Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
- The 2024 Korean Enhanced Recovery After Surgery guidelines for hepatobiliary and pancreatic surgery
- Kwangpyo Hong, Hongbeom Kim, Hyung Sun Kim, Hae Won Lee, Ho Joong Choi, YoungRok Choi, Jae Do Yang, Sung-Moon Jeong, Dae Wook Hwang, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2025;17(3):172-180. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0034
-
 Abstract
Abstract
 PDF
PDF - Purpose
The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition has developed comprehensive guidelines for hepatobiliary and pancreatic (HBP) surgery by adapting established international protocols. These guidelines provide evidence-based recommendations specifically tailored to the Korean healthcare system and address perioperative management for both pancreatoduodenectomy and hepatectomy.
Methods
The HBP subcommittee reviewed existing international ERAS guidelines and conducted an adaptation process. Key questions were identified based on national survey results from Korean HBP surgeons and were prioritized according to clinical relevance. The committee focused on elements supported by moderate- to high-quality evidence with strong recommendation grades. Literature searches were conducted through January 2025, and evidence quality was evaluated using GRADE methodology. Four key questions underwent formal assessment, and eight additional questions were adapted from international guidelines.
Results
Twelve key questions were selected and addressed, covering critical perioperative care domains: prehabilitation, preoperative nutritional assessment and support, anti-thrombotic prophylaxis, prophylactic abdominal drainage, preoperative biliary drainage, smoking and alcohol cessation, pre-anesthetic medication, minimally invasive surgical approaches, prophylactic nasogastric intubation, postoperative glycemic control, perianastomotic drainage management, and early mobilization protocols. Each recommendation was assigned specific evidence levels and graded for strength. High-quality evidence supported strong recommendations for the routine avoidance of prophylactic drainage in uncomplicated hepatectomy, early drain removal after pancreatoduodenectomy in low-risk patients, elimination of routine nasogastric decompression, and the implementation of early mobilization strategies.
Conclusion
These Korean-adapted ERAS guidelines for HBP surgery are expected to standardize perioperative care, reduce postoperative complications, shorten hospital stays, and enhance overall patient outcomes across Korean healthcare institutions.
- 1,627 View
- 39 Download

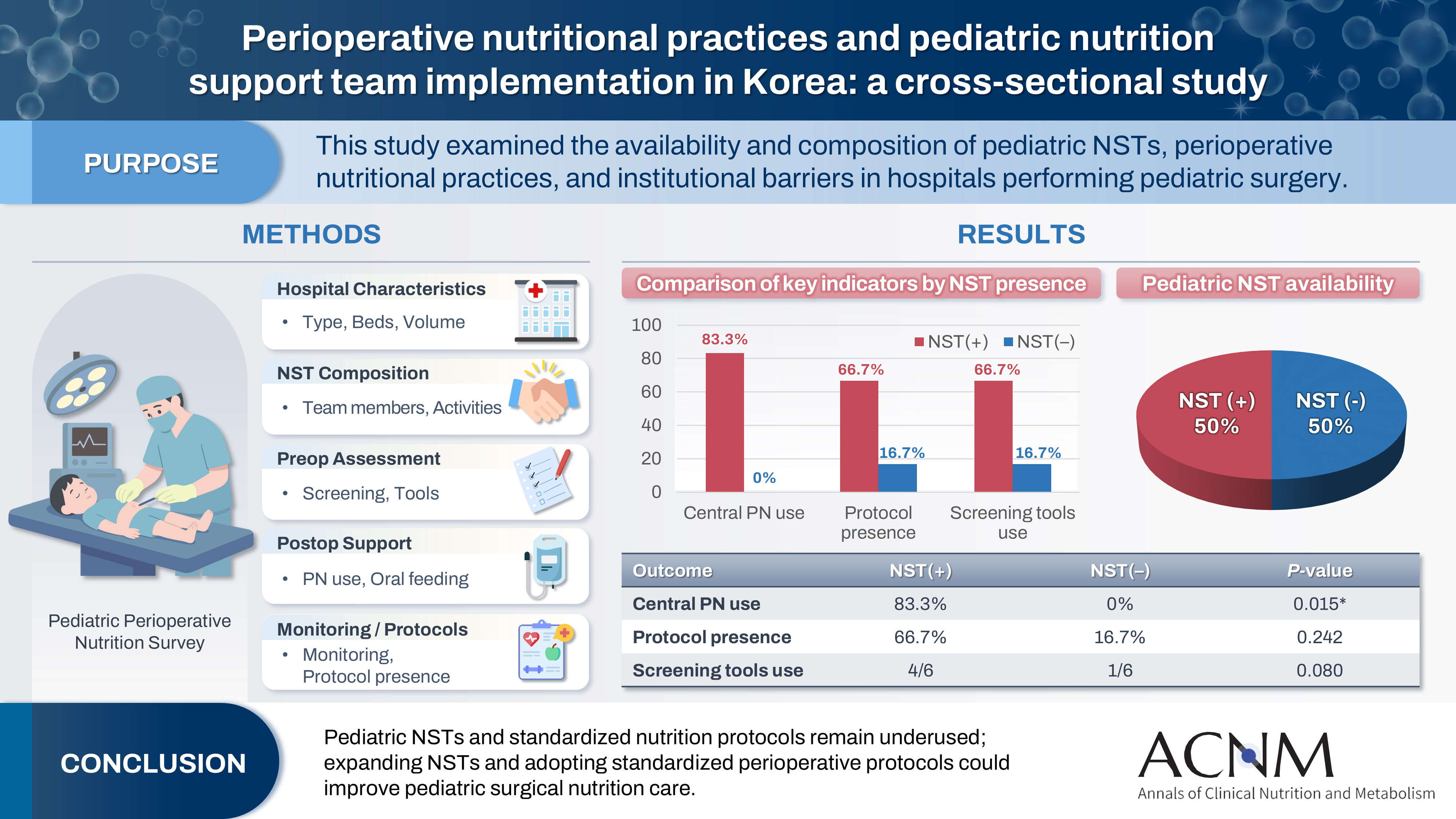
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 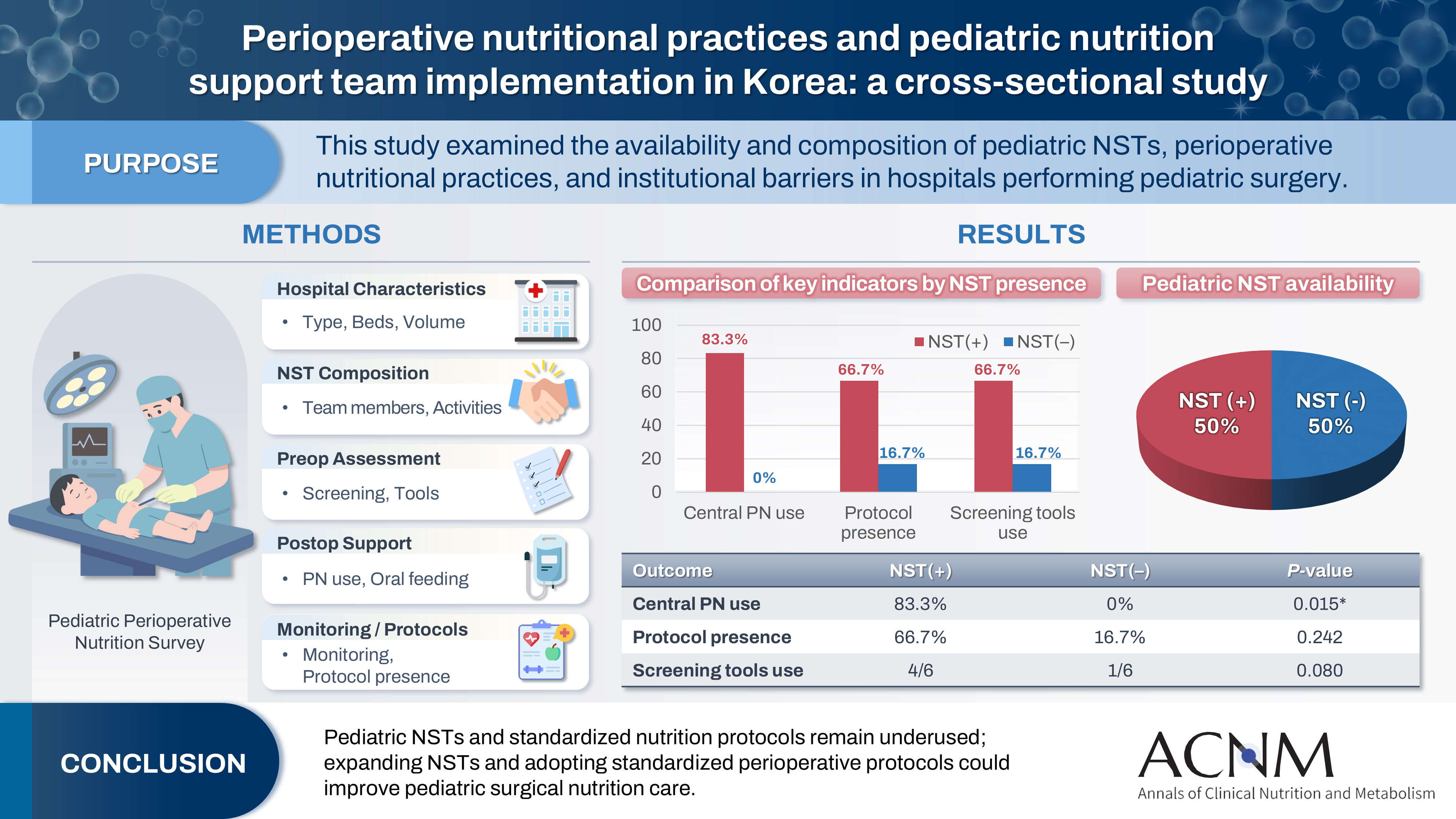
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 1,448 View
- 23 Download

