2021. We divided the patients into survivors and those who died during COVID-19 treatment and compared and analyzed their clinical parameters, nutrition-related indicators, nutritional status, and nutritional support.
Results: Of 70 patients reviewed, 57 survived. Mortality was higher in the older group (P=0.006). The patients who underwent ventilator, extracorporeal membrane oxygenation, or continuous renal replacement therapy showed higher mortality. Nutritional status at the time of admission and the nutritional requirements did not differ among patient groups. However, the actual amounts of calories (P<0.001) and protein (P=0.019) supplied were lower in the mortality group. Serum C-reactive protein level was higher (P=0.002) and serum albumin level was lower in those who did not survive (P<0.001) compared with surviving patients at discharge.
Conclusion: We did not determine whether the initial nutritional status of patients with COVID-19 affected their survival due to various factors associated with the severity of the disease. However, given the similarities between disease severity and nutritional status at the time of admission, our results indicate that adequate nutritional support can contribute to survival in critically ill COVID-19 patients with pneumonia. -
Citations
Citations to this article as recorded by- The association between enteral nutrition with survival of critical patients with COVID‐19
Maryam Gholamalizadeh, Zahra Salimi, Khadijeh Abbasi Mobarakeh, Zahra Mahmoudi, Shirin Tajadod, Mahdi Mousavi Mele, Farkhondeh Alami, Bojlul Bahar, Saeid Doaei, Sara Khoshdooz, Masoume Rahvar, Somayeh Gholami, Masoume Pourtaleb
Immunity, Inflammation and Disease.2024;[Epub] CrossRef
- The association between enteral nutrition with survival of critical patients with COVID‐19
- 2,485 View
- 6 Download
- 1 Crossref

- Perioperative Nutritional Support
- Seung Jong Oh
- J Clin Nutr 2021;13(1):7-11. Published online June 30, 2021
- DOI: https://doi.org/10.15747/jcn.2021.13.1.7
-
 Abstract
Abstract
 PDF
PDF - Malnutrition in surgical patients is a prevalent problem. As the geriatric population gradually increases, surgeons need to be more careful in preventing the risk of iatrogenic malnutrition. Delayed wound healing, exposure to infection, pressure sores, gastrointestinal bacterial overgrowth, and immunosuppression in malnourished patients can be prevented or diminished with active nutritional support. Preoperative nutritional assessment and support, as well as adequate postoperative nutrition, will improve surgical outcomes, which in turn will lead to fewer postoperative complications, shorter hospital stays, and lower medical costs. The success of surgery depends not only on technical surgical skills but also on metabolic interventions that take into account the patient’s ability to deliver the metabolic load and provide adequate nutritional support.
- 793 View
- 2 Download

- Effect of Nutritional Intervention by the Nutrition Support Team on Postnatal Growth in Preterm Infants
- So Jin Yoon, Joo Hee Lim, Soon Min Lee, Sun Jung Kim, Sun Kyung Lee, Soo Min Lee
- J Clin Nutr 2020;12(2):26-33. Published online December 31, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.2.26
-
 Abstract
Abstract
 PDF
PDF - Purpose: Nutritional intervention by an interdisciplinary nutrition support team (NST) can potentially improve postnatal growth outcomes in preterm infants. This study aimed to measure the growth impact of a nutritional intervention package performed by an NST in a quality improvement effort in a neonatal intensive care unit (NICU).
Methods: Fifty-two infants born below 2,000 g and admitted to NICU participated in the Quality Improvement (QI) program between March 2016 and February 2017. The nutritional intervention was applied according to newly established nutritional guidelines on parenteral and enteral nutrition, and an NST performed a weekly nutritional assessment. The Z-scores of weight, height, and head circumference were calculated according to the gestational age and sex. The clinical impact on postnatal growth was compared between the QI and pre-QI groups. The pre-QI group included 69 infants admitted in the same NICU between 2014 and 2015.
Results: The time to the initiation of enteral nutrition decreased significantly (P<0.001). Changes in weight (P=0.027), head circumference (P=0.003), Z-scores between birth, and 40 weeks postconceptional age (PCA) were significantly larger in the QI than the pre-QI group. The percentage of infants weighing below the 10th percentile at one month after birth and at 40 weeks PCA was higher in the pre-QI than the QI group.
Conclusion: The implementation of evidence-based best practices for preterm nutrition resulted in significant improvements in the growth outcomes in preterm infants. -
Citations
Citations to this article as recorded by- Nutrition Supply and Growth Post Nutrition Support Team Activity in Neonatal Intensive Care Unit
Hye Min Ha, Yu Jin Jung, Yoo Rha Hong, So Yoon Choi
Pediatric Gastroenterology, Hepatology & Nutrition.2024; 27(5): 313. CrossRef
- Nutrition Supply and Growth Post Nutrition Support Team Activity in Neonatal Intensive Care Unit
- 1,059 View
- 1 Download
- 1 Crossref

