Indexed in:
Scopus, KCI, KoreaMed
Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
Guidelines
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part II. selection and initiation of enteral feeding routes
- Ja Kyung Min, Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Jung Mi Song, Hyunjung Kim, Jae Hak Kim, Kyung Won Seo, Sung Shin Kim, Chi-Min Park, Jeongyun Park, Eunjung Kim, Eunmi Sul, Sung-Sik Han, Jeong Wook Kim, Seungwan Ryu, Minji Seok, Jinhee Yoon, Eunhee Kong, Youn Soo Cho, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(3):165-171. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0037
-
 Abstract
Abstract
 PDF
PDF - Purpose
We developed evidence-based recommendations for selecting and initiating the enteral nutrition (EN) delivery route in adult and pediatric patients to improve safety and standardize practice in Korea.
Methods
Key questions covered feeding tube selection, methods to verify tube placement, confirmation in pediatric patients, and timing of EN following percutaneous endoscopic gastrostomy (PEG). Recommendations were drafted and refined through multidisciplinary expert consensus under the Korean Society for Parenteral and Enteral Nutrition (KSPEN).
Results
Feeding tube selection should be based on gastrointestinal anatomy, function, and expected EN duration. Short-term feeding is recommended with nasogastric or orogastric tubes, whereas long-term feeding should use percutaneous or surgical routes such as PEG. Tube position must always be verified before use, preferably with radiography or pH testing; auscultation alone is unreliable and should not be used. In pediatric patients, radiographic confirmation remains the gold standard, although pH testing and insertion-length assessment may be considered when imaging is not feasible. After PEG, EN can be initiated safely within 4 hours in both adults and children without increasing complications if trained staff monitor for leakage or infection.
Conclusion
This guideline offers a structured framework for safe and timely EN tailored to patient characteristics. Early verification and multidisciplinary collaboration help reduce complication, improving outcomes of EN therapy.
- 436 View
- 31 Download

- The 2024 Korean Enhanced Recovery After Surgery guidelines for hepatobiliary and pancreatic surgery
- Kwangpyo Hong, Hongbeom Kim, Hyung Sun Kim, Hae Won Lee, Ho Joong Choi, YoungRok Choi, Jae Do Yang, Sung-Moon Jeong, Dae Wook Hwang, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2025;17(3):172-180. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0034
-
 Abstract
Abstract
 PDF
PDF - Purpose
The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition has developed comprehensive guidelines for hepatobiliary and pancreatic (HBP) surgery by adapting established international protocols. These guidelines provide evidence-based recommendations specifically tailored to the Korean healthcare system and address perioperative management for both pancreatoduodenectomy and hepatectomy.
Methods
The HBP subcommittee reviewed existing international ERAS guidelines and conducted an adaptation process. Key questions were identified based on national survey results from Korean HBP surgeons and were prioritized according to clinical relevance. The committee focused on elements supported by moderate- to high-quality evidence with strong recommendation grades. Literature searches were conducted through January 2025, and evidence quality was evaluated using GRADE methodology. Four key questions underwent formal assessment, and eight additional questions were adapted from international guidelines.
Results
Twelve key questions were selected and addressed, covering critical perioperative care domains: prehabilitation, preoperative nutritional assessment and support, anti-thrombotic prophylaxis, prophylactic abdominal drainage, preoperative biliary drainage, smoking and alcohol cessation, pre-anesthetic medication, minimally invasive surgical approaches, prophylactic nasogastric intubation, postoperative glycemic control, perianastomotic drainage management, and early mobilization protocols. Each recommendation was assigned specific evidence levels and graded for strength. High-quality evidence supported strong recommendations for the routine avoidance of prophylactic drainage in uncomplicated hepatectomy, early drain removal after pancreatoduodenectomy in low-risk patients, elimination of routine nasogastric decompression, and the implementation of early mobilization strategies.
Conclusion
These Korean-adapted ERAS guidelines for HBP surgery are expected to standardize perioperative care, reduce postoperative complications, shorten hospital stays, and enhance overall patient outcomes across Korean healthcare institutions.
- 1,149 View
- 30 Download

Original Article
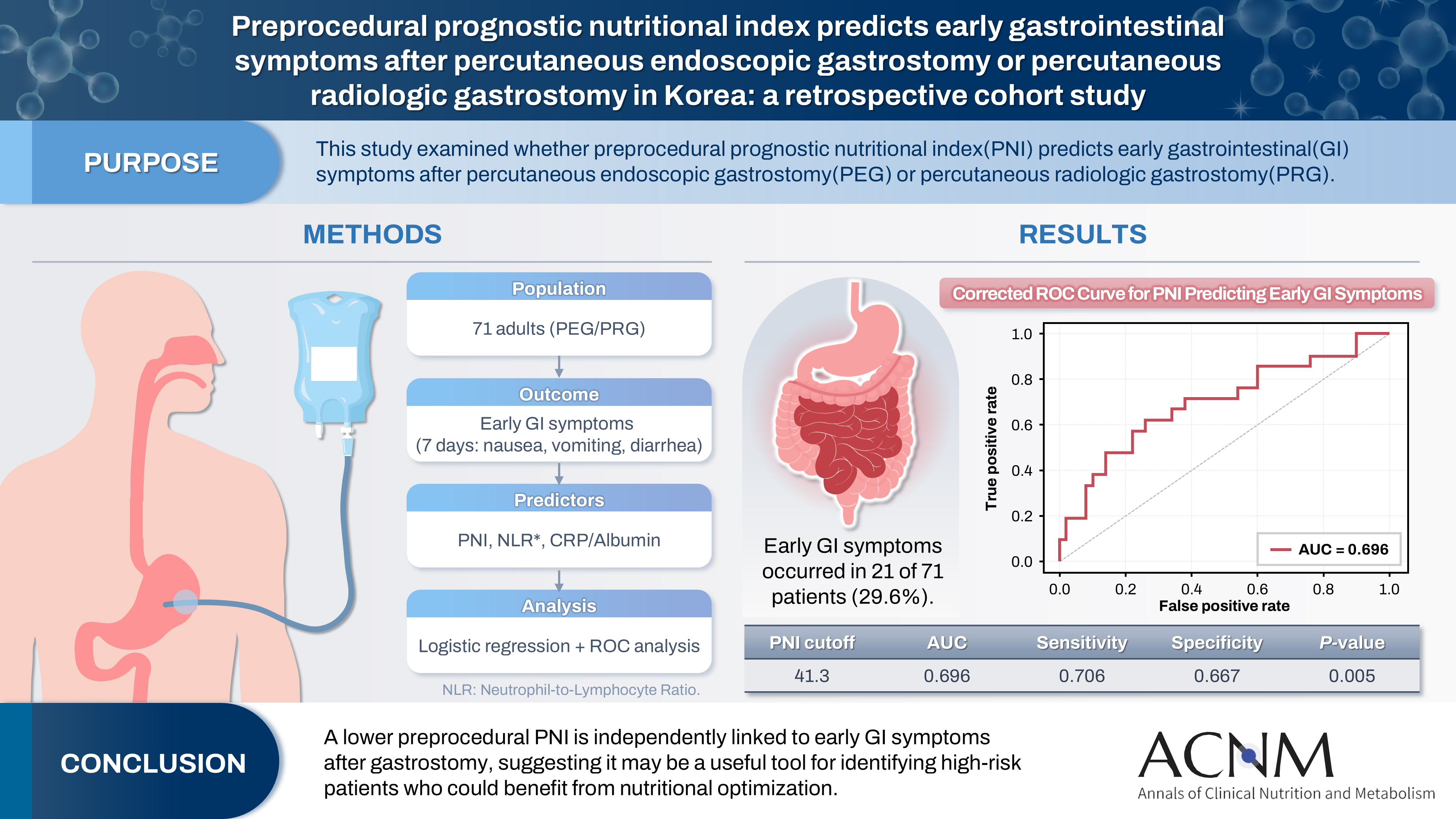
- Preprocedural prognostic nutritional index predicts early gastrointestinal symptoms after percutaneous endoscopic gastrostomy or percutaneous radiologic gastrostomy in Korea: a retrospective cohort study
- Yoonhong Kim, Jee Young Lee, Yeajin Moon, Seung Hun Lee, Kyung Won Seo, Ki Hyun Kim
- Ann Clin Nutr Metab 2025;17(3):196-202. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0032
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 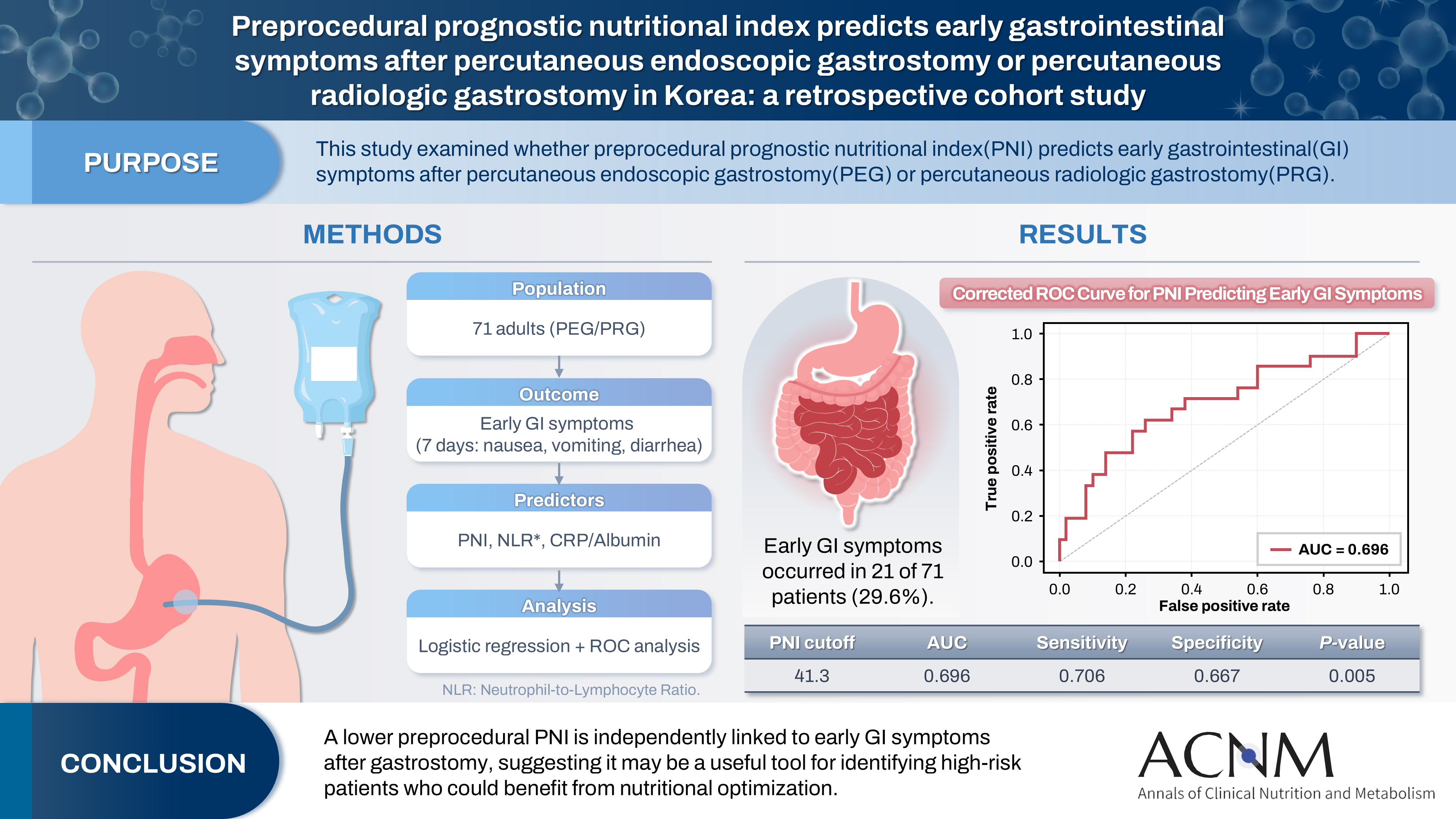
- Purpose
The prognostic nutritional index (PNI) reflects immunonutritional status and is a well-established predictor of surgical outcomes. Although its association with post-gastrostomy mortality has been documented, its relationship with early gastrointestinal (GI) symptoms remains unclear. This study aimed to evaluate whether the preprocedural PNI predicts early GI symptoms following percutaneous gastrostomy, including percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG).
Methods
This retrospective study included 71 adults who underwent PEG or PRG. Early GI symptoms, such as nausea, vomiting, and diarrhea, occurring within 7 days were recorded. The preprocedural PNI, neutrophil-to-lymphocyte ratio (NLR), and the C-reactive protein (CRP)-to-albumin ratio were analyzed using logistic regression to identify predictors. Receiver operating characteristic (ROC) analysis was performed to assess the PNI’s discriminative performance.
Results
Early GI symptoms occurred in 21 of 71 patients (29.6%). In univariate analysis, the PNI (P=0.009) and CRP-to-albumin ratio (P=0.018) were significant predictors, whereas NLR was not (P=0.125). After adjustment for potential confounders, including age, sex, body mass index, and NLR, the PNI remained an independent predictor of early GI symptoms (adjusted odds ratio, 0.90; 95% confidence interval, 0.83–0.98; P=0.021). ROC analysis for the PNI produced an area under the curve of 0.696, with an optimal cutoff value of 41.3 (sensitivity 70.6%, specificity 66.7%).
Conclusion
A lower preprocedural PNI is independently associated with the development of early GI symptoms after gastrostomy. The PNI may serve as a practical screening tool to identify high-risk patients who could benefit from preemptive nutritional optimization.
- 688 View
- 15 Download