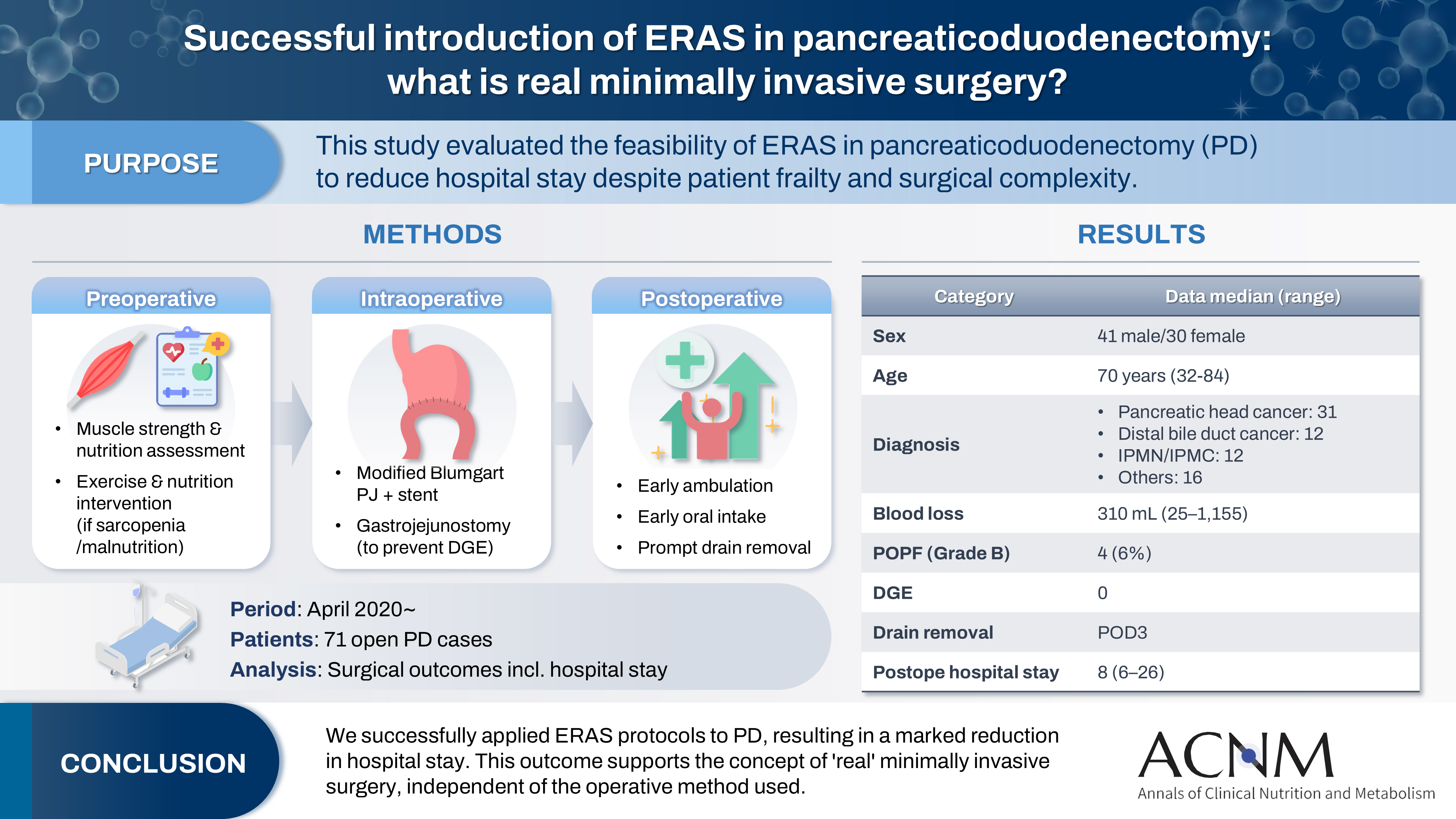
- Successful introduction of ERAS in pancreaticoduodenectomy: what is real minimally invasive surgery?
- Toshimi Kaido, Yosuke Miyachi, Koichiro Mitsuoka, Mariko Sambommatsu
- Ann Clin Nutr Metab 2025;17(2):156-161. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0014
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 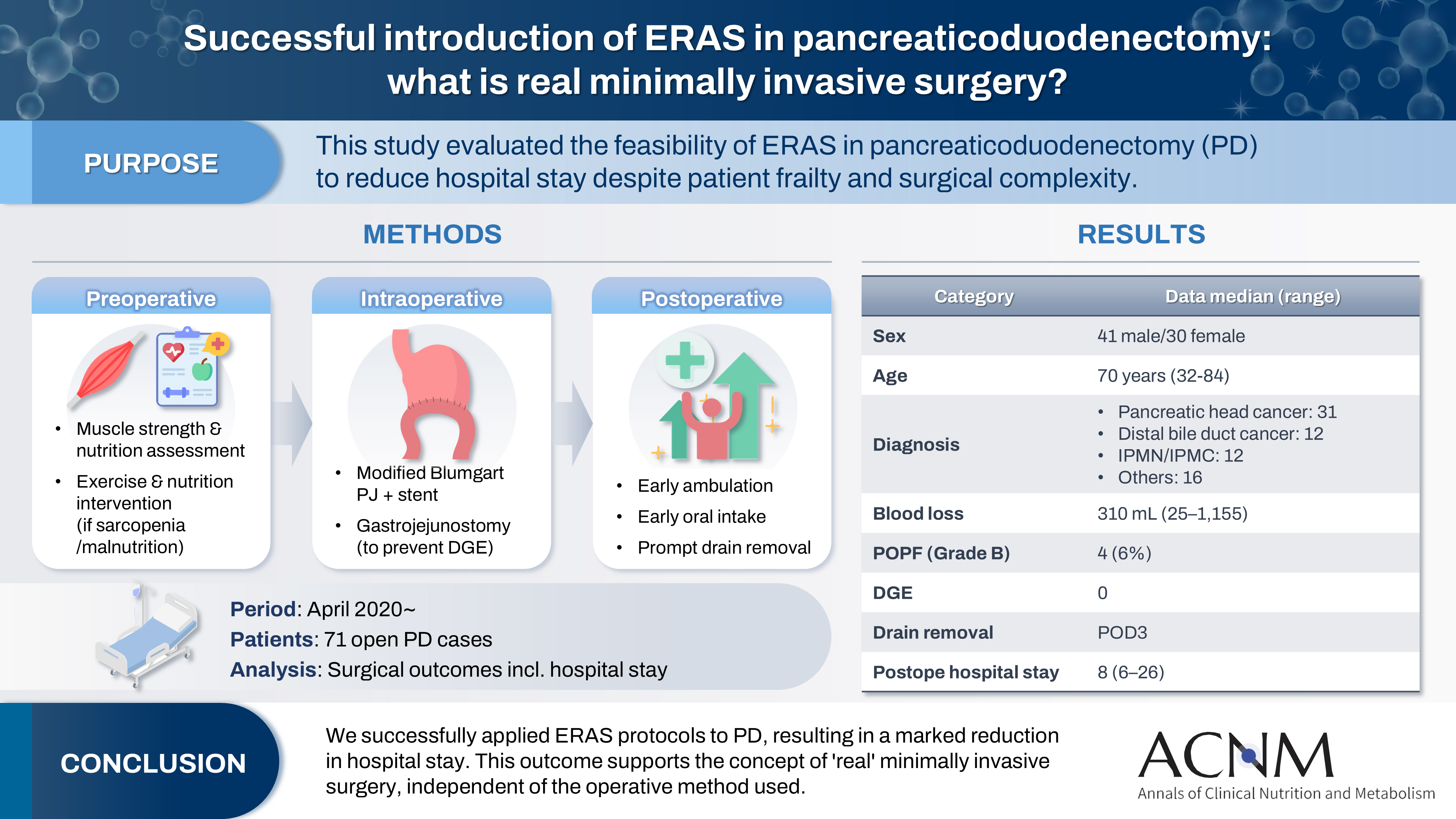
- Purpose
The introduction of Enhanced Recovery After Surgery (ERAS) protocols for pancreaticoduodenectomy (PD) has been considered challenging due to factors such as preexisting malnutrition, sarcopenia, the complexity of the surgery, and the high incidence of postoperative complications, including postoperative pancreatic fistula (POPF) and delayed gastric emptying (DGE). This study aimed to determine whether ERAS could be implemented in PD to achieve shorter postoperative hospital stays.
Methods
Our novel approach consists of three components. Preoperatively, we routinely assess patients' muscle strength and nutritional status and initiate exercise and nutritional interventions for those identified with sarcopenia or malnutrition. Intraoperatively, we perform pancreaticojejunostomy using a modified Blumgart’s technique with our stent placement policy and utilize new gastrojejunostomy methods to prevent DGE. Principles of postoperative management are early ambulation, early oral intake, and early drain removal. Since April 2020, we have employed this strategy and retrospectively evaluated its effectiveness. We enrolled 71 consecutive patients who underwent open PD with curative intent. Various surgical outcomes, including postoperative hospital stay, were analyzed.
Results
There were 41 men and 30 women, with a median age of 70 years. Preoperative diagnoses included pancreatic head cancer in 31, distal bile duct cancer in 12, and others. Median intraoperative blood loss was 310 mL. Grade B POPF occurred in four patients (6%). No cases of DGE were observed. The median postoperative hospital stay was 8 days (range, 6–26 days).
Conclusion
We successfully implemented ERAS protocols in PD and achieved a significantly reduced postoperative hospital stay. We propose that this approach is “real minimally invasive surgery," regardless of the surgical technique used.
- 3,966 View
- 19 Download