- Nutritional Support Team Approach Decreases the In-Hospital Mortality Rate after Deceased Donor Liver Transplantation
- Sang-Oh Yun, Jong Man Kim, Sangjin Kim, Jinsoo Rhu, Hyun Jung Kim, Soo Hyun Park, Hyo Jung Park, Eunmi Gil, Wonseok Kang, Gyu-Seong Choi, Won Hyuck Chang, Jeong-Meen Seo, Jae-Won Joh
- Surg Metab Nutr 2020;11(1):7-11. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.7
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study compared the mortality rates between a period of time without employing a nutritional support team (NST) and a period of time with an NST.
Materials and Methods: Forty-six patients underwent adult deceased donor liver transplantation (DDLT) in 2016, and their medical records were prospectively collected. All the donor recipients underwent routine enteral feeding after liver transplantation. An NST cared for twenty-one patients after September 2016. The NST consisted of transplant surgeons, hepatologists, a critical care team, a rehabilitation team, dietitians, pharmacists, and nurses. We defined the patients within the time period without an NST as the control group and those patients within the time period with an NST as the case group.
Results: There were no statistically significant differences in baseline or perioperative characteristics between the two groups. The median model for the end-stage liver disease (MELD) score was 36 (range: 21∼40) for the control group and 36 (range: 23∼40) for the case group (P=0.596). The 30-day mortality rate was 24.0% (6/25) for the control group, but it was 4.8% (1/20) for the case group. The patient survival rates at 1-year and 2-year were 68.0% and 64.0% in the control group and 85.7% and 81.0% in the case group, respectively. However, there were no statistically significant differences of the 30-day mortality rate and 1∼2 year patient survival rate between the two groups.
Conclusion: The present study suggests that an NST should be required to prevent 30-day mortality and increase patient survival of adult DDLT patients with a high MELD score.
- 830 View
- 0 Download

- The Influence of Pediatric Nutrition Support Team on Hospitalized Pediatric Patients Receiving Parenteral Nutrition
- Sijin Baek, Juhyun Rho, Hyung Wook Namgung, Eunsook Lee, Euni Lee, Hye Ran Yang
- J Clin Nutr 2020;12(1):7-13. Published online June 30, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.1.7
-
 Abstract
Abstract
 PDF
PDF - Purpose: Malnutrition is a common problem in hospitalized patients that can increase the risk of complications, including infections and length of hospitalization. Appropriate nutritional support is important, particularly in pediatric patients, because growth and development are closely related to the nutritional supply. This study examined the status of nutritional support for pediatric patients in general wards to determine if interventions of the pediatric nutrition support team (pNST) contribute to appropriate nutritional support and help improve their nutritional status.
Methods: Between July 2016 and June 2017, all pediatric inpatients who received parenteral nutrition support at the Seoul National University Bundang Hospital were recruited and divided into the NST group and non-NST group according to the activities of pNST. The nutritional status was assessed in all subjects, and the calories and proteins delivered through nutritional support in each group were calculated and then compared with the recommended requirements in pediatric patients.
Results: The number of patients recruited was 174: 100 (57.5%) in the NST group and 74 (42.5%) in the non-NST group. Significantly more calories and protein were supplied in the NST group than the non-NST group in hospitalized children aged between four and 17 years (P<0.05). In the non-NST group, the amounts of calories supplied were insufficient compared to the recommended requirements. The proportion of patients supplied with the appropriate number of calories was 60.0% in the NST group and 20.0% in the non-NST group (P<0.001), and the proportion of cases supplied with the appropriate amount of protein was 87.0% in the NST group and 62.2% in the non-NST group (P<0.001).
Conclusion: Interventions of the pediatric nutrition support team contributed to the sufficient supply of calories and protein and the improvement of clinical outcomes in hospitalized children on parenteral nutrition therapy. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 728 View
- 5 Download
- 1 Crossref