Interesting image
- Penetration of a nasogastric tube by a stylet during insertion
- Akihide Takami, Haruka Tsuji, Kazuya Omura
- Ann Clin Nutr Metab 2025;17(3):210-211. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0029
- 255 View
- 8 Download

Original Articles
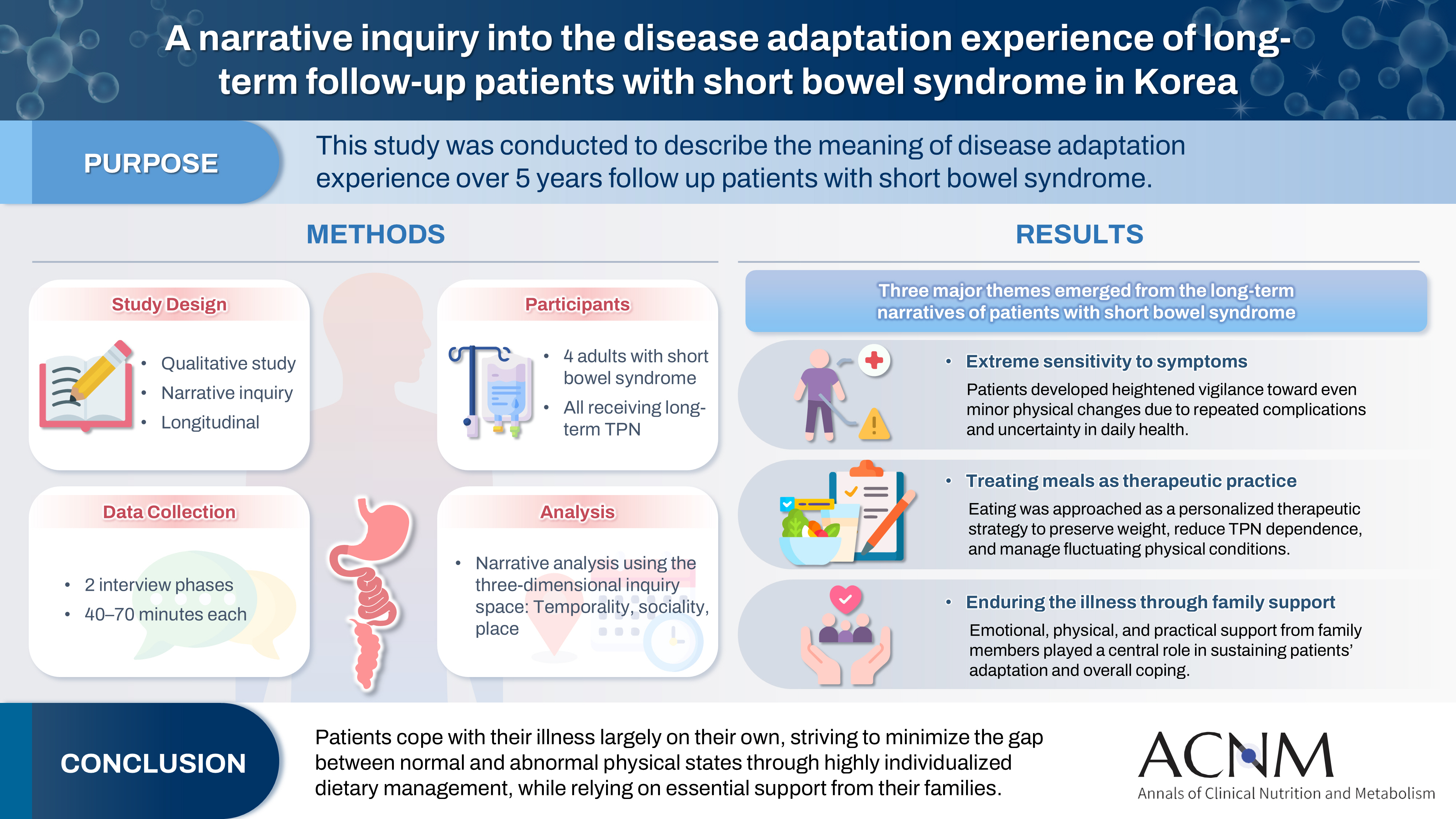
- A narrative inquiry into the disease adaptation experience of long-term follow-up patients with short bowel syndrome in Korea
- Eun-Mi Seol, Eunjung Kim
- Ann Clin Nutr Metab 2025;17(3):188-195. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0028
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 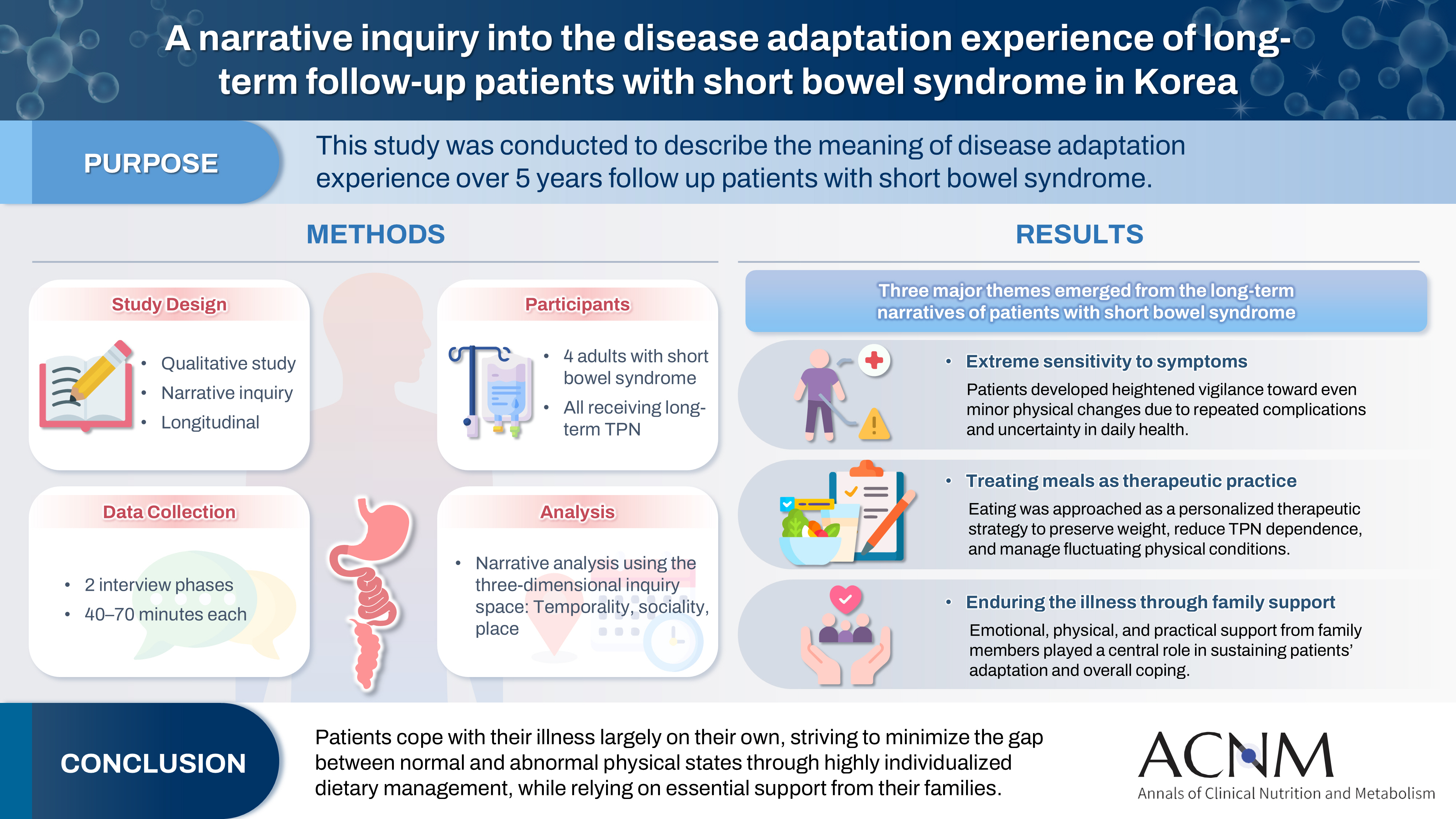
- Purpose
This study was conducted to describe the meaning of disease adaptation experience over a 5-year long-term follow-up of patients with short bowel syndrome.
Methods
Four patients were recruited from a tertiary hospital in Korea. This study was conducted through first and second interviews from January 2019 to July 2022. The transcribed data were analyzed using narrative methods.
Results
The mean age of the participants was 64 years, and the mean treatment period after small bowel resection was 100 months. The participants lost a mean of 19.3 kg body weight and all were receiving home total parenteral nutrition 2–7 days a week. The meaning of the experience of adapting to the disease for patients was found to be “extremely sensitive to the symptoms,” “considering eating food as another effective treatment method,” and “enduring the disease through family affection.”
Conclusion
Patients are struggling alone to cope with physical symptoms and adapt to their disease. For this, they are doing their best to narrow the gap between normal and abnormal physical conditions by thoroughly implementing diet therapy according to their physical characteristics. This entire process is supported by their families.
- 781 View
- 18 Download