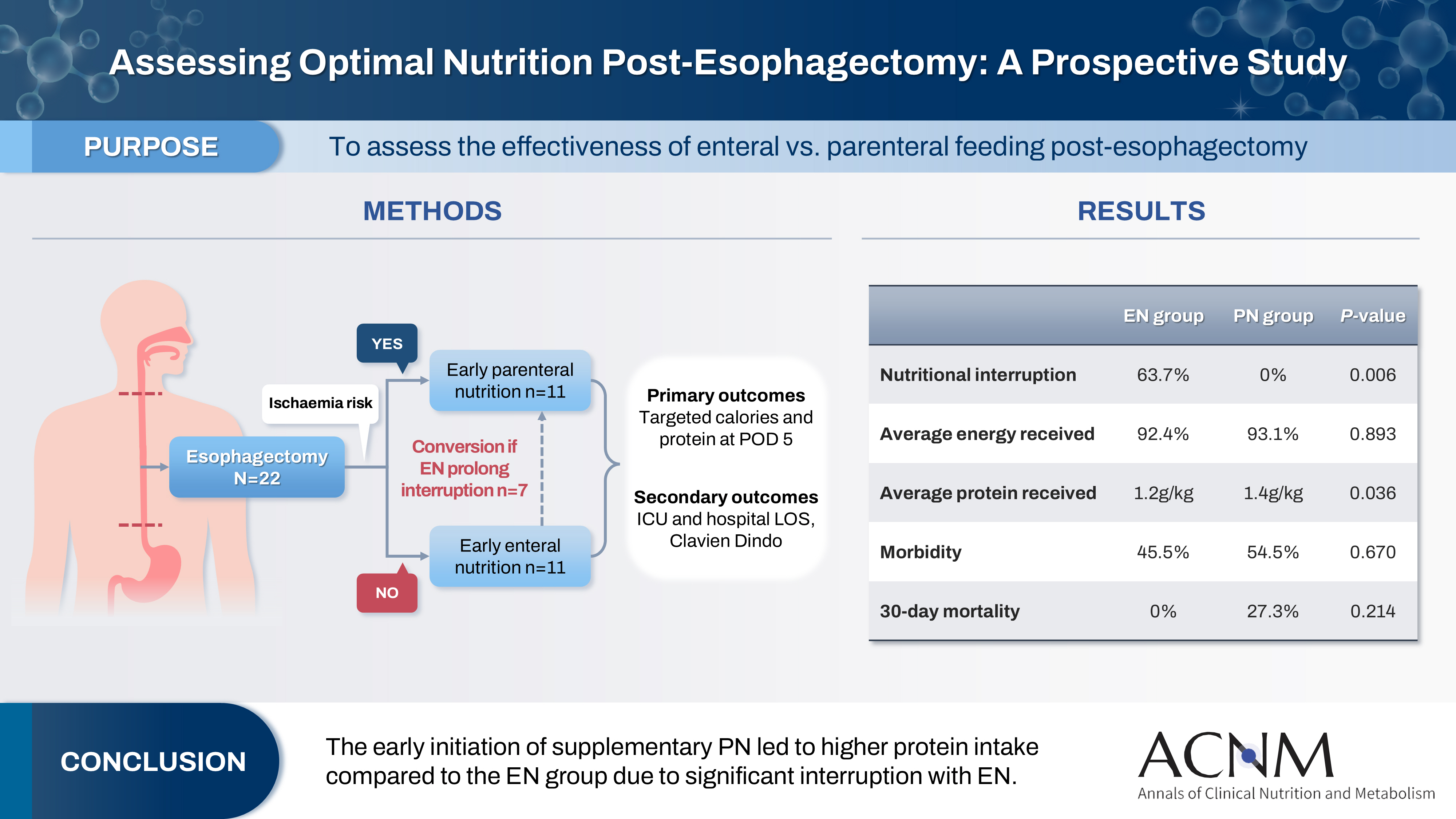
- Comparison of efficacy of enteral versus parenteral nutrition in patients after esophagectomy in Malaysia: a prospective cohort study
- Ramizah Mohd Shariff, Sze Chee Tee, Shukri Jahit Mohammad, Khei Choong Khong
- Ann Clin Nutr Metab 2025;17(1):41-49. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 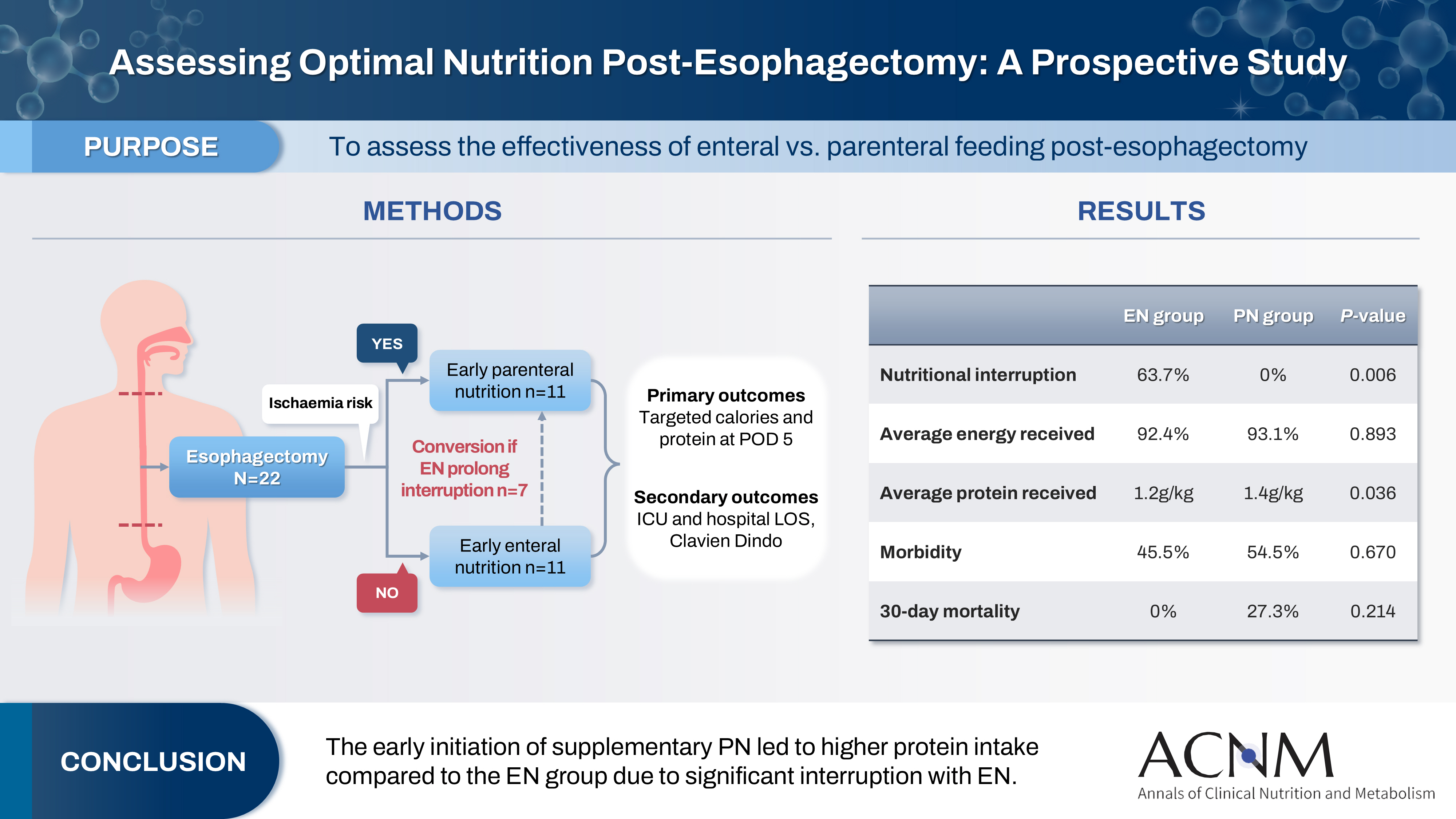
- Purpose
This study aims to assess the effectiveness of enteral versus parenteral feeding in patients after esophagectomy.
Methods
This a prospective cohort study of post-esophagectomy intensive care unit (ICU) patients over 12 months in the National Cancer Institute, Malaysia. Early enteral feeding followed the Enhanced Recovery After Surgery protocol, and parenteral nutrition (PN) was considered if there was a risk for conduit ischemia. It compared the effectiveness of enteral versus PN following esophagectomy, and assessed the correlations between biochemical nutritional markers and hospital lengths of stay or ventilation days.
Results
It included two cohorts receiving PN (n=11) or enteral nutrition (EN) (n=11) following elective esophagectomy. Preoperative weight, body mass index, and Subjective Global Assessment were higher in the EN group (P=0.033, P=0.021, P=0.031, respectively). Nutritional interruption occurred more frequently in the EN group (63.7%) compared to the PN group (P=0.001). Mean levels of energy and protein received were 93.1 kcal/kg and 1.4 g/kg for PN versus 92.4 kcal/kg and 1.2 g/kg for EN (P=0.893, P=0.036). The median lengths of ICU stay (P=0.688) and postoperative stay (P=0.947) between groups showed no significant difference. In addition, 30-day mortality (P=0.214) and other postoperative complications (P>0.05) were comparable in the two groups.
Conclusion
Early initiation of supplementary PN due to significant interruption in EN led to higher protein intake compared to the EN group. However, there were no significant differences in postoperative outcomes, including 30-day mortality, ICU length of stay, and ventilation days. PN ensures adequate nutritional intake, especially in terms of protein delivery, without adversely affecting postoperative recovery and clinical outcomes. -
Citations
Citations to this article as recorded by- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
Ioana Alexandra Prisacariu, Konstantinos Eleftherios Koumarelas, Konstantinos Argyriou, Alexandros Charalabopoulos, Grigorios Christodoulidis
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
- 5,567 View
- 67 Download
- 1 Crossref