- Nutritional Support for Cancer Patients
- Yoontaek Lee
- Surg Metab Nutr 2019;10(2):27-31. Published online December 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.2.27
-
 Abstract
Abstract
 PDF
PDF Cancers are the leading cause of death worldwide, and various modalities of cancer treatment, such as surgery, radiation therapy, and pharmacological therapies, have been applied. Malnutrition and a loss of muscle mass are encountered frequently in cancer patients and adversely affect the clinical outcomes. Therefore, screening for, monitoring, and treating malnutrition are important procedures in treating cancer patients. This paper reviews the guidelines as well as comparative studies describing the nutritional support provided to cancer patients and describes the evidence-based guidelines and recommendation for each topic.
- 1,300 View
- 15 Download

- Parenteral Nutrition in Hospitalized Adult Patients in South Korea
- Miyoung Ock, Sera Lee, Hyunah Kim
- J Clin Nutr 2018;10(2):38-44. Published online December 31, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.2.38
-
 Abstract
Abstract
 PDF
PDF Purpose:
Parenteral nutrition (PN) is known to provide therapeutic beneficial improvements in malnourished patients for whom enteral nutrition is not feasible. The objective of this study was to investigate the current clinical characteristics and utilization of PN in Korea.
Methods:
We analyzed the Health Insurance Review Agency National Inpatients Sample database from 2014 to 2016, which included 13% of all hospitalized patients in Korea. Adult patients aged 20 years or older and receiving premixed multi-chamber bag containing PN were included for this study. Patient characteristics, admission type, primary diagnosis, and hospital demographics were evaluated. SAS version 9.4 was used for data analysis.
Results:
From 2014 to 2016, 149,504 patients received premixed PN, with 226,281 PN prescriptions being written. The mean patient age was 65.0 years, and 81,876 patients (54.8%) were male. Premixed 3-chamber bag and 2-chamber bag PN solutions were utilized in 131,808 (88.2%) and 32,033 (21.4%) patients, respectively. The number of patients hospitalized through the emergency department were 70,693 (47.3%), whereas 43,125 patients (28.8%) were administered PN in intensive care units. In the adult PN patients, the highest primary diagnosis was malignant neoplasm of the stomach (8,911, 6.0%), followed by organism unspecified pneumonia (7,008, 4.7%), and gastroenteritis and colitis of unspecified origin (6,381, 4.3%). Overall, 34% of adult PN patients were diagnosed with malignancies, the most common being neoplasm of the stomach (17.7%), neoplasm of bronchus/lung (11.2%), neoplasm of colon (11.1%), and neoplasm of liver/intrahepatic bile ducts (10.0%). PN solutions were most frequently administered in the metropolitan area (55.0%) and in hospitals with more than 1,000 beds (23.6%).
Conclusion:
PN was commonly administered in older patients, with primary diagnosis of malignancy in a significant number of cases. This study is the first large-scale description of PN-prescribing patterns in real-world clinical practice in South Korea.
- 876 View
- 8 Download

- Analysis of Current Status and Predisposing Factors for Nutritional Support of Patients in Surgical Intensive Care Unit
- Byung Chul Kim, In Kyu Lee, Eun Young Kim
- Surg Metab Nutr 2016;7(2):32-38. Published online December 30, 2016
- DOI: https://doi.org/10.18858/smn.2016.7.2.32
-
 Abstract
Abstract
 PDF
PDF Purpose:
Enteral feeding is strongly recommended for critically ill patients since it can enhance the immunologic function, which serves as a host defense mechanism against inflammation or metabolic response to stress. Herein, we investigated nutritional status and estimated the adequacy of the nutritional supply for acutely ill patients admitted to the surgical intensive care unit (SICU) after a major operation.
Materials and Methods:
From February to October 2016, patients admitted and stayed over 48 hours after major surgical procedures at SICU in Seoul St. Mary’s Hospital were reviewed. The nutritional parameters and surgical outcomes were compared according to the status of nutritional support.
Results:
A total of 220 patients composed of 130 males (59.1%) and 90 females (40.9%) were enrolled, and mean age was 61.4±13.6 years. All patients were classified into two groups according to nutritional status, which was assessed by the ratio of total delivered calories to total required calories (D/R); group A (54 cases, 24.5%, D/R≥0.7) versus group B (166 cases, 75.5%, D/R<0.7). In multivariate analysis, incision in the lower abdomen (Odds Ratio 2.277, P=0.078), absence of NST consultation (Odds Ratio 2.728, P=0.011), and not receive minimal invasive surgery (Odds Ratio 3.518, P=0.001) were independent risk factors associated with poor nutritional status.
Conclusion:
Clinicians should pay more attention to patients who had an incision in the lower abdomen or did not receive minimal invasive surgery or NST consultation, which would be predisposing factors for nutritional insufficiency resulting in postoperative morbidities.
-
Citations
Citations to this article as recorded by- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 66. CrossRef
- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
- 794 View
- 0 Download
- 1 Crossref