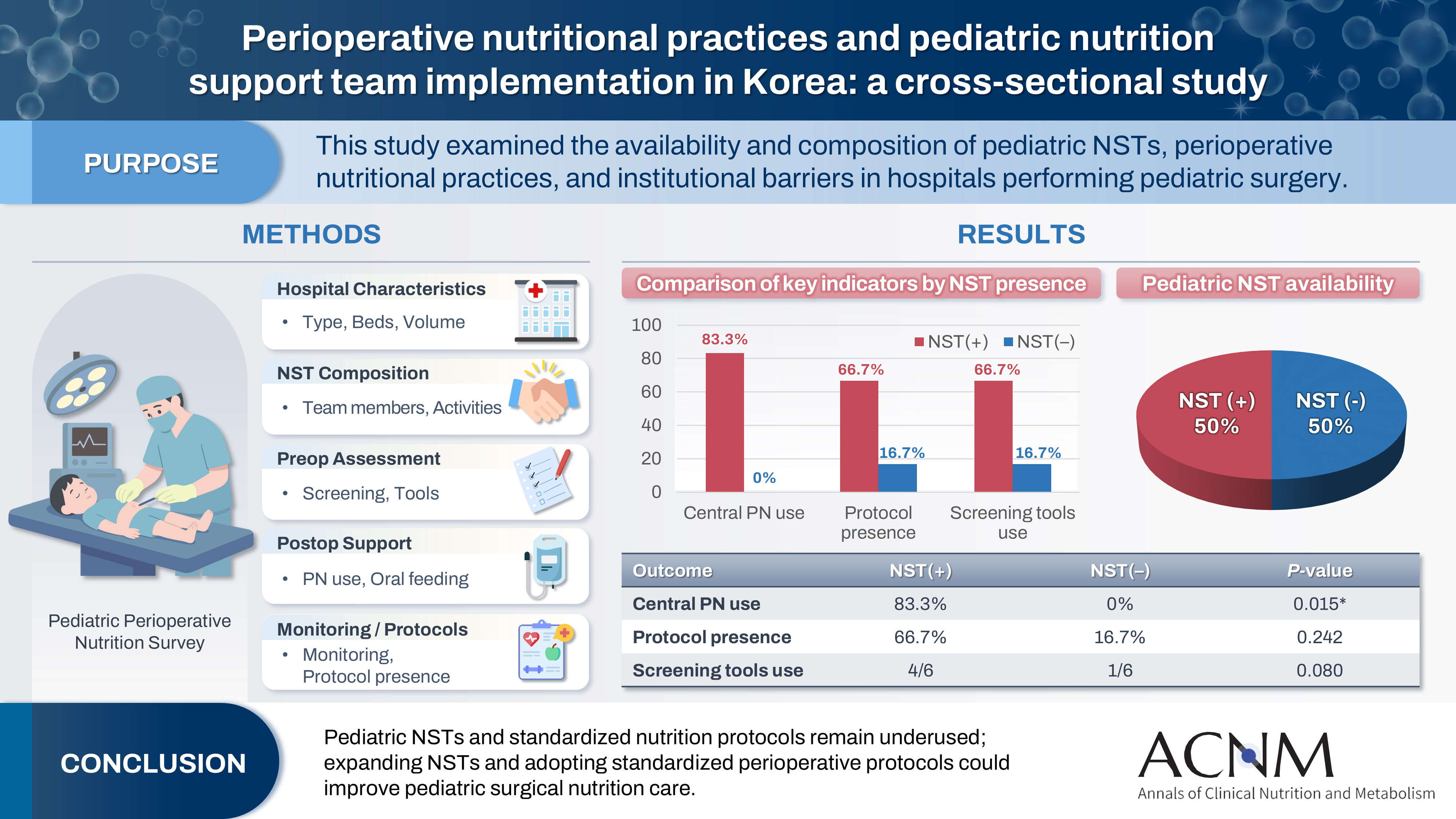
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 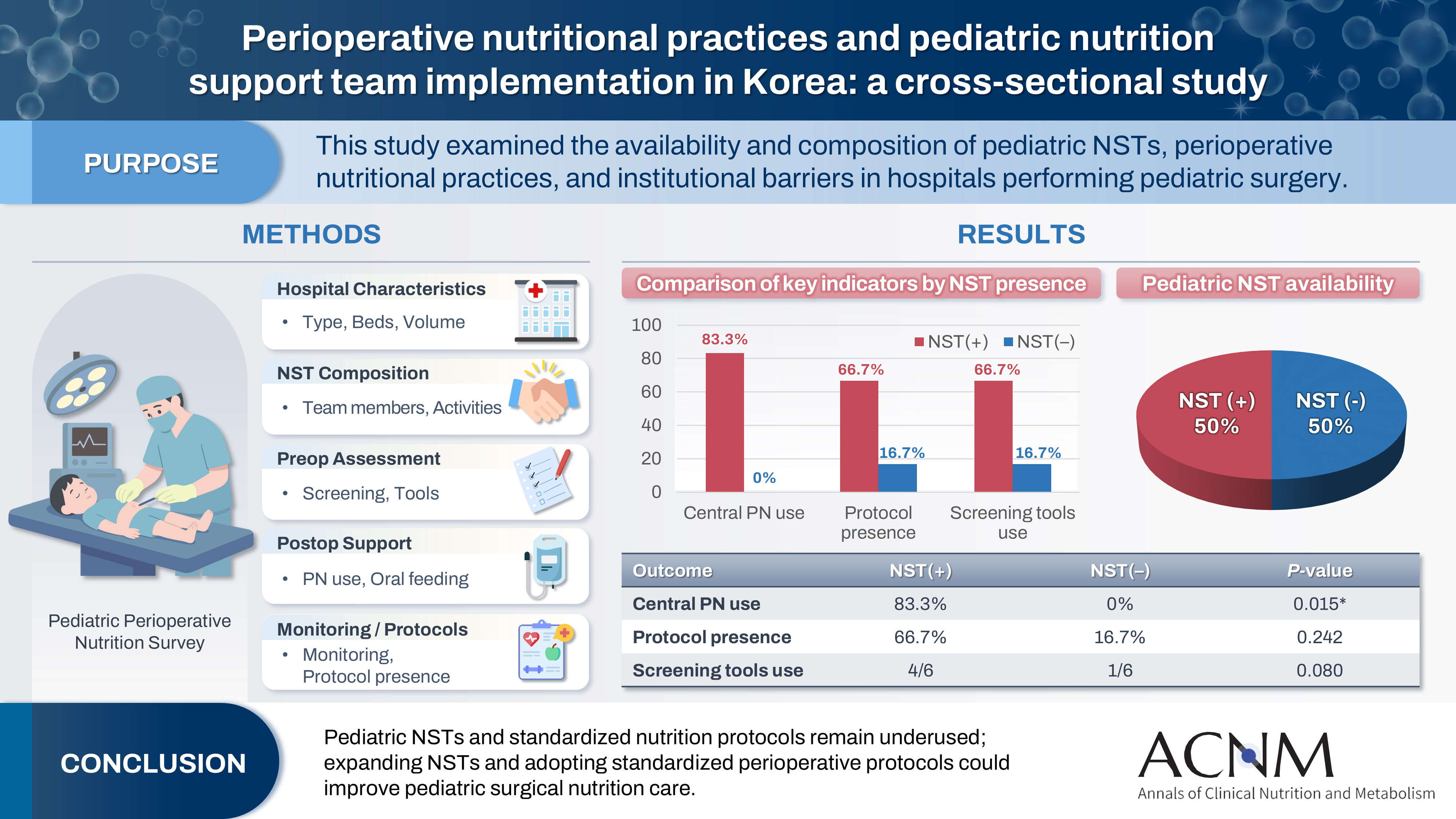
- Purpose
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 884 View
- 16 Download

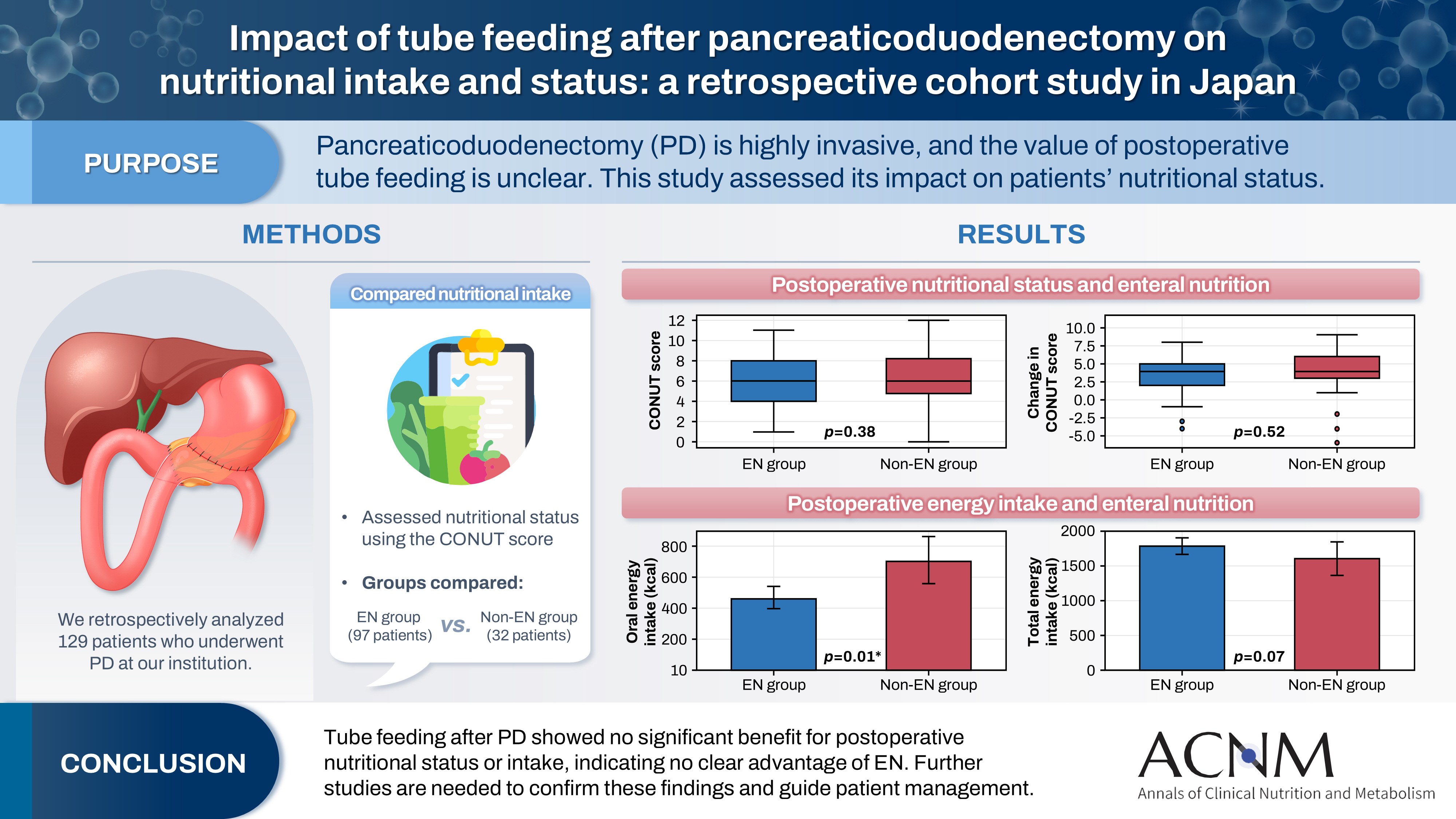
- Impact of tube feeding after pancreaticoduodenectomy on nutritional intake and status: a retrospective cohort study in Japan
- Masaharu Ishida, Masahiro Iseki, Shuichiro Hayashi, Aya Noguchi, Hideaki Sato, Shingo Yoshimachi, Akiko Kusaka, Mitsuhiro Shimura, Shuichi Aoki, Daisuke Douchi, Takayuki Miura, Shimpei Maeda, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(3):203-209. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0020
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 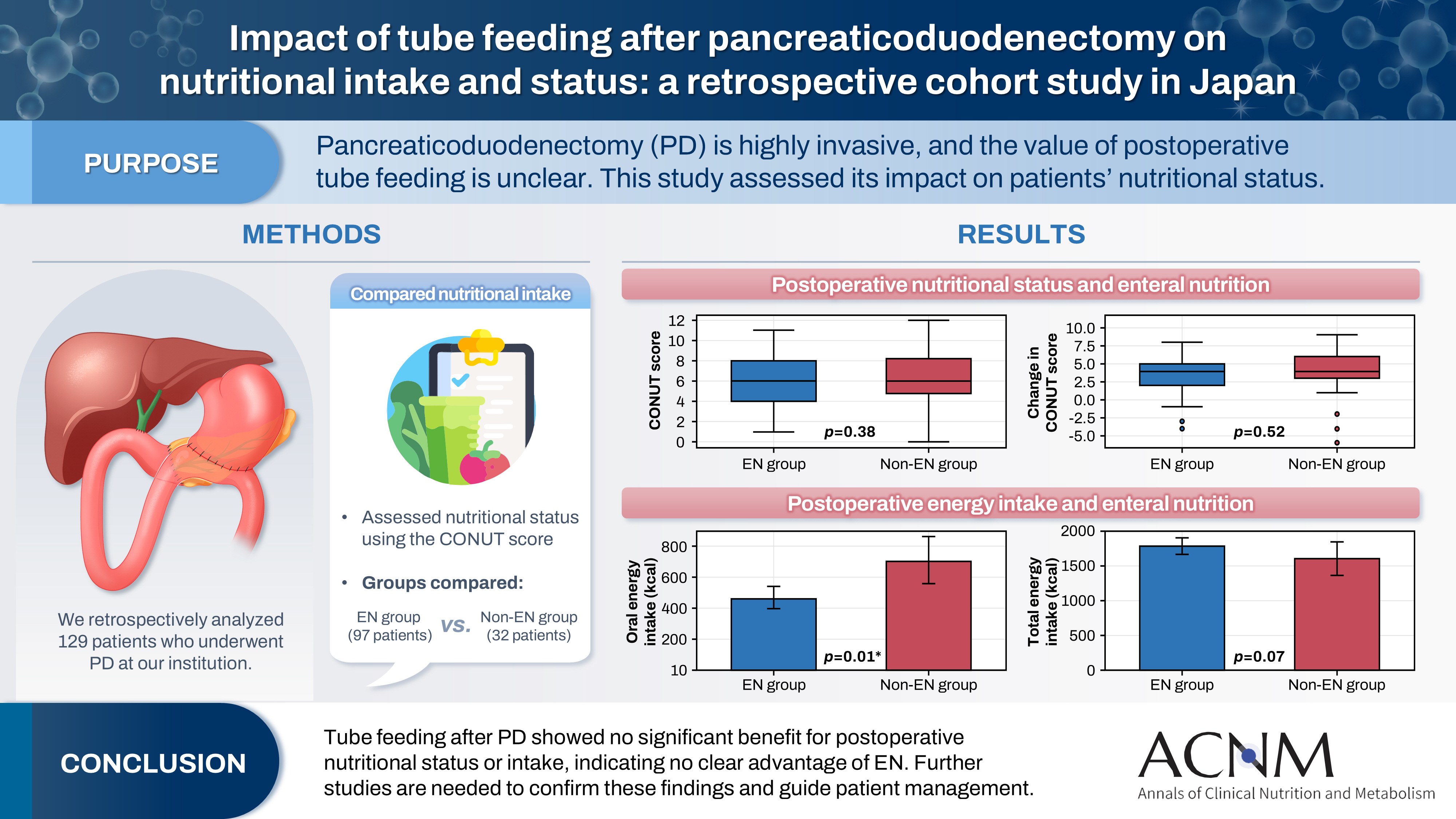
- Purpose
Pancreaticoduodenectomy (PD) is one of the most invasive procedures in gastrointestinal surgery. However, the clinical significance of postoperative tube feeding remains unclear. This study investigated the impact of enteral nutrition (EN) on the postoperative nutritional status of patients undergoing PD.
Methods
We retrospectively analyzed 129 patients who underwent PD at Tohoku University Hospital. Nutritional intake and status, evaluated using the Controlling Nutritional Status score, were compared between two groups: an EN group (97 patients) and a non-EN group (32 patients).
Results
There were no significant differences between the two groups in age, sex, body mass index, underlying diseases, operative duration, blood loss, postoperative pancreatic fistula, postoperative complications, delayed gastric emptying, or length of hospital stay. Although the EN group showed improvements in nutritional status both at discharge and compared with preoperative values, none of these changes reached statistical significance. Oral caloric intake was significantly higher in the non-EN group (P=0.01). In contrast, total energy intake was higher in the EN group, but this difference did not reach statistical significance (P=0.07).
Conclusion
Tube feeding after PD did not significantly influence postoperative nutritional status or overall nutritional intake. These findings suggest that EN offers no clear advantage over other approaches; however, further research is warranted to validate these results, refine existing guidelines, and optimize postoperative patient management.
- 401 View
- 9 Download