- Perioperative nutritional practice of surgeons in Korea: a survey study
- Ji-Hyeon Park, Mi Ran Jung, Sang Hyun Kim, Hongbeom Kim, Gyeongsil Lee, Jae-Seok Min, Heung-Kwon Oh, Jung Hoon Bae, Yoona Chung, Dong-Seok Han, Seung Wan Ryu, The External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(3):134-148. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.134
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Enhanced recovery after surgery (ERAS) protocols advocate reduced fasting and early nutrition to improve recovery in surgical patients. However, data on ERAS implementation among Korean surgeons performing major abdominal surgeries remain sparse.
Methods: A survey conducted by the External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition assessed perioperative nutritional practices among 389 Korean general surgeons from February to September 2023. The survey covered preoperative fasting, carbohydrate drinks, nasogastric tube use, postoperative dietary progression, parenteral nutrition (PN), and oral supplements, yielding 551 responses stratified by specialty.
Results: More than 80% of respondents practiced “midnight NPO (Nil Per Os)” fasting, often at the anesthesiology department’s request, while 70%–80% reported no use of preoperative carbohydrate drinks. Most surgeons began dietary progression with water on postoperative day one, advancing to a liquid or soft diet by day two. PN was routinely prescribed by 49% of respondents, with a common dosage of 1,000–1,500 kcal/d. Oral supplements were selectively provided, with 21% of surgeons prescribing them universally.
Conclusion: The results reveal significant variability in perioperative nutrition practices across Korean surgical specialties, with many adhering to traditional practices despite ERAS guidelines. These findings highlight a need for standardized guidelines in Korea to optimize perioperative nutritional support and improve patient recovery outcomes following major abdominal surgeries. -
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Perioperative nutrition practices in gastrointestinal cancer surgery: A nationwide survey among German surgical departments
Rahel Maria Strobel, Katharina Beyer, Johannes Christian Lauscher, Marc Martignoni, Christoph Reißfelder, Tim Vilz, Arved Weimann, Maria Wobith
Langenbeck's Archives of Surgery.2025;[Epub] CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 6,755 View
- 88 Download
- 2 Crossref

- Changes in perceptions of taste after bariatric surgery: a narrative review
- Young Suk Park
- Ann Clin Nutr Metab 2024;16(3):120-124. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.120
-
 Abstract
Abstract
 PDF
PDF - Purpose: Bariatric surgery effectively treats severe obesity, leading to significant weight loss and improved comorbidities. However, many patients experience postoperative alterations in taste perception, affecting food selection and eating behavior. This narrative review examines the current understanding of taste perception changes following bariatric surgery, including patterns, potential mechanisms, impact on weight loss outcomes, and implications for patient care.
Current concept: Changes in taste perception are frequently reported after bariatric procedures, with prevalence rates from 36% to 72%. Common alterations involve decreased preference and increased sensitivity to sweet and fatty tastes, potentially leading to reduced calorie intake and healthier food choices. Persistence of these changes varies and may depend on surgery type, with Roux-en-Y gastric bypass patients often experiencing more substantial effects than sleeve gastrectomy patients. Potential mechanisms include alterations in gut hormone secretion (e.g., GLP-1, peptide YY, ghrelin), modifications in neural pathways (e.g., vagus nerve), and shifts in the gut microbiome. These factors may collectively influence taste sensitivity and preferences, contributing to weight loss outcomes. Altered reward processing may reduce the appeal of high-calorie foods.
Conclusion: Alterations in taste perception are common after bariatric surgery and may significantly impact dietary behaviors, weight loss, and quality of life. While exact mechanisms are not fully understood, changes in gut hormones, neural pathways, and microbiota are likely involved. Patient counseling and postoperative management of bariatric surgery patients should address potential changes in taste. Further research is needed to elucidate the long-term impacts of taste alterations on weight-loss maintenance and nutritional status.
- 5,836 View
- 60 Download