- The Effects of Early Enteral Nutrition in Patients: A Role of Nutrition Support Team
- Kye Wol Park, Hee Ryoung Son, Ji Hoon Kim, Myoung Hee Kim, Eun Jin Choi
- J Clin Nutr 2016;8(2):66-70. Published online August 31, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.2.66
-
 Abstract
Abstract
 PDF
PDF Purpose:
The study examined the effects of early enteral nutrition on the patients’ length of stay in an intensive care unit (ICU), length of stay and mortality rate.
Methods:
A retrospective design was employed with a total of 461 patients (mean age=69.9±15.6 years; 253 males; 208 females). They were divided into two groups according to when they received enteral feeding: an “early enteral nutrition” (EEN) group of 148 patients (32.1%) who received enteral feeding within 48 hours of their arrival at the hospital and a “delayed enteral nutrition” (DEN) group of 313 patients (67.9%) who received enteral feeding at some point after 48 hours of their arrival at the hospital. The EEN group and control group were similar in terms of age, sex, body mass index, and underlying diseases.
Results:
The EEN group’s total length of stay in hospital was shorter (23.29±27.19 days) than that of the control group (36.74±32.24 days); the difference was significant (P<0.001). The EEN group also showed a shorter length of stay in the ICU (13.67±22.77 days) than the DEN group (17.46±21.02 days) and a lower mortality rate (17.6%) than the control group (18.8%), but these differences were not significant.
Conclusion:
The study found that early enteral nutrition treatment reduced total length of stay in hospital significantly. The findings suggest that early enteral nutrition treatment plays an important role in the patients’ recovery and prognosis.
-
Citations
Citations to this article as recorded by- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
Seung Hwan Lee, Jae Gil Lee, Min Kwan Kwon, Jiyeon Kim, Mina Kim, Jeongyun Park, Jee Young Lee, Ye Won Sung, Bomi Kim, Seong Eun Kim, Ji Yoon Cho, A Young Lim, In Gyu Kwon, Miyoung Choi
Annals of Clinical Nutrition and Metabolism.2024; 16(3): 89. CrossRef - The Status of Enteral Nutrition Formula Use by Dietitians in Hospitals Within Busan and Gyeongnam Area
Haejin Kang, Minji Woo, Eunju Park, Yoo Kyoung Park
Clinical Nutrition Research.2022; 11(1): 9. CrossRef - Physician Compliance with Nutrition Support Team Recommendations: Effects on the Outcome of Treatment for Critically Ill Patients
Hyon-Ju Yon, Eun-Suk Oh, Ji Young Jang, Ji Yun Jang, Hongjin Shim
Journal of Acute Care Surgery.2022; 12(1): 1. CrossRef - Health and Nutrition Status of Elderly People with Multimorbidity: A Korea National Health and Nutrition Examination Survey (2013~2015)
Na-Gyeong Oh, Jung-Sook Seo
Korean Journal of Community Nutrition.2020; 25(6): 502. CrossRef
- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
- 910 View
- 8 Download
- 4 Crossref

- Nutritional Supports in Patients with Inflammatory Bowel Disease
- Bong-Hyeon Kye
- J Clin Nutr 2016;8(1):11-18. Published online April 30, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.1.11
-
 Abstract
Abstract
 PDF
PDF Underweight and specific nutrient deficiencies are frequent in adult patients with inflammatory bowel disease (IBD). In addition, a significant number of children with IBD, particularly Crohn’s disease (CD) have impaired linear growth. Nutritional support is important in patients with IBD and nutritional problems. Enteral nutrition (EN) can reduce CD activity and maintain remission in both adults and children. Given that the ultimate goal in the treatment of CD is mucosal healing, this advantage of EN over corticosteroid treatment is valuable in therapeutic decision-making. EN is indicated in active CD, in cases of steroid intolerance, in patient’s refusal of steroids, in combination with steroids in undernourished individuals, and in patients with inflammatory stenosis of the small intestine. EN should be the first choice compared to total parenteral nutrition. However, EN does not have a primary therapeutic role in ulcerative colitis. In conclusion, it appears that the role of nutrition as supportive care in patients with IBD should not be underestimated. The aim of this comprehensive review is to provide the reader with an update on the role of nutritional support in IBD patients.
-
Citations
Citations to this article as recorded by- Anti-inflammatory and apoptosis improving effects of sulfasalazine and Cinnamomi cortex and Bupleuri radix mixture in TNBS-induced colitis mouse model
Kyeong Jo Kim, Mi-Rae Shin, Soo Hyun Kim, Su Ji Kim, Ah Reum Lee, O Jun Kwon, Ki-Jung Kil, Seong-Soo Roh
Journal of Applied Biological Chemistry.2017; 60(3): 227. CrossRef
- Anti-inflammatory and apoptosis improving effects of sulfasalazine and Cinnamomi cortex and Bupleuri radix mixture in TNBS-induced colitis mouse model
- 1,289 View
- 13 Download
- 1 Crossref