- Current practices and challenges in nutrition support team activities, 2025 in Korea: a multicenter cross-sectional descriptive study
- So Hyun Nam
- Ann Clin Nutr Metab 2025;17(2):97-103. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0026
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
This study aimed to evaluate the current practices, activities, and challenges of nutrition support teams (NSTs) in Korea. The assessment was conducted as part of the 4th NST Leadership Program of the Korean Society of Surgical Metabolism and Nutrition held in 2025, which seeks to foster leadership and enhance team functionality.
Methods
A nationwide survey was conducted in February 2025 among 54 NST members from 44 institutions. The survey explored team composition, consultation volume, educational programs, barriers to implementation, institutional support, and reimbursement challenges.
Results
Of the 44 participating hospitals, most (86.4%) operated a single NST, with multidisciplinary physician involvement from over three specialties in 77.2% of cases. Inpatient referrals to NSTs were generally low, with less than 10% at 63% of institutions. Only 40.9% had an individual office, and formal incentive systems were reported in 18.1% of hospitals. Educational programs for in-hospital staff were limited (29.5%), and less than half conducted regular academic meetings. Rates of adoption of NST recommendations varied widely, with barriers including a lack of engagement from attending physicians, failure to review the recommendations, and department-specific clinical policies. Efforts to promote NST activation included computerized prescription systems, automated referral workflows, staff education, and quality improvement initiatives. Participants focused on sharing effective NST cases, building incentives, exchanging clinical insights, clarifying team roles and leadership, and developing unified practice guidelines.
Conclusion
NSTs in Korea are well established but face ongoing challenges in collaboration and sustainability. Continued leadership and policy support are crucial for enhancing team performance and improving patient outcomes. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 5,353 View
- 80 Download
- 1 Crossref

Review
- Postoperative gut dysbiosis and its clinical implications, with an emphasis on probiotic strategies in gastric cancer patients undergoing gastrectomy: a narrative review
- Cheong Ah Oh
- Ann Clin Nutr Metab 2025;17(2):114-124. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0023
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review explores alterations in gut microbiota following gastrointestinal surgery, with a focus on gastrectomy for gastric cancer, and evaluates the therapeutic potential of probiotics in restoring microbial balance and reducing postoperative complications, including infections, inflammation, immune dysfunction, and cancer recurrence.
Current concept
Gastrointestinal surgery disrupts gut microbial homeostasis via surgical stress, oxygen exposure, altered bile flow, and perioperative antibiotic use. Gastrectomy, in particular, induces marked changes in the microbiota, including increased oral-origin and aerotolerant bacteria, decreased short-chain fatty acid–producing species, and elevated bile acid-transforming organisms. These alterations contribute to complications such as small intestinal bacterial overgrowth, surgical site infections, postoperative ileus, nutrient malabsorption, and potentially a higher risk of colorectal cancer. Probiotics—especially strains of Lactobacillus, Bifidobacterium, and Clostridium—have demonstrated beneficial effects by modulating the gut ecosystem, enhancing epithelial barrier integrity, and regulating immune and metabolic pathways. Randomized clinical trials support using probiotics in improving gastrointestinal recovery, reducing systemic inflammation, restoring microbial diversity, and shortening hospital stays after gastrectomy. Multi-strain probiotic formulations, particularly when administered perioperatively, show the greatest promise. However, safety concerns remain, especially for immunocompromised or critically ill patients, underscoring the need for rigorous clinical oversight and adherence to regulatory standards such as the European Food Safety Authority’s Qualified Presumption of Safety guidelines.
Conclusion
Postoperative dysbiosis is a modifiable factor in adverse surgical outcomes. Probiotic supplementation offers promising therapeutic potential in patients undergoing gastrectomy, though optimal strains, dosing, and timing remain to be determined. Tailored, evidence-based strategies may ultimately enhance both recovery and long-term outcomes after gastric cancer surgery.
- 8,567 View
- 56 Download

Original Article
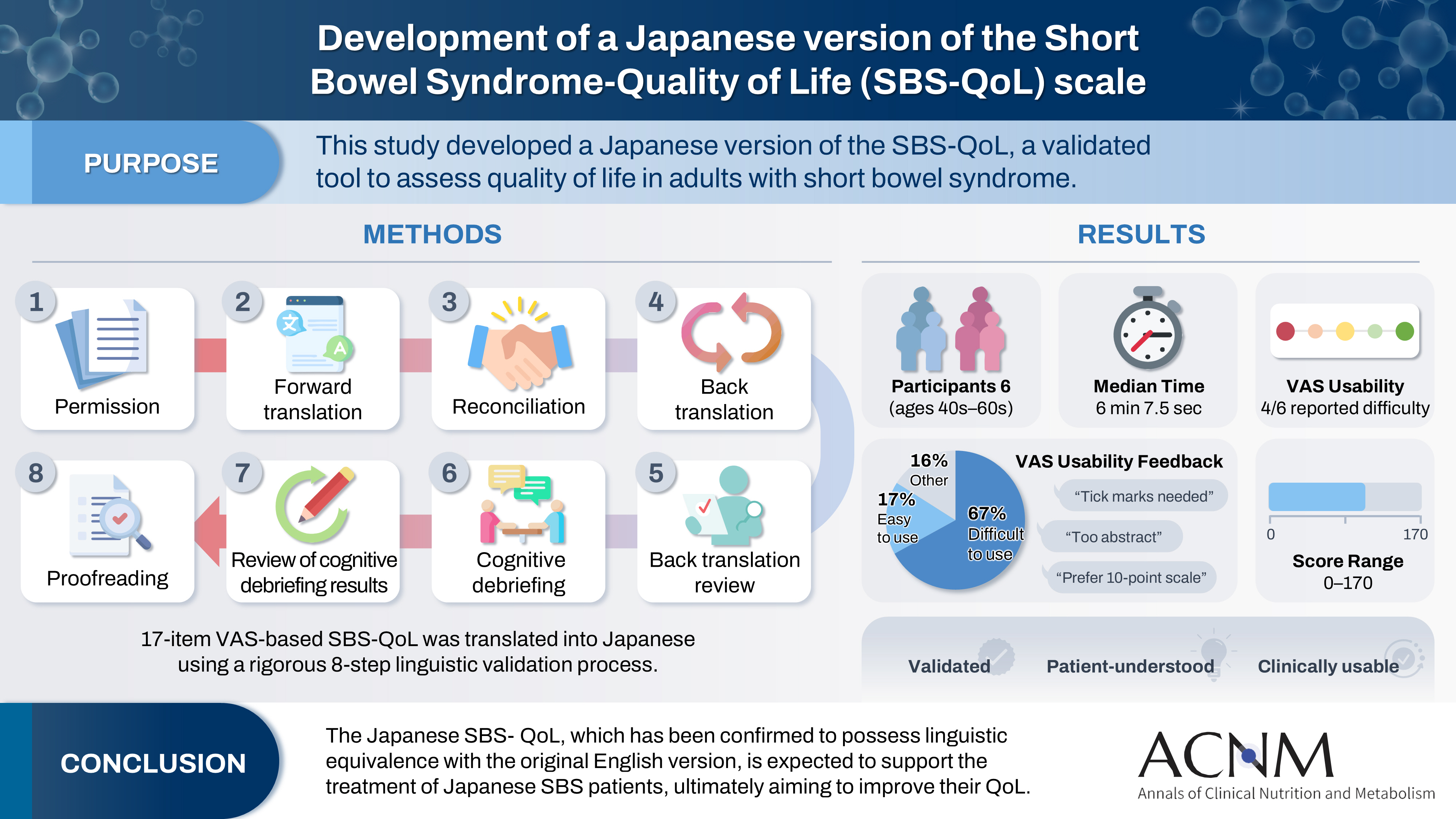
- Development of a Japanese version of the Short Bowel Syndrome-Quality of Life (SBS-QoL) scale
- Yuko Tazuke, Mayu Suzuki, Sae Kikuchi, Kaori Ishiguro, Hiroomi Okuyama
- Ann Clin Nutr Metab 2025;17(2):132-138. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 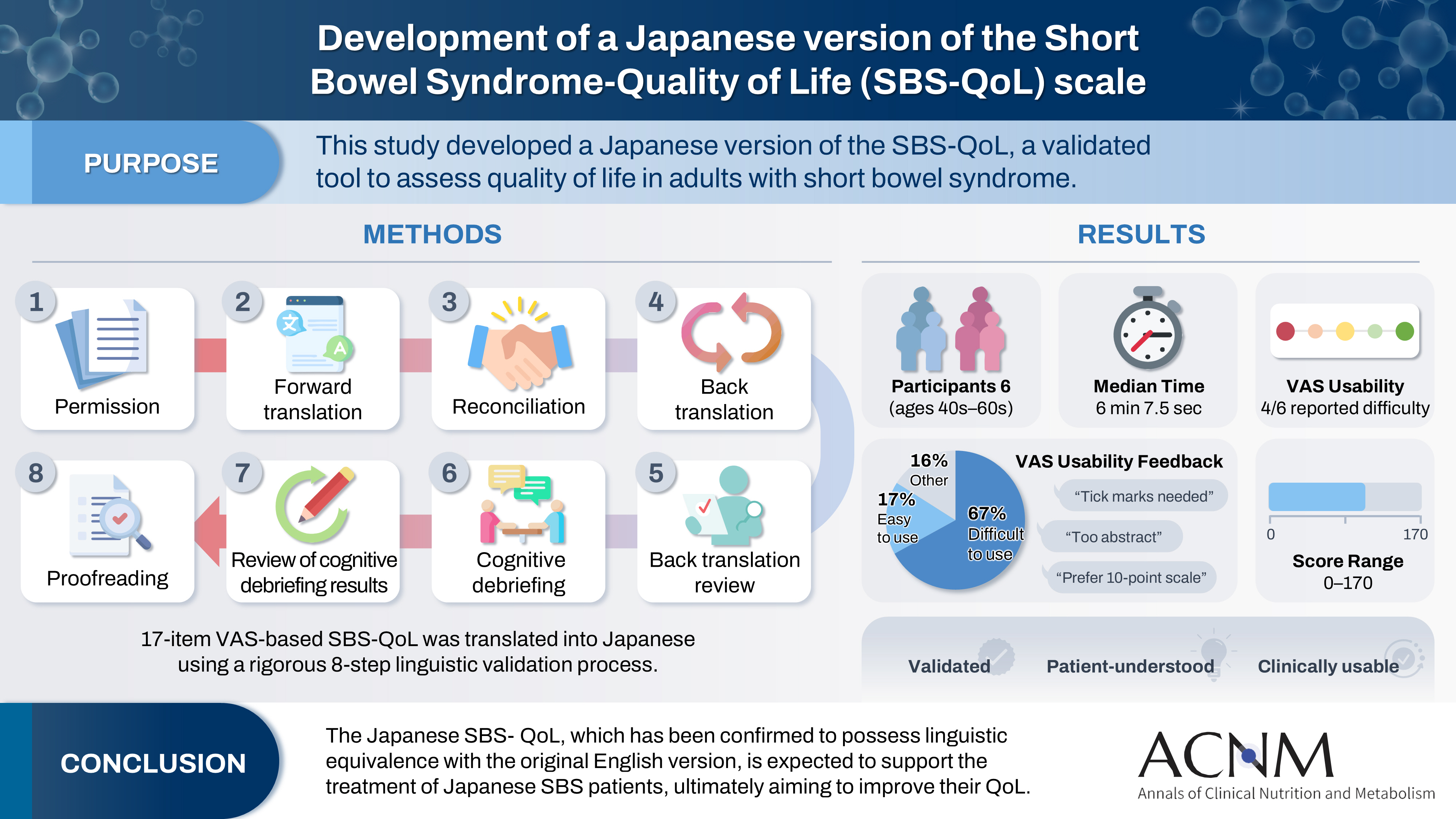
- Purpose
The Short Bowel Syndrome‐Quality of Life (SBS‐QoL) scale is a reliable and sensitive instrument developed to measure and evaluate the quality of life (QoL) in adult patients with short bowel syndrome (SBS). In Japan, increasing attention has been given to the assessment of QoL in patients with SBS; however, no Japanese‐language SBS‐specific scale is currently available. This study aimed to develop a Japanese version of the SBS‐QoL based on the original English version.
Methods
A provisional Japanese version was created in accordance with the guidelines of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force, utilizing a process of forward translation, adjustment, and back translation.
Results
Cognitive debriefing using the provisional Japanese version was conducted with six Japanese patients with SBS. Based on these results, the Japanese wording was evaluated and revised, leading to the creation of the final Japanese version.
Conclusion
The Japanese SBS‐QoL, which has been confirmed to possess linguistic equivalence with the original English version, is expected to support the treatment of Japanese SBS patients, ultimately aiming to improve their QoL.
- 1,643 View
- 19 Download