- The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
- Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(2):22-42. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.22
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition was established to develop ERAS guidelines tailored to the Korean context. This guideline focuses on creating the most current evidence-based practice guidelines for ERAS based on systematic reviews. All key questions targeted randomized controlled trials (RCTs) exclusively. If fewer than two RCTs were available, studies using propensity score matching were also included. Recommendations for each key question were marked with strength of recommendation and level of evidence following internal and external review processes by the committee.
-
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Optimizing postoperative pain management in minimally invasive colorectal surgery
Soo Young Lee
Annals of Coloproctology.2024; 40(6): 525. CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 10,552 View
- 137 Download
- 2 Crossref

- Comparative assessment of nutritional characteristics of critically ill patients at admission and discharge from the neurosurgical intensive care unit in Korea: a comparison study
- Eunjoo Bae, Jinyoung Jang, Miyeon Kim, Seongsuk Kang, Kumhee Son, Taegon Kim, Hyunjung Lim
- Ann Clin Nutr Metab 2023;15(3):97-108. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.97
-
 Abstract
Abstract
 PDF
PDF - Purpose: Patients in neurosurgical (NS) intensive care units (ICUs) experience considerable energy and protein deficits associated with adverse outcomes. This study aimed to compare the nutritional status of patients at admission to (baseline) and discharge from the NS ICU.
Methods: This was a single-center, retrospective, before and after study of patients admitted in the NS ICU of the CHA Bundang Medical Center, from January 31, 2019, to February 28, 2020. All anthropometric data, biochemical data, clinical data, and dietary data were collected during the NS ICU stay. Specifically, we investigated the cumulative caloric deficit rate, phase angle and skeletal muscle index as indicators of lean muscle mass, and nitrogen balance according to demographic and clinical characteristics.
Results: A total of 140 NS patients were studied. Calf circumference decreased from 31.4±4.2 cm at baseline to 30.2±4.0 cm at discharge (P<0.001). Energy supply rate increased from 44.4% at baseline to 89.2% at discharge. Phase angle (PhA) patients with an modified Nutrition Risk in the Critically ill (mNUTRIC) score≤5 group had significantly lower PhA values than those with an mNUTRIC score>5 (P=0.005).
Conclusion: Although clinical and dietary parameters of patients in the NS ICU improved from baseline to discharge, anthropometric and biochemical markers of lean muscle mass and nutritional status decreased. PhA and nitrogen balance difference values were significantly different between those with an mNUTRIC score≤5 and those with an mNUTRIC score>5. These data indicate that the nutritional risk of critically ill patients increases during hospitalization in the NS ICU. -
Citations
Citations to this article as recorded by- Association between the Modified NUTRIC Score (mNUTRIC) and Clinical Outcomes in a Mixed Intensive Care Unit: A Retrospective Cohort Study
Thanh Luan Nguyen, Quang Dai Le, Trang Nguyen Hoai Dinh, Van Hoang Nam Ho, Cong Dang Tran, Van Phieu Duong, Hoang Ngoc Thao Duong, Phuc Tuong Pham, Thi Phuong Thao Le, Tuyet Phuong Bui
SN Comprehensive Clinical Medicine.2026;[Epub] CrossRef - A Review on the Effects of Multiple Nutritional Scores on Wound Healing after Neurosurgery.
Jingqian Ye, Bo Ning , Jianwen Zhi
International Journal of Biology and Life Sciences.2025; 9(2): 82. CrossRef - Transition from Enteral to Oral Nutrition in Intensive Care and Post Intensive Care Patients: A Scoping Review
Gioia Vinci, Nataliia Yakovenko, Elisabeth De Waele, Reto Stocker
Nutrients.2025; 17(11): 1780. CrossRef
- Association between the Modified NUTRIC Score (mNUTRIC) and Clinical Outcomes in a Mixed Intensive Care Unit: A Retrospective Cohort Study
- 3,974 View
- 29 Download
- 3 Crossref

- Role of preoperative immunonutrition in patients with colorectal cancer: a narrative review
- Soo Young Lee, Hyeung-min Park, Chang Hyun Kim, Hyeong Rok Kim
- Ann Clin Nutr Metab 2023;15(2):46-50. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: Colorectal cancer surgery presents challenges due to surgical stress and immunosuppression, leading to postoperative complications. Nutrition is crucial for colorectal cancer patients who are prone to malnutrition. This study aims to provide a comprehensive review of the role of preoperative immunonutrition in colorectal cancer surgery.
Current concept: Preoperative immunonutrition, consisting of immunonutrients such as arginine, ω-3 fatty acids, and nucleotides, has emerged as a potential strategy to enhance surgical outcomes by modulating immune responses and reducing complications. Current guidelines recommend preoperative oral nutritional supplements for major abdominal surgery and immunonutrition for nutritionally high-risk patients. Meta-analysis have demonstrated significant decreases in infectious complications and hospital stay durations with preoperative immunonutrition. However, limitations such as publication bias and heterogeneity in the previous studies should be considered. Further research should focus on the optimal timing, duration, and amount of immunonutrition; the patient populations that would benefit most; and the integration of immunonutrition into enhanced recovery after surgery protocols.
Conclusion: While preoperative immunonutrition shows promise, additional research is crucial to refine protocols and establish optimal clinical practice utilization. -
Citations
Citations to this article as recorded by- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Coloproctology.2025; 41(1): 3. CrossRef - Efficacy of preoperative immunonutrition in malnourished patients undergoing colorectal cancer surgery: a study protocol for a multicenter randomized clinical trial
Soo Young Lee, Chang Hyun Kim, Gi Won Ha, Soo Yeun Park, In Jun Yang, Jin Soo Kim, Gyung Mo Son, Sung Il Kang, Sung Uk Bae
Trials.2025;[Epub] CrossRef - The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park
Annals of Clinical Nutrition and Metabolism.2024; 16(2): 22. CrossRef
- The 2024 Korean Enhanced Recovery After Surgery (ERAS) guidelines for colorectal cancer: a secondary publication
- 15,626 View
- 99 Download
- 3 Crossref

- Development of the Korean Version of the Gastrointestinal Quality of Life Index Questionnaire
- In Jun Yang, Heung-Kwon Oh, Jeehye Lee, Jung Wook Suh, Hong-min Ahn, Hyeonjeong Park, Hyun Hee Sim, Yong Beom Cho, In Kyu Lee, Seungbum Ryoo, Dong-Won Lee, Duck-Woo Kim, Sung-Bum Kang
- Ann Clin Nutr Metab 2022;14(1):32-37. Published online June 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.1.32
-
 Abstract
Abstract
 PDF
PDF - Purpose: To establish a standardized quality of life measurement that allows global cross-study comparisons, we translated the Gastrointestinal Quality of Life Index (GIQLI) into Korean and linguistically validated the Korean version of the GIQLI (K-GIQLI) in patients who underwent colorectal surgery.
Materials and Methods: A cross-cultural adaptation of the original GIQLI was created based on the established guidelines. Based on participation in a cognitive interview, 20 patients with colorectal cancer were enrolled in the study. To ensure that the Korean version of the questionnaire was understood as intended, the time needed to complete the questionnaire was measured, and three additional items related to comprehension were added.
Results: From May to July 2021, two translators, whose native language was Korean translated the GIQLI items into Korean, and a native English editor who had no knowledge of the original questionnaire translated the items back into English. In the cognitive interview, the median age of the patients was 61.8 (range: 44~82) years, and the median time required to complete the questionnaire was 6.5 (range: 5~10) min. For the language and cultural adaptation process, the participants’ comprehension of the questionnaire was measured on a scale of 1~5, with a mean score of 4 (range: 3~4).
Conclusion: The K-GIQLI was developed and did not exhibit a significant difference from the original English version in terms of social, linguistic, and cultural differences between the Western world and Republic of Korea. -
Citations
Citations to this article as recorded by- Comparison of laparoscopic and robotic surgery of choledochal cyst in pediatrics: single center experience
Jiyong Jang, Dayoung Ko, Joong Kee Youn, Hee-Beom Yang, Hyun-Young Kim
Surgical Endoscopy.2026; 40(1): 462. CrossRef - Longitudinal quality of life assessment after laparoscopic colorectal cancer surgery using the Gastrointestinal Quality of Life Index questionnaire: A multicentre prospective study
Tae‐Gyun Lee, Seung‐Bum Ryoo, Heung‐Kwon Oh, Yong Beom Cho, Chang Hyun Kim, Ju Hyun Lee, Hong‐Min Ahn, Hye‐Rim Shin, Mi Jeong Choi, Min Hyeong Jo, Duck‐Woo Kim, Sung‐Bum Kang
Colorectal Disease.2025;[Epub] CrossRef
- Comparison of laparoscopic and robotic surgery of choledochal cyst in pediatrics: single center experience
- 2,404 View
- 19 Download
- 2 Crossref