- Use of Bioelectrical Impedance Analysis for Nutritional Treatment in Critically Ill Patients
- Yeon Hee Lee, Jae Myeong Lee
- J Clin Nutr 2015;7(1):9-14. Published online April 30, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.1.9
-
 Abstract
Abstract
 PDF
PDF Patients in the intensive care unit (ICU) easily have large amounts of extracellular fluids, such as edema or ascites, because of cardiovascular instability under septic conditions and also have high risk of malnutrition while staying in the ICU. Traditional nutritional assessment parameters like body mass index have a limitation in ICU patients due to muscle atrophy and decrease of lean body mass. Bioimpedence analyses (BIA) can be used to assess body composition and are useful in performance of nutritional assessments in ICU patients. BIA can simply and noninvasively estimate body composition (total body water, extracellular water, intracellular water, body cell mass, and free fat mass etc.) by sending a weak electric current through the body. In particular, phase angle (PhA, phase difference between the voltage applied to the impedance and the current driven through it), one of the parameters of BIA, is related to cell membrane integrity or cell size. Low PhA can possibly imply malnutrition and PhA has been reported as a useful indicator of clinical outcomes or prognosis of severe patients. Additional study with clinical application of BIA in ICU patients is needed in order to confirm the usefulness of BIA.
-
Citations
Citations to this article as recorded by- CORRELATION BETWEEN COVID-19 SYMPTOMS AND CERTAIN PHYSIOLOGICAL AND BODY COMPOSITION PARAMETERS RELATED TO OBESITY AND OVERWEIGHT
Attila Novák, Szabolcs Szalánczi, Beatrix Hornyák, Zsófia Rázsó, Andrea Sótér, Csaba Nyakas
Military Medical Science Letters.2024; 93(1): 112. CrossRef - Sequential Changes in Body Composition Using Bioelectrical Analysis during the Metabolic Response in Critically Ill Surgical Patients
Seok Rae Park, Seung Hwan Lee, Kyung Sik Kim, Hosun Lee, Tae Hwa Hong, Jae Gil Lee
Surgical Metabolism and Nutrition.2017; 8(1): 13. CrossRef
- CORRELATION BETWEEN COVID-19 SYMPTOMS AND CERTAIN PHYSIOLOGICAL AND BODY COMPOSITION PARAMETERS RELATED TO OBESITY AND OVERWEIGHT
- 899 View
- 4 Download
- 2 Crossref