Review
- Improving the usability of lipid emulsions and optimizing their user-friendliness: a narrative review
- Keisuke Kubota, Natsuko Ichikawa, Kazuhiro Isoda, Misato Enomoto, Miyoko Kosugi, Mari Tanabe, Naoya Sakuraba, Sayuri Endo, Atsushi Suzuki, Masanori Hashimoto
- Ann Clin Nutr Metab 2025;17(2):104-113. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0015
-
 Abstract
Abstract
 PDF
PDF - Purpose
Reluctance to administer lipid emulsions to patients receiving treatment, or as recommended by a nutritional support team, often stems from various restrictions or concerns about potential adverse effects. This paper aims to discuss the appropriate clinical use of lipid emulsions to enhance both patient safety and convenience.
Current concept
We conducted a literature review to assess the importance of nutritional therapy and nutritional intervention, the advantages and disadvantages of lipid-emulsion administration, the current situation in Japan, and differences between lipid formulations. Here, we address issues regarding lipid-emulsion use, including: administration rate, drug mixing, administration in critically ill patients, and early postoperative use. Our findings suggest the following solutions to each issue: although a rate below 0.1 g/kg/hr is generally recommended, faster administration is possible if needed, depending on the case; administration via a piggy tube to basic infusion formulations is unproblematic; second- and third-generation fat emulsions are safe for critically ill patients, though soybean oil should be used with caution; and while fat emulsion administration is feasible immediately after surgery, due to endogenous energy mobilization, it is preferable to initiate administration from the third to fourth postoperative day.
Conclusion
The provisional conclusions of this study are as follows: the introduction of medium-chain triglyceride formulations and fish oil (second- and third-generation lipid emulsions), which are not yet available in Japan, is urgently needed; and individualized administration is essential due to substantial interindividual variability in lipid emulsion usage.
- 4,289 View
- 30 Download

Original Articles
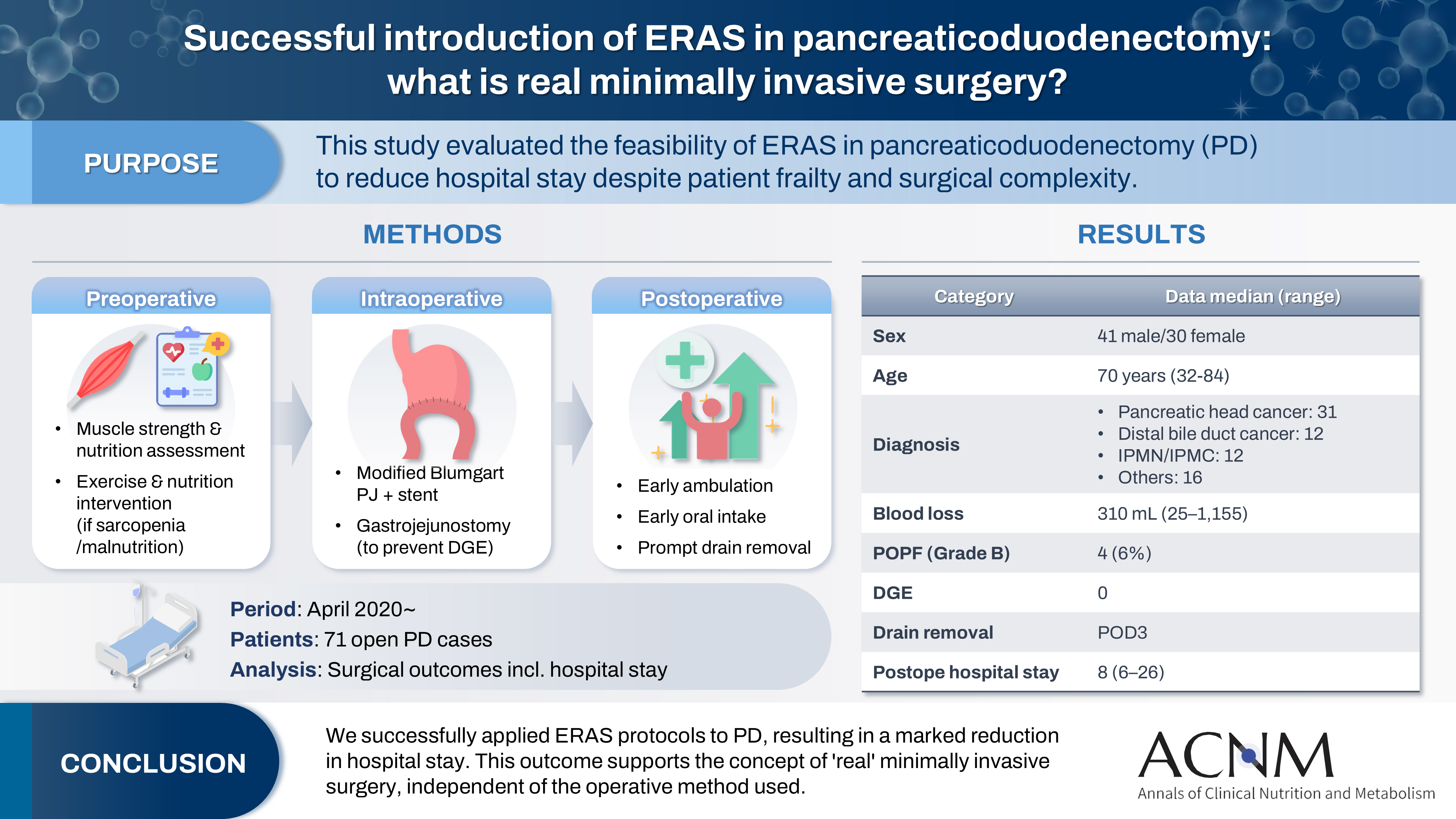
- Successful introduction of ERAS in pancreaticoduodenectomy: what is real minimally invasive surgery?
- Toshimi Kaido, Yosuke Miyachi, Koichiro Mitsuoka, Mariko Sambommatsu
- Ann Clin Nutr Metab 2025;17(2):156-161. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0014
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 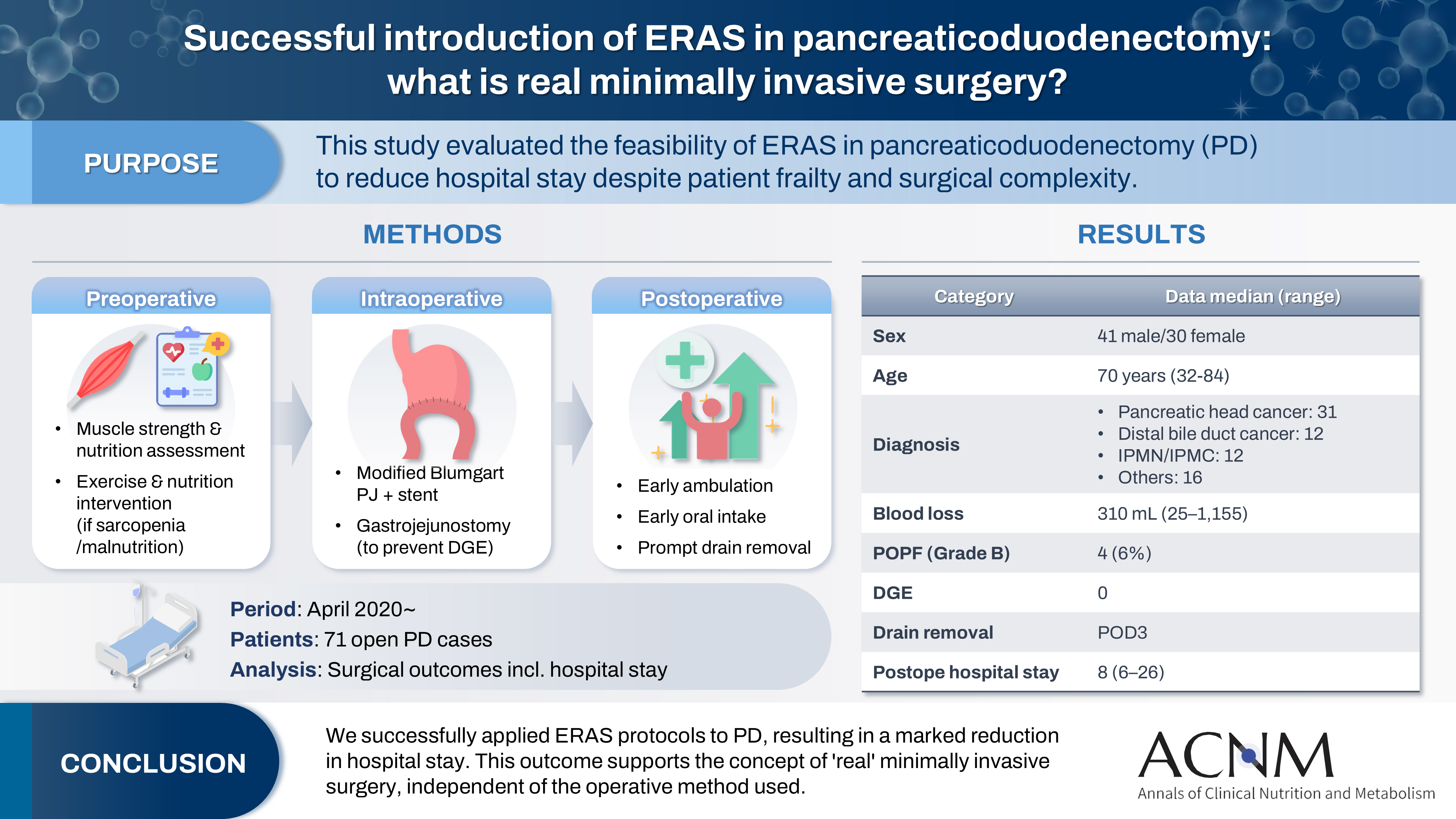
- Purpose
The introduction of Enhanced Recovery After Surgery (ERAS) protocols for pancreaticoduodenectomy (PD) has been considered challenging due to factors such as preexisting malnutrition, sarcopenia, the complexity of the surgery, and the high incidence of postoperative complications, including postoperative pancreatic fistula (POPF) and delayed gastric emptying (DGE). This study aimed to determine whether ERAS could be implemented in PD to achieve shorter postoperative hospital stays.
Methods
Our novel approach consists of three components. Preoperatively, we routinely assess patients' muscle strength and nutritional status and initiate exercise and nutritional interventions for those identified with sarcopenia or malnutrition. Intraoperatively, we perform pancreaticojejunostomy using a modified Blumgart’s technique with our stent placement policy and utilize new gastrojejunostomy methods to prevent DGE. Principles of postoperative management are early ambulation, early oral intake, and early drain removal. Since April 2020, we have employed this strategy and retrospectively evaluated its effectiveness. We enrolled 71 consecutive patients who underwent open PD with curative intent. Various surgical outcomes, including postoperative hospital stay, were analyzed.
Results
There were 41 men and 30 women, with a median age of 70 years. Preoperative diagnoses included pancreatic head cancer in 31, distal bile duct cancer in 12, and others. Median intraoperative blood loss was 310 mL. Grade B POPF occurred in four patients (6%). No cases of DGE were observed. The median postoperative hospital stay was 8 days (range, 6–26 days).
Conclusion
We successfully implemented ERAS protocols in PD and achieved a significantly reduced postoperative hospital stay. We propose that this approach is “real minimally invasive surgery," regardless of the surgical technique used.
- 3,778 View
- 18 Download