- Effect of Probiotics/Synbiotics on Postoperative Outcomes in Patients Undergoing Abdominal Surgery
- In Ja Park
- Ann Clin Nutr Metab 2022;14(1):10-19. Published online June 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.1.10
-
 Abstract
Abstract
 PDF
PDF - Environmental factors, drugs, diet, and surgery alter the composition of the gut microbiota leading to the production of different metabolites or toxins that can cause disease or delay postoperative recovery. Surgical damage leads to gut barrier disruption, increased intestinal permeability, gut microbial imbalance, and immunologic compromise of the host with subsequent bacterial translocation from the gastrointestinal tract to systemic circulation. Therefore, perioperative stabilization of the intestinal microbiota is a potential method of reducing postoperative complication rates. Probiotics have been proposed as a viable option for prophylaxis of postoperative infections through increased intestinal motility to prevent bacterial overgrowth, improve gut barrier function, and modulate immune response. This review investigates microbial changes after surgery and the influence of probiotics on postoperative microbial composition. Infectious postoperative complications and immunologic changes related to probiotics/synbiotics were also reviewed in patients who underwent abdominal surgery.
-
Citations
Citations to this article as recorded by- Postoperative gut dysbiosis and its clinical implications, with an emphasis on probiotic strategies in gastric cancer patients undergoing gastrectomy: a narrative review
Cheong Ah Oh
Ann Clin Nutr Metab.2025; 17(2): 114. CrossRef - Formoterol promotes mitochondrial biogenesis, improves liver regeneration, and suppresses liver injury and inflammation after liver resection in mice with endotoxemia
Amir K Richardson
International Journal of Physiology, Pathophysiology and Pharmacology.2025; 17(4): 131. CrossRef - Probiotics in the Management of Surgery- Induced Diarrhea: Efficacy and Clinical Applications
P. Dhivyaprasath, Gayathri R, Poovitha M, Rabiyath Riswana M, Sabithra P, Susitha R
International Journal of Innovative Science and Research Technology.2024; : 1482. CrossRef
- Postoperative gut dysbiosis and its clinical implications, with an emphasis on probiotic strategies in gastric cancer patients undergoing gastrectomy: a narrative review
- 12,181 View
- 127 Download
- 3 Crossref

- Perioperative Management of Morbidly Obese Patients during Major Abdominal Surgery
- Byeong-Gon Na, Sang-Jae Park
- Ann Clin Nutr Metab 2021;13(2):26-33. Published online December 31, 2021
- DOI: https://doi.org/10.15747/ACNM.2021.13.2.26
-
 Abstract
Abstract
 PDF
PDF - The population with obesity is seeing a steady increase globally. Obesity is known to be associated with morbidity and mortality after major abdominal surgery, and this correlation becomes more prominent in morbidly obese (MO) patients. Accordingly, adequate preoperative evaluation and preparation should be performed with an understanding of the pathophysiological changes associated with the MO. Precise surgery and adequate postoperative management are also mandatory to reduce complications and unplanned readmissions. However, adequate guidelines for the perioperative management of MO patients undergoing major abdominal surgery are lacking. We provide an overview of the pathophysiologic changes and practical guidelines on the perioperative management of major abdominal surgery in MO patients.
-
Citations
Citations to this article as recorded by- Spinal Anesthesia in Morbidly Obese Patients: Risks, Benefits, and Future Perspectives
T. K. Nematulloev, M. M. Matlubov
Innovative Medicine of Kuban.2025; 10(3): 99. CrossRef - FEATURES OF PREOPERATIVE MANAGEMENT FOR ABDOMINAL SURGERY IN OBESE PATIENTS
Sergii Khimich, Ihor Malyshevskyi, Olena Katelian
Актуальні проблеми сучасної медицини: Вісник Української медичної стоматологічної академії.2025; 25(3): 111. CrossRef - Multiplicative effect of frailty and obesity on postoperative mortality following spine surgery: a deep dive into the frailty, obesity, and Clavien-Dindo dynamic
Oluwafemi P. Owodunni, Evan N. Courville, Uchenna Peter-Okaka, Christian B. Ricks, Meic H. Schmidt, Christian A. Bowers
International Journal of Obesity.2024; 48(3): 360. CrossRef
- Spinal Anesthesia in Morbidly Obese Patients: Risks, Benefits, and Future Perspectives
- 7,421 View
- 88 Download
- 3 Crossref

- Nutritional Status of Patients with Hepatobiliary-Pancreatic Surgical Disease
- Sang Soo Eom, Yong Chan Shin, Chang-Sup Lim, In Woong Han, Woohyun Jung, Yoonhyeong Byun, Dong Wook Choi, Jin Seok Heo, Hongbeom Kim
- Surg Metab Nutr 2020;11(2):46-52. Published online December 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.2.46
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study examined the nutritional status of patients with hepatobiliary-pancreatic diseases before surgery to establish basic reference data.
Materials and Methods: This study evaluated retrospectively 2,322 patients admitted for hepatobiliary-pancreatic surgery between 2014 and 2016 at four Korean medical institutions using the body mass index (BMI) score. The prognostic nutrition index (PNI) was calculated in patients diagnosed with malignant diseases.
Results: The mean BMI was 24.0 kg/m2 (range, 13.2~39.1 kg/m2). The patients were classified as low BMI (<21.5 kg/ m2, below 25 percentile), intermediate BMI (21.5~25.5 kg/m2), and high BMI (>25.5 kg/m2, above 75 percentile). There were significant differences in the age, sex distribution, ASA classification, type of hospitalization, biliary drainage, organ, and pathology diagnosis between the pairs among the low, intermediate, and high BMI groups. Among the three BMI groups, the complication rate of the low BMI group was highest (34.4% vs. 29.7% vs. 25.8% P=0.005). The median lengths of hospital stay in the low, intermediate, and high BMI groups were 9, 9, and 7 days, respectively (P<0.001). Multivariate analysis revealed the risk factors of the low BMI group to be a higher ASA classification, biliary drainage, pancreatic disease, and malignant disease. The group with PNI<45 had significantly longer hospital stays than the group with PNI≥45 (P<0.001).
Conclusion: Patients with a low BMI had a higher ASA classification, preoperative biliary drainage, pancreatic disease, and malignant disease. The low PNI group had significantly longer hospital stays than the high PNI group. Screening of the preoperative nutritional status is necessary for assessing the risk of malnutrition and its treatment. -
Citations
Citations to this article as recorded by- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
Hengwei Jin, Xu Sun, Chang Fu, Changqing Fan, Junhong Chen, Ziyu Zhang, Yibo Yang, Xiaoyu Fan, Ye He, Siyuan Yin, Kai Liu
Surgical Endoscopy.2025; 39(8): 5107. CrossRef
- Machine learning-based prediction model for post-ERCP cholangitis in patients with malignant biliary obstruction: a retrospective multicenter study
- 1,424 View
- 19 Download
- 1 Crossref

- Status of Nutritional Support after Emergency Gastrointestinal Surgery in Korea: Retrospective Multicenter Study
- Dae Sang Lee, Young Eun Park, Kyoung Hoon Lim, Ye Rim Chang, Suk-Kyung Hong, Minchang Kang, Jung-Min Bae, Ji Young Jang, Young Goun Jo, Ki Hoon Kim, Gil Jae Lee
- Surg Metab Nutr 2020;11(1):1-6. Published online June 30, 2020
- DOI: https://doi.org/10.18858/smn.2020.11.1.1
-
 Abstract
Abstract
 PDF
PDF - Purpose: Surgery itself causes an inflammatory response to an injury to the patient that leads to a stress metabolic state. Emergency gastrointestinal surgery may cause complications, such as ileus, bowel obstruction, ischemia, or anastomotic leakage, resulting in a delayed oral diet or poor overall nutrition. This study investigated the route of nutrition for patients who underwent emergency gastrointestinal surgery and when to provide nutrition after surgery.
Materials and Methods: Ten hospitals collected data retrospectively on the nutritional status and nutritional status of patients undergoing emergency gastrointestinal surgery for one year from January to December 2016. The clinical outcomes of the nutrient supply method, duration of supply, and type of surgery were performed. The dates from the time of surgery to the start of enteral nutrition, oral nutrition, and parenteral nutrition were calculated.
Results: Of 706 patients, there were 187 (26.5%) trauma patients, of which 63.5% were male. The onset of nutrition began after an average of 10.7 days postoperatively and after an average of 12.1 days of enteral nutrition. On average, it took 7.7 days to provide adequate calories, of which 63.3% had achieved adequate calories within a week. In the case of minimally invasive surgery, such as laparoscopic surgery, the adequate calorie supply time was five days, which was reached within one week.
Conclusion: In a retrospective multicenter analysis, the patients who underwent emergency gastrointestinal surgery had a late start of oral or enteral nutrition, and the ratio of adequate calorie supply within a week was low.
- 690 View
- 2 Download