- Effects of Nutrition Consultation on Nutritional Status in Critically Ill Surgical Patients
- Hee Sook Hwang, Seung Hwan Lee, Hosun Lee, Kyung Sik Kim, Seo Jin Chung, Jae Gil Lee
- J Clin Nutr 2015;7(1):28-34. Published online April 30, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.1.28
-
 Abstract
Abstract
 PDF
PDF Purpose:
The aim of this study was to investigate nutritional support status and effects of nutrition consultation in critically ill surgical patients.
Methods:
The medical records of 76 patients, admitted between June 1 and November 30, 2013, were reviewed retrospectively. Patients were divided into 2 groups: the nutrition consultation group (n=17) and the no consultation group (n=59). Patients were also divided into 3 groups: the enteral nutrition (EN) group (n=8), the parenteral nutrition (PN) group (n=25), and the enteral and parenteral mixed nutrition (ENPN) group. Total delivered/required caloric ratio and serum albumin, serum total protein, hemoglobin and other biochemical variables were compared in each group.
Results:
Mean daily required and delivered caloric/protein amount were EN group 60.0%, PN group 64.6%, and ENPN group 86.9%. ENPN group showed statistically significant difference when compared with EN group, PN group (P=0.005). When the proportion of patients who were fed more than 75% of the daily required calories was calculated, EN, PN, and ENPN showed 37.5%, 25.0% and 81.8%, respectively. ENPN group were significantly more supplied (P=0.007). Although neither the nutrition consultation group nor the non-consultation group received more than 80% of the daily required calories, the nutrition consultation group received 73% of the daily required calories whereas the no consultation group only received 46% (P=0.007). The total delivered/required protein ratio was approximately 69% of the nutrition consultation group and approximately 42% of the no consultation group (P=0.006).
Conclusion:
The results of providing nutritional consultation to intensive care unit patients showed an increase in the nutrition support. Nutrition education, continuous monitoring and management for nutritional support by systemic administration of a nutritional support team should be considered in order to achieve effective clinical outcomes in critically ill surgical patients.
-
Citations
Citations to this article as recorded by- Early nutritional support for inpatients reduces admission rates to intensive care units in Korea: a single-center case-control study
Hyun Suk Kim, Jae Do Yang, Se Wung Han, Mi Rin Lee, Da-Sol Kim, Sejin Lee, Seon-Hyeong Kim, Chan-Young Kim
Annals of Clinical Nutrition and Metabolism.2024; 16(2): 57. CrossRef - Clinical pharmacist interventions in nutrition-and drug-related problems in critically ill patients with renal dysfunction: a non-randomized controlled study
Betül Özgan, Yunus Emre Ayhan, Sule Apikoglu, Sait Karakurt
Frontiers in Medicine.2024;[Epub] CrossRef - Physician Compliance with Nutrition Support Team Recommendations: Effects on the Outcome of Treatment for Critically Ill Patients
Hyon-Ju Yon, Eun-Suk Oh, Ji Young Jang, Ji Yun Jang, Hongjin Shim
Journal of Acute Care Surgery.2022; 12(1): 1. CrossRef - Nutrition and Clinical Outcomes of Nutrition Support in Multidisciplinary Team for Critically Ill Patients
Jeong Shin Lee, Ji Eun Kang, So Hyun Park, Hye Kyung Jin, Soo Min Jang, Sun Ah Kim, Sandy Jeong Rhie
Nutrition in Clinical Practice.2018; 33(5): 633. CrossRef - The Comparison of Improvement Effect in Patient’s Nutrition State according to the Adaptation of Nutrition Support Team’s Consultation
권지은, 김순주, 나현오, 박애령
Journal of Korean Society of Health-System Pharmacists.2017; 34(2): 147. CrossRef
- Early nutritional support for inpatients reduces admission rates to intensive care units in Korea: a single-center case-control study
- 814 View
- 4 Download
- 5 Crossref

- Refeeding Syndrome
- Jeong Wook Kim
- J Clin Nutr 2015;7(1):15-22. Published online April 30, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.1.15
-
 Abstract
Abstract
 PDF
PDF Refeeding syndrome refers to a life-threatening shift of electrolytes and fluid with metabolic abnormalities in malnourished patients undergoing refeeding, whether orally, enterally, or parenterally. Clinical findings are fluid-balance abnormalities, abnormal glucose metabolism, hypophosphatemia, hypomagnesemia, hypokalemia and deficiencies of vitamin and trace element. Multiple organ systems including cardiac, respiratory, neurologic, renal, hematologic, and gastrointestinal can be affected. When recognized in a timely manner, these complications can be easily and successfully prevented and treated. Four factors appear fundamental: early identification of patients at risk, correction of abnormalities before refeeding, close monitoring during refeeding, and an appropriate feeding regimen.
-
Citations
Citations to this article as recorded by- Refeeding Syndrome after Gastrectomy in a Patient with Hypophosphatemia: A Case Report
Cheong Ah Oh
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 88. CrossRef - Effects of Early Phosphorus Intake on Respiratory Distress in Extremely Low-Birth-Weight Infants
Hye Jung Bae, Hyung Woo Yoon, Moon Jin Kim, Ae Hee Jung, Sun Hoi Jung, Hyeon Joo Hahn, Yun Hee Jo, Yoon Sook Cho, Ee-Kyung Kim, Seung Han Shin, In Gyu Song, Seung Hyun Shin
Neonatal Medicine.2019; 26(3): 155. CrossRef
- Refeeding Syndrome after Gastrectomy in a Patient with Hypophosphatemia: A Case Report
- 2,396 View
- 33 Download
- 2 Crossref


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