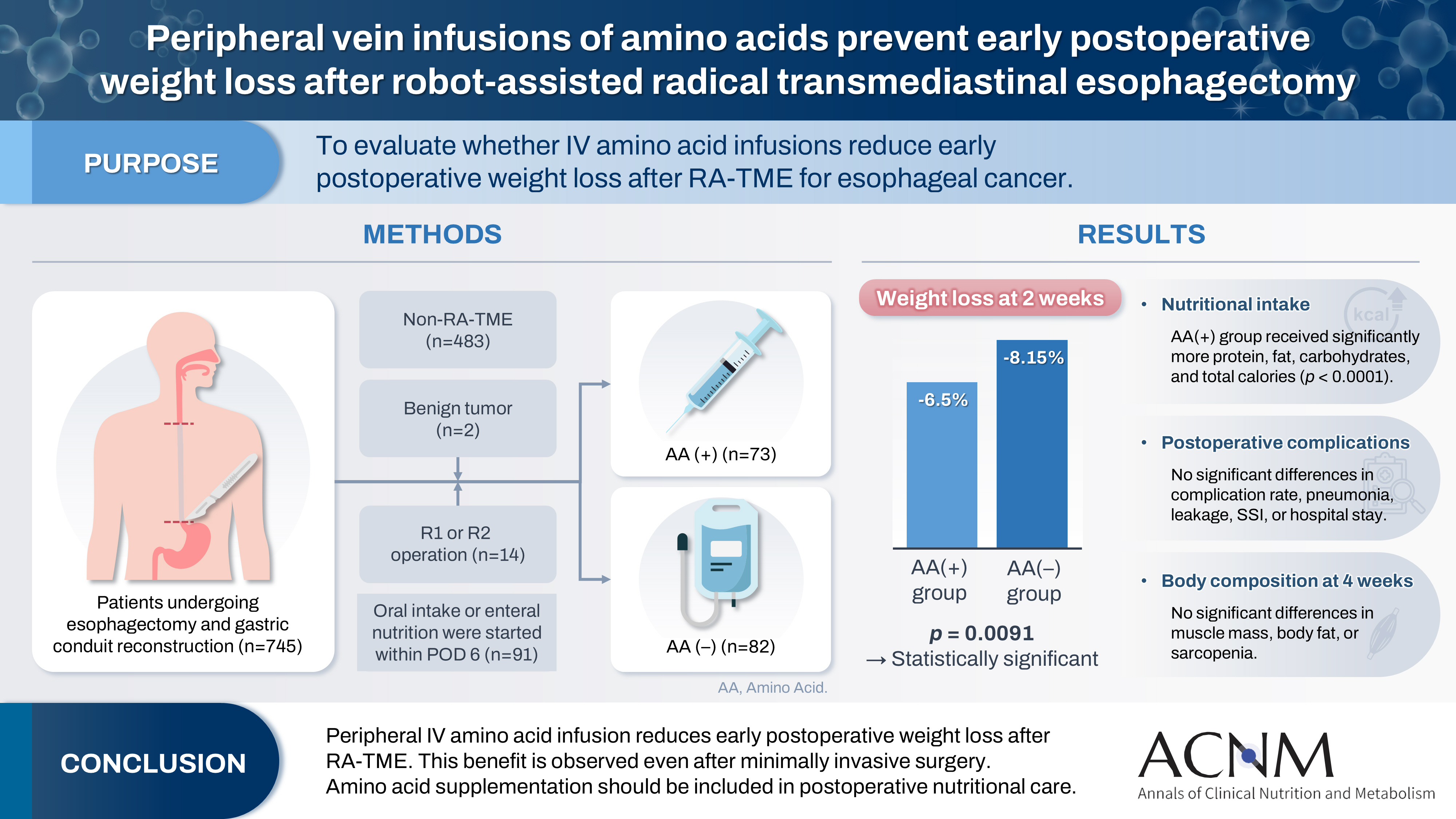
- Peripheral vein infusions of amino acids prevent early postoperative weight loss after robot-assisted radical transmediastinal esophagectomy: a retrospective study in Japan
- Tomonori Narita, Kazuhiko Fukatsu, Satoshi Murakoshi, Reo Inoue, Kenichi Kono, Midori Noguchi, Nana Matsumoto, Shoh Yajima, Koichi Yagi, Yoshifumi Baba
- Ann Clin Nutr Metab 2025;17(2):149-155. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0012
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 
- Purpose
Postoperative body weight loss (PBWL) is linked to poor long-term outcomes following esophagectomy for esophageal cancer, making perioperative nutrition critically important. Although minimally invasive procedures such as robot-assisted radical transmediastinal esophagectomy (RA-TME) have become more prevalent, less attention has been paid to perioperative nutritional management. This study evaluates the impact of intravenous (IV) amino acid infusions on PBWL in patients undergoing RA-TME.
Methods
We retrospectively analyzed 155 patients who underwent RA-TME for esophageal or esophagogastric junction cancer at our hospital between 2011 and 2022. Patients were divided into two groups: AA(+) (n=73, received IV amino acids between postoperative days 1–6) and AA(–) (n=82, did not receive IV amino acids). Oral or enteral nutrition was withheld until postoperative day 6. We compared nutrient intake, postoperative outcomes, and nutritional status between groups.
Results
Patient backgrounds, surgical outcomes, and complication rates were similar in both groups. However, the AA(+) group received significantly greater energy and nutrient intake. PBWL at 2 weeks post-surgery was significantly lower in the AA(+) group than in the AA(–) group (6.50% vs. 8.15%, P=0.0091).
Conclusion
IV amino acid infusion may help mitigate early PBWL after RA-TME.
- 1,195 View
- 17 Download

- Insulinotropic action of L-carnitine and branched-chain amino acids following energy intake in healthy, young Japanese women: a non-randomized controlled trial
- Yoichi Sakurai, Hideyuki Namba, Satoshi Odo
- Ann Clin Nutr Metab 2025;17(2):139-148. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0011
-
 Abstract
Abstract
 PDF
PDF - Purpose
The present study uses healthy human volunteers to examine the insulinotropic action of L-carnitine and branched-chain amino acids (BCAAs) after energy intake.
Methods
A total of 39 young, healthy human volunteers were assigned to receive oral doses of either L-carnitine alone (L group, n=10) or L-carnitine combined with a single or long-term continuous dose of BCAAs. Controls (C group, n=16) received none of these. L-carnitine was administered orally at 1,000 mg/d for 14 days, and BCAA was administered orally either once just before exercise (L+SB group, n=6), or every day for 14 days (L+CB group, n=7) until 2 days before the experiment. After overnight fasting, 200 kcal of glucose and oral nutritional supplement were administered to prevent hypoglycemia. Blood glucose, free-fatty acid, and serum insulin levels were measured to examine the insulinotropic action before and after exercise.
Results
Blood glucose and serum insulin levels in the L group were significantly lower than those in the C group. While the serum insulin levels were higher after energy administration than those in the fasting state in all groups, these were significantly higher in the L+SB group and in the L+CB group compared with those in the L group. The insulinotropic action after energy intake remained even after the repeated administration of BCAA discontinued 2 days before the experi¬ment and even after serum BCAA levels remained the same.
Conclusion
While the insulinotropic action appeared after a single dose of BCAA, it was also potentiated by long-term repeated oral administration of BCAA.
- 941 View
- 13 Download

- Evaluation of the modified Nutrition Risk in Critically Ill score in Korean critically ill patients with COVID-19: a retrospective cohort study
- Won Ho Han, Jong-Mog Lee, Jae Hoon Lee, Hyun Mi Lee, Ji-Yeon Kim, Mok Young Jang, Sung-Sik Han
- Ann Clin Nutr Metab 2025;17(2):125-131. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0009
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
We evaluated the efficacy of the modified Nutrition Risk in Critically Ill (mNUTRIC) score for malnutrition screening and its association with mortality in intensive care unit (ICU) patients with COVID-19.
Methods
The nutritional status of 129 COVID-19 ICU patients admitted between February 2021 and May 2022 was assessed using American Society for Parenteral and Enteral Nutrition/Academy of Nutrition and Dietetics (ASPEN/AND) criteria. The sensitivity, specificity, and clinical correlations of the mNUTRIC score were analyzed.
Results
Of the 129 patients, 35 (27.1%) met the ASPEN/AND malnutrition criteria. Multivariable analysis identified the mNUTRIC score, underlying malignancy, and mechanical ventilation as significant factors associated with malnutrition. The mNUTRIC score had a sensitivity of 77.1% and specificity of 63.8% (area under the curve [AUC], 0.71; 95% confidence interval [CI], 0.62–0.79) for diagnosing malnutrition, improving to 88.6% and 80.9%, respectively, after adjusting for malignancy and ventilation (AUC, 0.89; 95% CI, 0.82–0.95). Patients with a low mNUTRIC score had a mortality rate of 2.9% and a median ICU stay of 7.7 days (range, 0–84.2 days), whereas those with a high score (≥5) had a mortality rate of 13.1% and a median ICU stay of 10.2 days (range, 1.4–88.5 days) (P=0.046 and P=0.011, respectively).
Conclusion
The mNUTRIC score is an effective screening tool for malnutrition in ICU patients with COVID-19, especially those with malignancy or requiring mechanical ventilation, and is strongly associated with mortality and length of ICU stay.
- 2,781 View
- 30 Download

- Perioperative outcomes of older adult patients with pancreatic cancer based on nutritional status: a retrospective cohort study
- Takanori Morikawa, Masaharu Ishida, Masamichi Mizuma, Kei Nakagawa, Takashi Kamei, Michiaki Unno
- Ann Clin Nutr Metab 2025;17(1):66-74. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.001
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study investigated the effects of preoperative nutritional status on postoperative outcomes in older adult patients with pancreatic adenocarcinoma.
Methods
The background and perioperative factors of patients who underwent pancreatectomy for pancreatic adenocarcinoma between 2007 and 2020 were retrospectively analyzed.
Results
Patients aged 75 years or over (older adults) were significantly associated with hypertension, upfront surgery, and lower prognostic nutritional index. In addition, these patients had a significantly lower rate of portal vein resection, less blood loss, and shorter operation time than patients aged less than 75 years (non-older adults). During the postoperative course, older adult patients had a higher rate of pneumonia and lower overall survival than younger patients, although recurrence‐free survival was comparable. In addition, older adult patients showed preoperative malnutrition as a risk factor for postoperative in‐hospital death.
Conclusion
Surgical treatment for pancreatic cancer in older adult patients was performed safely. However, preoperative malnutrition is a risk factor for in‐hospital death and such patients require nutritional support and less‐invasive surgery. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,833 View
- 23 Download
- 1 Crossref

Review
- Pathogenesis, risk factors, and management of postoperative delayed gastric emptying after distal gastrectomy: a narrative review
- Cheong Ah Oh
- Ann Clin Nutr Metab 2025;17(1):9-17. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0007
-
 Abstract
Abstract
 PDF
PDF - Purpose
This narrative review elucidates the complex pathogenesis, key risk factors, and effective management strategies for postoperative delayed gastric emptying (DGE) following distal gastrectomy with D2 lymphadenectomy, a definitive procedure for middle and lower gastric cancer. It also explores opportunities for improved prevention and innovative treatment options.
Current concept
DGE significantly disrupts gastric motility and presents with symptoms such as early satiety, postprandial fullness, nausea, vomiting, and gastric atony. Although rarely fatal, DGE hampers oral intake, prolongs hospital stays, and diminishes quality of life. Current evidence indicates that DGE is a multifactorial disorder resulting from an interplay of vagal nerve disruption, damage to smooth muscle and interstitial cells of Cajal, imbalances in gastrointestinal hormones, and postoperative gut microbiome dysbiosis. Patient-specific factors, including advanced age, poor nutritional status, diabetes, and preoperative pyloric obstruction, along with surgical factors (most notably Billroth II reconstruction), further increase the risk of DGE. Management involves dietary modifications, prokinetic agents (such as metoclopramide and selective 5-HT4 agonists like prucalopride), and gastric decompression.
Conclusion
DGE is a challenging complication following gastrectomy that demands a deeper understanding of its underlying mechanisms to improve patient outcomes. Emerging therapies, including microbiota modulation and advanced pharmacological agents, offer promising new treatment avenues.
- 10,074 View
- 112 Download

Original Article
- Effects of enteral nutrition formulas with varying carbohydrate amounts on glycemic control in diabetic mice
- Yukari Miki, Kazuo Hino
- Ann Clin Nutr Metab 2025;17(1):85-93. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0006
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study evaluated the effects of an 8‑week liquid diets with different carbohydrate contents–64% energy in HINE E‑Gel (ST) and 50% energy in HINE E‑Gel LC (LC)–on glycemic control and nutritional status in a mouse model of type 2 diabetes mellitus (db/db mice). The objective was to determine whether reducing carbohydrate intake within the Dietary Reference Intakes for Japanese people improves glycemic control indices, addressing the evidence gap in regarding the long‑term safety and efficacy of low‑carbohydrate enteral nutrition in patients with diabetes.
Methods
db/db mice (n=10 per group) and non‑diabetic db/m mice (n=4) as controls were fed ST, LC, or AIN‑93G diets ad libitum for 8 weeks. The diets primarily differed in carbohydrate content (64% in ST vs. 50% in LC). Blood glucose and glycated hemoglobin (HbA1c), plasma glucose and glycoalbumin, organ weights, and renal function markers were measured weekly or at 4 and 8 weeks. Histopathological examinations of the liver and kidneys were performed at 8 weeks.
Results
At 8 weeks, the LC group showed significantly lower plasma glucose (P=0.0051) and glycoalbumin (P=0.0013) levels compared to the ST group, with a trend toward lower HbA1c (P=0.0514). Although body weight was significantly higher in the LC group (P=0.0038), there were no significant differences between the ST and LC groups in caloric intake, renal function, or histopathological findings.
Conclusion
Reducing carbohydrate intake to 50% of total energy within dietary guidelines may improve glycemic control in diabetic mice, suggesting the need for further long‑term evaluation for clinical applications. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,748 View
- 29 Download
- 1 Crossref

Review
- Perioperative nutritional management to improve long-term outcomes in critically ill perioperative organ transplant patients: a narrative review
- Toshimi Kaido
- Ann Clin Nutr Metab 2025;17(1):18-24. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0005
-
 Abstract
Abstract
 PDF
PDF - Purpose
This review examines the significance of perioperative nutritional management in organ transplantation, with a particular focus on liver transplantation. Organ transplant recipients often experience malnutrition and sarcopenia due to nutritional and metabolic abnormalities associated with organ dysfunction. Because transplantation is a highly invasive procedure, optimizing perioperative nutritional care is critical for improving short-term outcomes and reducing postoperative infection-related mortality.
Current concept
Recent clinical investigations have shown that liver transplant recipients, who are frequently afflicted with end-stage liver disease and uncompensated cirrhosis, are particularly vulnerable to protein-energy malnutrition and secondary sarcopenia. Our analysis identified low pre-transplant nutritional status and the absence of preoperative branched-chain amino acid supplementation as independent risk factors for post-transplant sepsis. In response, we developed a customized nutritional therapy protocol that incorporates precise body composition analysis, serial measurements of biochemical markers (including prealbumin, zinc, and the branched-chain amino acid/tyrosine ratio), and targeted supplementation with branched-chain amino acids, zinc acetate, and synbiotics. Early initiation of enteral nutrition coupled with postoperative rehabilitative interventions resulted in improved outcomes. In addition, stratified body composition parameters correlated with survival differences and informed revised transplantation criteria.
Conclusion
Tailored perioperative nutritional management and rehabilitative strategies are essential for improving early postoperative outcomes in liver transplantation. These findings underscore the need for proactive nutritional assessment and intervention, which may represent a breakthrough in transplant prognosis. Future research should refine nutritional protocols and integrate novel biomarkers, while education and interdisciplinary collaboration remain crucial for enhancing transplant outcomes and reducing complications. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 3,934 View
- 103 Download
- 1 Crossref