- Survey and Analysis of the Application and Implementations of Enhanced Recovery after Surgery (ERAS) Program for Surgical Patients in the Major Hospitals in Korea
- Eun Young Kim, In Kyu Lee
- Surg Metab Nutr 2019;10(2):32-45. Published online December 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.2.32
-
 Abstract
Abstract
 PDF
PDF Purpose:
A questionnaire survey was conducted using e-mail to investigate the application status of ERAS in Korea and its implementation by their institution. The perceptions of ERAS by medical staff and the factors that interfered with the application of ERAS were investigated.
Materials and Methods:
From July 2017 to March 2019, a questionnaire was sent by e-mail to members of the KSSMN. This consisted of 41 questions divided into three parts to investigate 1) respondents’ prior knowledge and understanding of ERAS, 2) actual components of ERAS and its clinical application, and 3) performance and preference of the respondents to ERAS. The items were categorized into “high acceptance” when more than 75% of respondents answered “yes”, or the items into “low acceptance” when less than 25% answered “no”.
Results:
Overall, 86 participants completed the survey. Of these, 59(68.6%) had prior knowledge of ERAS and 29 (33.7%) applied ERAS clinically. Seventy (81.4%) and 40 (46.5%) answered that ERAS would have a positive effect on shortening the hospital stay and reducing the number of complications. Seventy four (86%) indicated that they would implement ERAS in the future. The factors impeding the implementation of ERAS were a lack of understanding of physicians and a shortage of manpower and resources for ERAS.
Conclusion:
The ERAS implementation rate and awareness level of surgeons were low, but the positive expectations of the clinical efficacy of ERAS and the wiliness to accept were high. Overall, it would be necessary to cooperate with institutions to improve the manpower and resources, and supplement the education to overcome the lack of awareness, which has been pointed out as an obstacle to the implementation of ERAS.
-
Citations
Citations to this article as recorded by- Enhancing postoperative recovery with multimodal prehabilitation: the journey begins before surgery
Ah-Reum Cho, Wariya Vongchaiudomchoke, Detlef Balde, Do Jun Kim, Francesco Carli
Korean Journal of Anesthesiology.2025; 78(5): 401. CrossRef - Challenging issues of implementing enhanced recovery after surgery programs in South Korea
Soo-Hyuk Yoon, Ho-Jin Lee
Anesthesia and Pain Medicine.2024; 19(1): 24. CrossRef - Perioperative nutritional practice of surgeons in Korea: a survey study
Ji-Hyeon Park, Mi Ran Jung, Sang Hyun Kim, Hongbeom Kim, Gyeongsil Lee, Jae-Seok Min, Heung-Kwon Oh, Jung Hoon Bae, Yoona Chung, Dong-Seok Han, Seung Wan Ryu
Annals of Clinical Nutrition and Metabolism.2024; 16(3): 134. CrossRef - Effects of the Enhanced Recovery After Surgery (ERAS) Program for Colorectal Cancer Patients Undergoing Laparoscopic Surgery
Jeongwon Yeom, Hee-Sook Lim
Clinical Nutrition Research.2022; 11(2): 75. CrossRef - Effect of Non-contact Korean Medical Treatment for Patients Recovering at Home with Positive Coronavirus Disease 2019 Diagnostic Test Results at a Local Public Health Center : A Retrospective Chart Review
Chaeheun Jeon, Daejun Choi, Gyeongmuk Kim, Hyejin Kim, Jungtae Leem, Gyoo-yong Chi
Journal of Physiology & Pathology in Korean Medicine.2022; 36(4): 130. CrossRef - Perception and implementation status of enhanced recovery after surgery
Eun Young Kim
Journal of the Korean Medical Association.2021; 64(12): 826. CrossRef - Background for the introduction of enhanced recovery after surgery and patient outcomes
Do Joong Park
Journal of the Korean Medical Association.2021; 64(12): 801. CrossRef
- Enhancing postoperative recovery with multimodal prehabilitation: the journey begins before surgery
- 1,138 View
- 19 Download
- 7 Crossref

- Major Surgery in Sarcopenic Patients
- Kyung Won Seo
- Surg Metab Nutr 2019;10(1):5-8. Published online June 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.1.5
-
 Abstract
Abstract
 PDF
PDF Sarcopenia refers to reduced muscle mass in the elderly population, and this malady is of great interest in clinical course, including postoperative complications and mortality when treating major cancer in the elderly. The definition of sarcopenia varies according to the method of measuring muscle mass, and the skeletal muscle index (SMI) tends to be extensively used in retrospective studies. In many reports, sarcopenia has been reported to be a poor prognostic factor after gastrectomy, colectomy, pancreatectomy and liver transplantation, with regards to complications and the length of the hospital stay. Additionally, patients suffering from sarcopenia have a higher medical burden due to their poor clinical outcome after surgery. To overcome these difficulties, nutritional support and exercise training to improve sarcopenia before surgery is helpful, and so further studies that focus on these treatments need to be conducted.
- 801 View
- 0 Download

- Nutritional Assessment of Critically Ill Patients after Abdominal Surgery and Predisposing Factors of Prolonged ICU Stay after Surgery
- Sung Eun Park, In Kyu Lee, Eun Young Kim
- Surg Metab Nutr 2018;9(2):68-74. Published online December 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.2.68
-
 Abstract
Abstract
 PDF
PDF Purpose:
Patients in prolonged intensive care unit stay were vulnerable to malnutrition which deteriorated recovery and postoperative outcomes. The purpose of this study was to evaluate nutritional status in surgical patients entering the intensive care unit, and to identify the risk factors that influence prolonged intensive care unit stay.
Materials and Methods:
From January 2016 to June 2018, 740 patients (age≥18 years) who were admitted to our surgical intensive care unit after abdominal surgery with general anesthesia (≥4 hours) were enrolled. Patients were classified into short-term stay group (≤4 days) and long-term stay group (>4 days). These groups were analyzed and compared with patient factors and postoperative outcomes and the multivariate analysis was performed to assess the risk factors for prolonged intensive care unit stay.
Results:
A total of 119 patients were analyzed. The univariate and multivariate analysis showed that dialysis status (Odds ratio 7.684, 95% confidence interval 1.038∼1.103, P=0.013), total lymphocyte count (Odds ratio 0.999, 95% confidence interval 0.998∼1.000, P=0.047), and intraoperative transfusion (Odds ratio 1.002, 95% confidence interval 1.001∼1.002, P=0.000) were associated with prolonged intensive care unit stay. Lone-term stay group were significantly longer hospital stay and higher hospital morbidity rate than short-term stay group.
Conclusion:
Patients with risk factors of prolonged intensive care unit stay included dialysis status, low total lymphocyte count, a large amount of transfusion would be more interested and the active intervention such as early nutritional evaluation and adequate nutritional support should be needed.
- 693 View
- 2 Download

- Is Postoperative Albumin Level Related with Surgical Site Infection?
- Kyungtae CHO, Sung Woo CHO, Sangchul YUN, Suyeon Park
- Surg Metab Nutr 2018;9(2):59-67. Published online December 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.2.59
-
 Abstract
Abstract
 PDF
PDF Purpose:
Surgical site infection (SSI) is a hospital-acquired infection (HAI) associated with increased mortality, length of hospital stay, and cost of hospitalization. The aim of this study was to identify the value of albumin as an indicator of the nutritional status, postoperative C-reactive protein (CRP), and white blood cell (WBC) levels in predicting an outbreak of SSI and SSI-related epidemiology after colorectal surgery and identifying the risk factors for SSI.
Materials and Methods:
A total of 198 patients, who underwent colorectal surgery from September 1, 2015 to December 31, 2016, were included in the study. The patient identity, operation characteristics, and SSI data were analyzed retrospectively by a chart review and national SSI reporting sheet. The relationship of the SSI and clinical data was analyzed statistically, and the SSI detection time and post-operative inflammatory laboratory findings were analyzed individually using cumulative incidence analysis and cause-specific hazard model.
Results:
The incidence of SSI post colorectal surgery was 15.7% (31 out of 198 cases). Chronic renal failure (CRF), open surgery, long operation time, and stoma were identified as significant risk factors for SSI using univariate analysis. The CRF, long operation time, and stoma were significant risk factors according to multivariate analysis. The decrease in albumin on post-operative day (POD)#3 and CRP elevation on POD#4 were related to the early detection of SSI.
Conclusion:
The actual incidence of SSI might be higher than expected, particularly in cases where patients have several clinical and operative factors. In addition, the albumin level and multiple postoperative inflammation tests can be employed as an early predictors of SSI.
-
Citations
Citations to this article as recorded by- Serum Albumin Kinetics in Major Ovarian, Gastrointestinal, and Cervico Facial Cancer Surgery
Cyrus Motamed, Lucie Mariani, Stéphanie Suria, Gregoire Weil
International Journal of Environmental Research and Public Health.2022; 19(6): 3394. CrossRef
- Serum Albumin Kinetics in Major Ovarian, Gastrointestinal, and Cervico Facial Cancer Surgery
- 1,735 View
- 7 Download
- 1 Crossref

- Incidence and Management of Micronutrient Deficiencies in Post-bariatric Surgery Patients
- Young Suk Park, Ki Bum Park, Sa-Hong Min, Yoontaek Lee, Sang-Hoon Ahn, Do Joong Park, Hyung-Ho Kim
- J Clin Nutr 2017;9(2):48-55. Published online December 31, 2017
- DOI: https://doi.org/10.15747/jcn.2017.9.2.48
-
 Abstract
Abstract
 PDF
PDF Bariatric surgery is considered one of the most effective methods of achieving long-term weight loss in morbidly obese patients. Nevertheless, bariatric procedures are associated with a number of complications, and nutrient deficiencies can lead to deleterious consequences. Furthermore, the diet of patients prior to bariatric surgery is often of poor nutrition quality that does not meet the recommended dietary guidelines for micronutrient intake. Therefore, optimization of the postoperative nutritional status should begin before surgery. This review covers the essential information about micronutrient management in patients before and after bariatric surgery.
-
Citations
Citations to this article as recorded by- Nutritional Management after Bariatric Surgery
Young-Gil Son, Seung Wan Ryu
Journal of Metabolic and Bariatric Surgery.2018; 7(1): 32. CrossRef
- Nutritional Management after Bariatric Surgery
- 1,437 View
- 1 Download
- 1 Crossref

- Micronutrients Deficiencies in Bariatric Patients
- Yeon Ji Lee
- Surg Metab Nutr 2016;7(1):7-12. Published online June 30, 2016
- DOI: https://doi.org/10.18858/smn.2016.7.1.7
-
 Abstract
Abstract
 PDF
PDF Paradoxically, the obese are more susceptible to malnutrition. The more obese they are, the greater the risk for micronutrient deficiencies particularly in fat-soluble vitamins and anti-oxidants. Several micronutrient deficiencies could be worsened because of poor intake and absorption difficulty after bariatric surgery. Micronutrient deficiencies could not only decrease the effect of bariatric surgery but also cause various diseases such as anemia, neurologic impairment, or osteoporosis. Micronutrient deficiencies should be monitored, recognized, and corrected properly in bariatric patients in order to maximize the effect of surgery and improve the health-related quality of life.
- 698 View
- 2 Download

- Pilot Study for Safety and Efficacy of Newly Developed Oral Carbohydrate-Rich Solution Administration in Adult Surgery Patients
- Won-Bae Chang, Kyuwhan Jung, Sang-Hoon Ahn, Heung-Gwon Oh, Mi-Ok Yoon
- J Clin Nutr 2016;8(1):24-28. Published online April 30, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.1.24
-
 Abstract
Abstract
 PDF
PDF Purpose:
In surgical procedures under general anesthesia, 6 to 8 hours of a
nulla per os (NPO; nothing by mouth) has been regarded as essential for prevention of respiratory complication such as aspiration. However, recent studies have reported that oral intake of water and other clear fluids up to 2 hours before induction of anesthesia does not increase respiratory problems. The purpose of this pilot study is to investigate the safety and efficacy of a newly developed carbohydrate-rich solution in elective hernia repair surgery patients.Methods:
A group of 30 adult patients scheduled for elective surgeries under general anesthesia were enrolled. The enrolled study group of patients was permitted to drink a carbohydrate-rich solution until two hours before the operation without volume limitation. Respiratory complication was investigated in the patients using the carbohydrate-rich solution until two hours before induction of general anesthesia. The feelings of thirst, hunger sense were measured pre- and post-operatively. In addition, hoarseness of voice, nausea and vomiting were investigated post-operatively. Satisfaction regarding the short time of fasting was measured. Visual analogue scale (VAS) was used for measurement of these six variables.
Results:
No patients showed serious respiratory complication such as dyspnea, desaturation. Eight of 30 study group patients complained of mild hoarseness. Most symptoms of hoarseness were mild, with VAS score less than 3 out of 10. Two patients complained 5 out of 10. Six patients felt nausea and 1 patient had vomiting. Pre/post-operative hunger sense and thirst feeling were 1.63/1.60 and 1.90/5.76, respectively. The satisfaction score was 3.00 out of 4.
Conclusion:
Allowing the administration of an oral carbohydrate-rich solution in elective surgery patients requiring general anesthesia is safe without serious respiratory complications and effective in providing satisfaction.
-
Citations
Citations to this article as recorded by- The safety and effect of preoperative reduced fasting time by oral clear liquid administration in adult surgery patients: a randomized controlled trial
Donghyoun Lee, Soo-Jin Kim, Won-Bae Chang
Annals of Surgical Treatment and Research.2025; 109(1): 1. CrossRef - Oral high-carbohydrate solution as an alternative dietary modality in patients with acute pancreatitis
See Young Lee, Jaein Lee, Jae Hee Cho, Dong Ki Lee, Yeseul Seong, Sung Ill Jang
Pancreatology.2024; 24(7): 1003. CrossRef - Patient-reported outcome measures on intake of nutrition drink for nutritional supplements after periodontal surgery
Hyeong-Seok Kim, In-Woo Cho, Hyun-Seung Shin, Jung-Chul Park
Journal of Dental Rehabilitation and Applied Science.2016; 32(3): 176. CrossRef
- The safety and effect of preoperative reduced fasting time by oral clear liquid administration in adult surgery patients: a randomized controlled trial
- 1,732 View
- 1 Download
- 3 Crossref

- Enhanced Recovery After Surgery is Feasible in Laparoscopic Low Anterior Resection for Rectal Cancer
- Jeong Seon Jo, Soo Young Lee, Hun Jin Kim, Chang Hyun Kim, Young Jin Kim, Hyeong Rok Kim
- Surg Metab Nutr 2015;6(1):11-15. Published online June 30, 2015
- DOI: https://doi.org/10.18858/smn.2015.6.1.11
-
 Abstract
Abstract
 PDF
PDF Purpose:
The aim of this study was to compare short-term outcomes in patients who underwent laparoscopic assisted low anterior resection for colorectal cancer. The patients received either conventional perioperative care or the Enhanced Recovery After Surgery (ERAS) procedural care.
Materials and Methods:
A retrospective review was conducted in patients who underwent elective laparoscopic low anterior resection for colorectal cancer between May, 2011 and December, 2013. Patients were grouped and analyzed according to the perioperative care program of ERAS and conventional care.
Results:
A total of 81 patients received care via the ERAS pathway and 230 patients received care via conventional pathway. There was no significant difference in postoperative morbidity rates (P=0.381). The post-operative morbidity rates were 30.9% and 25.2% in the ERAS and conventional groups. No significant difference in hospital stay (9.0±6.8 vs. 8.6±3.5 days; P=0.575) was observed between the 2 groups.
Conclusion:
No short-term perioperative disadvantages were found for the ERAS program compared with the conventional perioperative care for colorectal cancer patients who underwent laparoscopic low anterior resection. (Surg Metab Nutr 2015;6:11-15)
- 823 View
- 4 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