Original Articles
- Association between decreased dietary intake during hospitalization and long-term weight loss in postoperative gastric cancer patients over 75 years of age: a retrospective cohort study
- Daiki Tabe, Isao Miyajima, Akira Tsukada
- Ann Clin Nutr Metab 2025;17(1):75-84. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0004
-
 Abstract
Abstract
 PDF
PDF - Purpose
Weight loss following gastrectomy is a significant concern, and maintaining adequate nutrition is necessary, especially given the growing number of older adult patients. This study examined the relationship between postoperative food intake and long-term weight loss in postgastrectomy patients aged ≥75 years.
Methods
Out of 88 patients who underwent gastrectomy for gastric cancer at our institute, 46 were aged ≥75 years. These patients were divided into two groups: one with an average energy intake exceeding 50% of the basal metabolic rate and one with an intake below 50% of the basal metabolic rate. The percentage change in body weight up to 6 months post-surgery was compared between the groups.
Results
In the group with higher dietary intake, the rate of weight change at 3 and 6 months postoperatively was lower, and fewer patients received postoperative adjuvant chemotherapy.
Conclusion
Poor postoperative food intake may serve as a predictor of weight loss up to 3 months following surgery in postgastrectomy patients aged ≥75 years. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 1,080 View
- 26 Download
- 1 Crossref

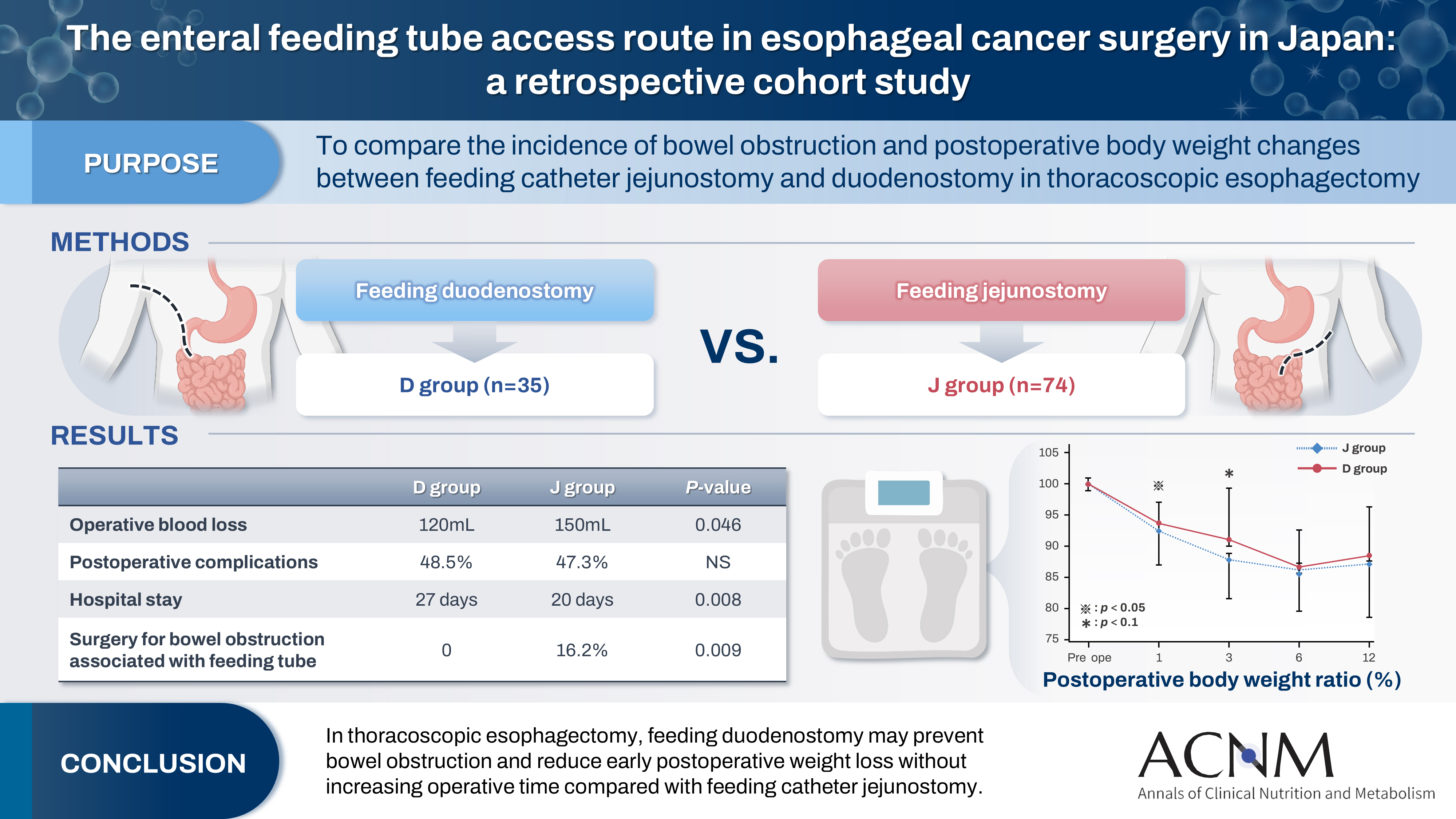
- The enteral feeding tube access route in esophageal cancer surgery in Japan: a retrospective cohort study
- Hiroyuki Kitagawa, Keiichiro Yokota, Tsutomu Namikawa, Kazuhiro Hanazaki
- Ann Clin Nutr Metab 2025;17(1):58-65. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0003
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 
- Purpose
Feeding catheter jejunostomy is a useful access route for early enteral nutrition during esophageal cancer surgery. However, it may lead to postoperative bowel obstruction associated with feeding jejunostomy (BOFJ). To prevent BOFJ, we introduced feeding catheter duodenostomy via the round ligament in 2018. This study aimed to compare the incidence of BOFJ and postoperative body weight changes between feeding catheter jejunostomy and duodenostomy.
Methods
A total of 109 patients who underwent thoracoscopic esophagectomy and gastric tube reconstruction for esophageal cancer at Kochi Medical School Hospital between March 2013 and November 2020 were included. Preoperative patient characteristics (age, sex, preoperative weight, body mass index, cancer stage, and preoperative treatment), surgical outcomes (operative time, blood loss, and postoperative complications [wound infection, pneumonia, anastomotic leakage, BOFJ]), and body weight changes at 1, 3, 6, and 12 months post-surgery were compared between the jejunostomy (J) and duodenostomy (D) groups.
Results
The D group consisted of 35 patients. No significant differences were observed between the groups regarding age, sex, weight, body mass index, cancer stage, operative time, postoperative complications, or duration of tube placement. However, the D group had a significantly lower rate of preoperative chemotherapy (45.7% vs. 78.4%, P=0.001) and lower operative blood loss (120 mL vs. 150 mL, P=0.046) than the J group. All 12 cases of BOFJ occurred in the J group. Furthermore, the D group experienced a significantly lower weight loss ratio at 1 month postoperatively (93.9% vs. 91.8%, P=0.039).
Conclusion
In thoracoscopic esophagectomy, feeding duodenostomy may prevent bowel obstruction and reduce early postoperative weight loss without increasing operative time compared with feeding catheter jejunostomy. -
Citations
Citations to this article as recorded by- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
Ye Rim Chang
Ann Clin Nutr Metab.2025; 17(2): 95. CrossRef
- Strengthening collaboration: introducing the contributions of Japanese Society for Surgical Metabolism and Nutrition to Annals of Clinical Nutrition and Metabolism
- 2,497 View
- 30 Download
- 1 Crossref

Guideline
- A practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition: Part I. prescribing enteral nutrition orders
- Ye Rim Chang, Bo-Eun Kim, In Seok Lee, Youn Soo Cho, Sung-Sik Han, Eunjung Kim, Hyunjung Kim, Jae Hak Kim, Jeong Wook Kim, Sung Shin Kim, Eunhee Kong, Ja Kyung Min, Chi-Min Park, Jeongyun Park, Seungwan Ryu, Kyung Won Seo, Jung Mi Song, Minji Seok, Eun-Mi Seol, Jinhee Yoon, Jeong Meen Seo, for KSPEN Enteral Nutrition Committee
- Ann Clin Nutr Metab 2025;17(1):3-8. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0002
-
 Abstract
Abstract
 PDF
PDF - Purpose
This study aimed to develop a comprehensive practical guide for enteral nutrition (EN) designed to enhance patient safety and reduce complications in Korea. Under the leadership of the Korean Society for Parenteral and Enteral Nutrition (KSPEN), the initiative sought to standardize EN procedures, improve decision-making, and promote effective multidisciplinary communication.
Methods
The KSPEN EN committee identified key questions related to EN practices and organized them into seven sections such as prescribing, delivery route selection, formula preparation, administration, and quality management. Twenty-one experts, selected based on their expertise, conducted a thorough literature review to formulate evidence-based recommendations. Drafts underwent peer review both within and across disciplines, with final revisions completed by the KSPEN Guideline Committee. The guide, which will be published in three installments, addresses critical elements of EN therapy and safety protocols.
Results
The practical guide recommends that EN orders include detailed elements and advocates the use of electronic medical records for communication. Standardized prescription forms and supplementary safety measures are outlined. Review frequency is adjusted according to patient condition—daily for critically ill or unstable patients and as dictated by institutional protocols for stable patients. Evidence indicates that adherence to these protocols reduces mortality, complications, and prescription errors.
Conclusion
The KSPEN practical guide offers a robust framework for the safe delivery of EN tailored to Korea’s healthcare context. It emphasizes standardized protocols and interdisciplinary collaboration to improve nutritional outcomes, patient safety, and operational efficiency. Rigorous implementation and monitoring of adherence are critical for its success. -
Citations
Citations to this article as recorded by- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
Suk-Kyung Hong
Ann Clin Nutr Metab.2025; 17(1): 1. CrossRef
- Bridging evidence and clinical practice: a practical guide for enteral nutrition from the Korean Society for Parenteral and Enteral Nutrition
- 6,883 View
- 183 Download
- 1 Crossref

Original Articles
- Development of a pre- and re-habilitation protocol for gastrointestinal cancer surgery
- Eun Young Kim, Jung Hoon Bae, Jiseon Kim, Eun Joo Yang, Sang-Jae Park, In Kyu Lee, on behalf of the Task Force Team for Development and Trial Application of Pre/Rehabilitation Protocol in GI Cancer Surgery
- Ann Clin Nutr Metab 2025;17(1):25-40. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0001
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose
Surgical resection is the primary curative treatment for gastrointestinal (GI) cancer; however, it is associated with high postoperative complication rates and impaired recovery. Frailty, malnutrition, and sarcopenia increase morbidity and mortality, underscoring the need for perioperative rehabilitation programs. Standardized rehabilitation protocols during the perioperative period are currently lacking in Korea. We aimed to develop an evidence-based rehabilitation protocol for GI cancer patients to enhance postoperative outcomes and facilitate clinical implementation.
Methods
A multidisciplinary task force team comprising experts in surgery, clinical nutrition, and rehabilitation medicine conducted a systematic literature search and comprehensive review from 2012 to 2022 to develop a standardized pre- and re-habilitation protocol for GI cancer surgery. The protocol underwent external validation and subsequent refinements before being finalized through expert consensus.
Results
The protocol development process was organized into four consecutive phases: keyword selection, literature review and case report form development, initial protocol drafting, and external validation leading to the final version of the protocol. The final version of the rehabilitation protocol is presented in the main text and included as Supplements.
Conclusion
This protocol provides a standardized clinical guideline based on the latest evidence-based pre- and re-habilitation strategies and is designed for seamless integration into routine clinical practice. By facilitating proactive rehabilitation interventions, it aims to improve outcomes in GI cancer patients who are at high risk of postoperative complications, functional decline, and malnutrition.
- 3,241 View
- 102 Download

- Impact of postoperative nutritional status on the patients’ clinical outcomes and knee biomechanics following total knee arthroplasty in Japan: a prospective cohort study
- Kenichi Kono, Tetsuya Tomita, Takaharu Yamazaki, Masashi Tamaki, Shuji Taketomi, Ryota Yamagami, Reo Inoue, Yuki Taniguchi, Sakae Tanaka, Kazuhiko Fukatsu
- Ann Clin Nutr Metab 2025;17(1):50-57. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.019
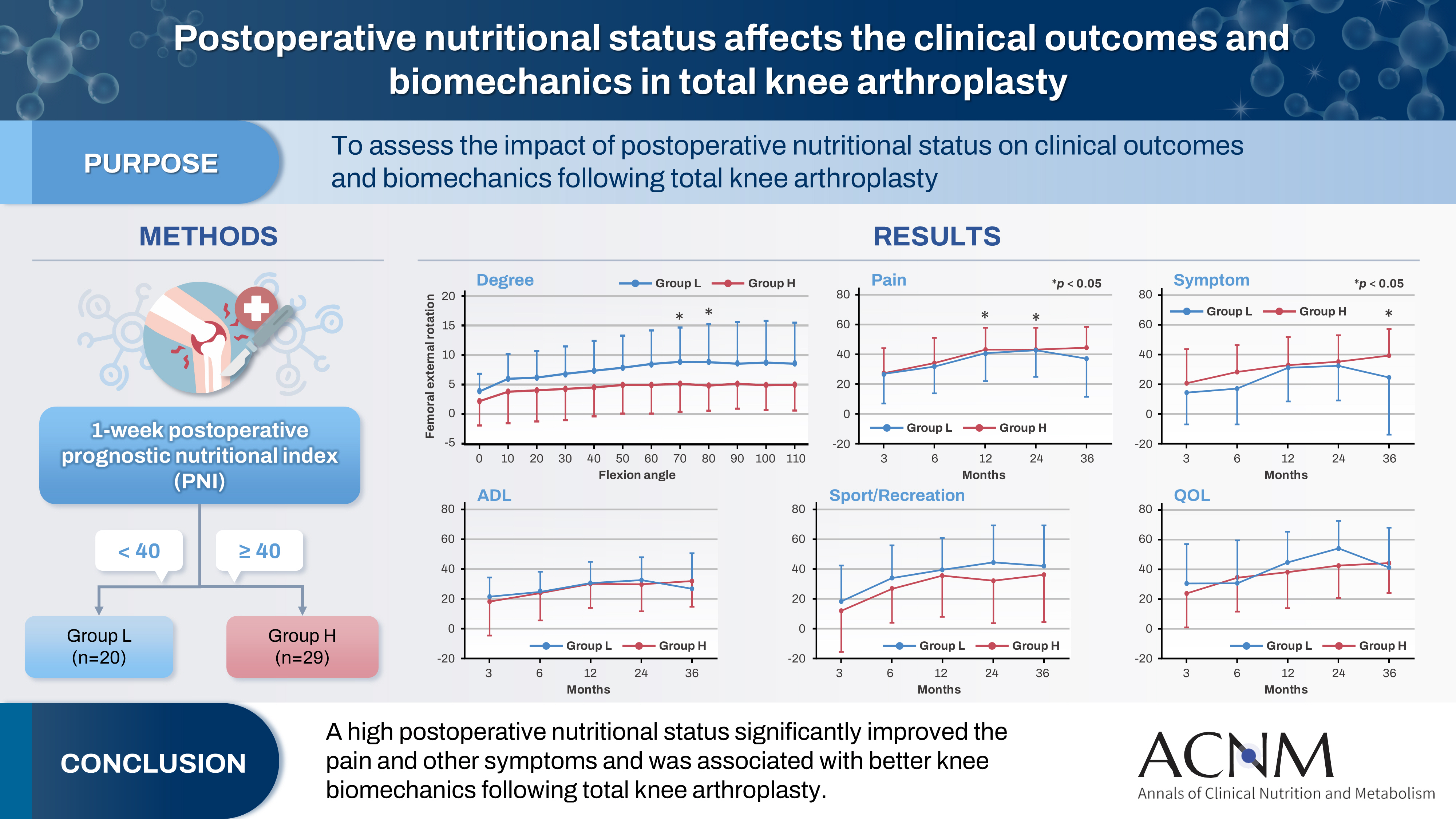
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 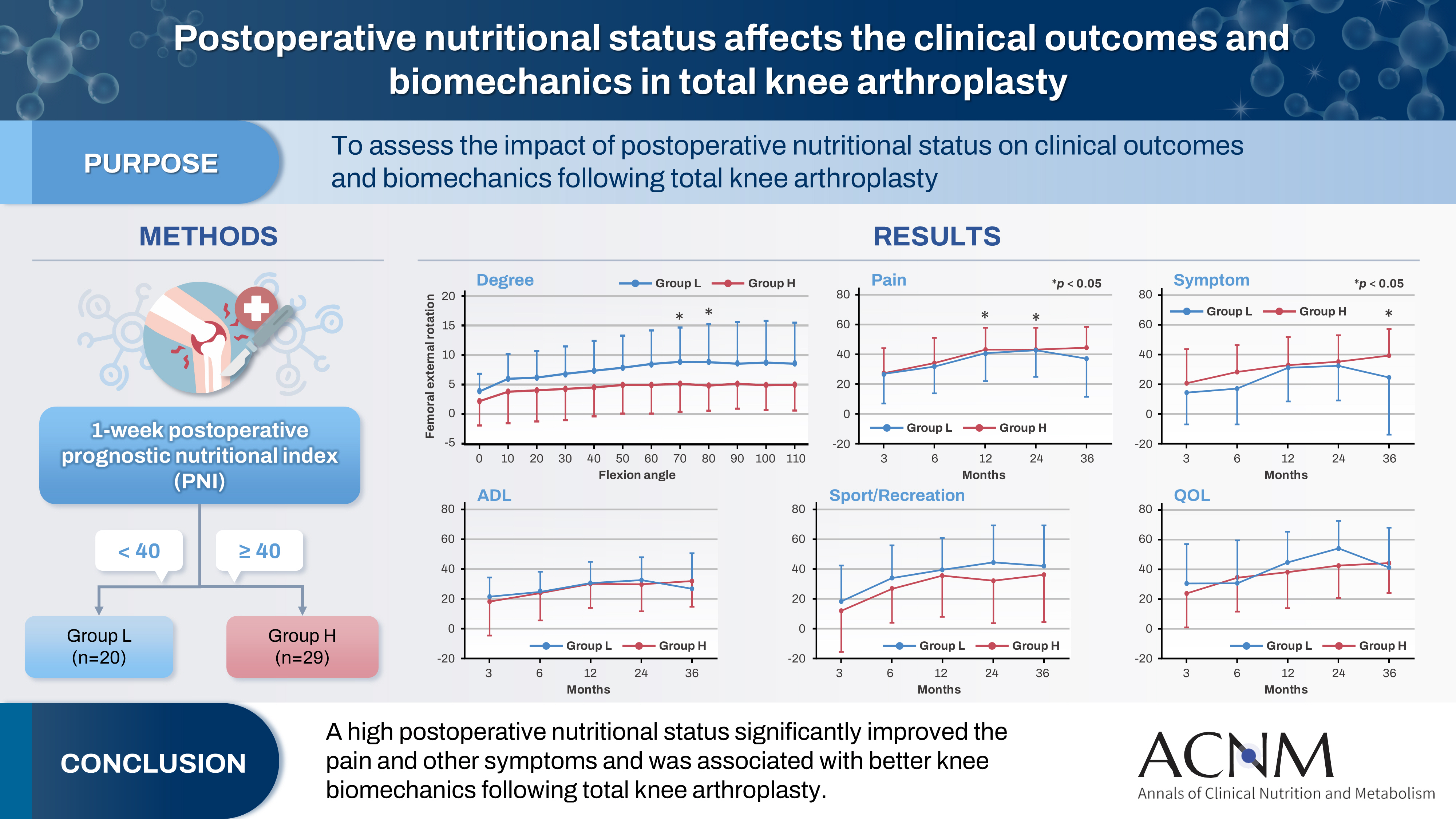
- Purpose
The impact of postoperative nutritional status on clinical outcomes and biomechanics following total knee arthroplasty remains largely unknown. This study aimed to assess this question using the prognostic nutritional index to evaluate the nutritional status of orthopedic participants.
Methods
Patients with knee osteoarthritis who underwent total knee arthroplasty (n=49) in Japan were divided into two groups based on their 1-week postoperative prognostic nutritional index. Group L patients had a prognostic nutritional index <40, whereas Group H comprised patients with a prognostic nutritional index ≥40. Postoperative improvements in Knee Injury and Osteoarthritis Outcome Score were evaluated. The patients performed squats under single-fluoroscopic surveillance in the sagittal plane for biomechanical evaluation. A two-dimensional/three-dimensional registration technique was employed to measure the tibiofemoral kinematics. The axial rotation of the femoral component relative to the tibial component and the anteroposterior translation of the medial and lateral femorotibial contact points were measured.
Results
Group H showed significantly higher pain scores than Group L at 12 and 36 months postoperatively and a significantly higher symptom score at 36 months postoperatively. The kinematic comparison revealed that the axial external rotation in Group L was larger than that in Group H from 70° to 80° with flexion. Moreover, in the medial anteroposterior translation, Group L was more anteriorly located than Group H, with flexion beyond 30°.
Conclusion
The results suggest that a high postoperative nutritional status significantly improved pain and other symptoms and was associated with better knee biomechanics following total knee arthroplasty.
- 2,504 View
- 37 Download

- Comparison of efficacy of enteral versus parenteral nutrition in patients after esophagectomy in Malaysia: a prospective cohort study
- Ramizah Mohd Shariff, Sze Chee Tee, Shukri Jahit Mohammad, Khei Choong Khong
- Ann Clin Nutr Metab 2025;17(1):41-49. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.016
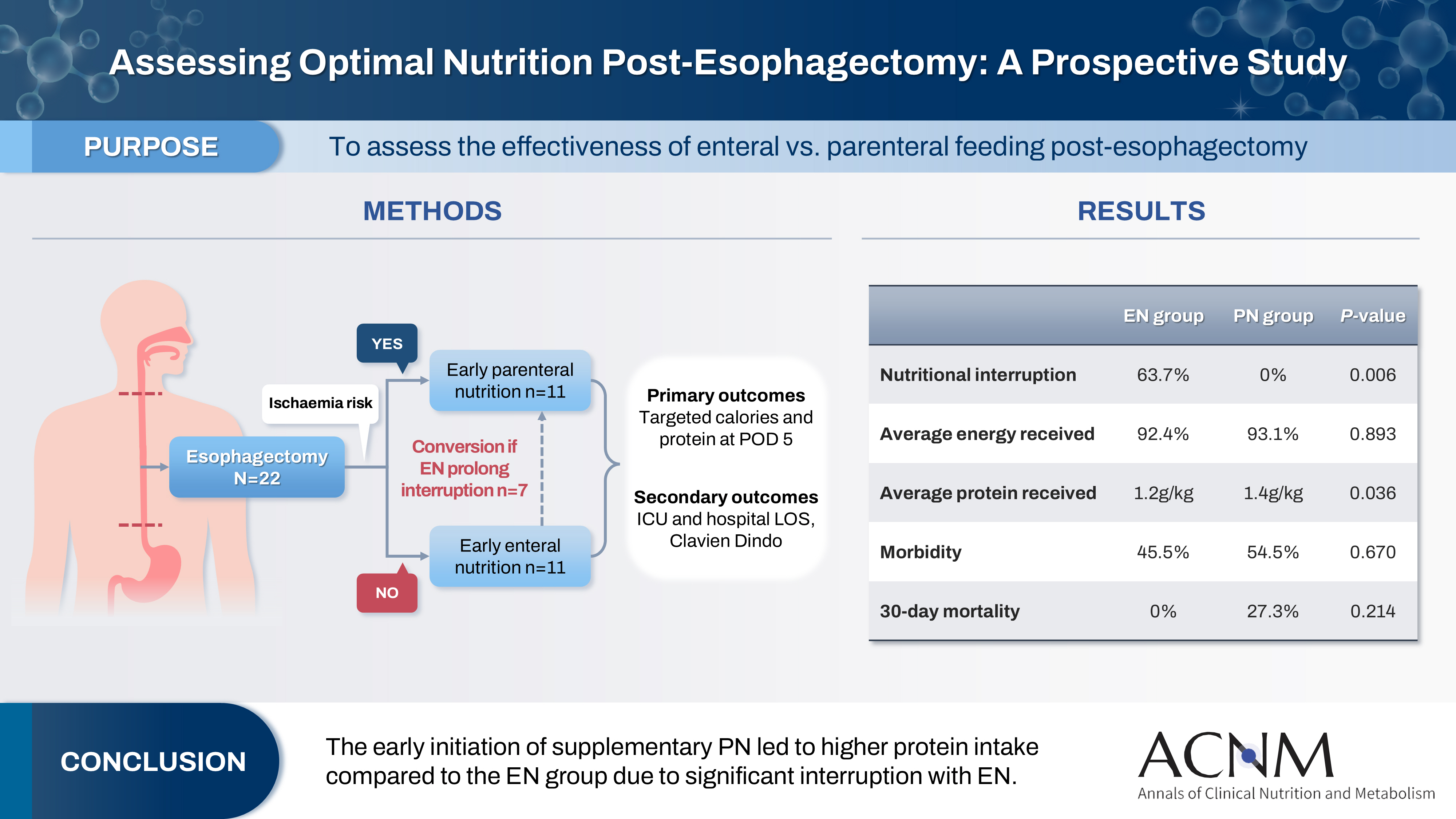
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 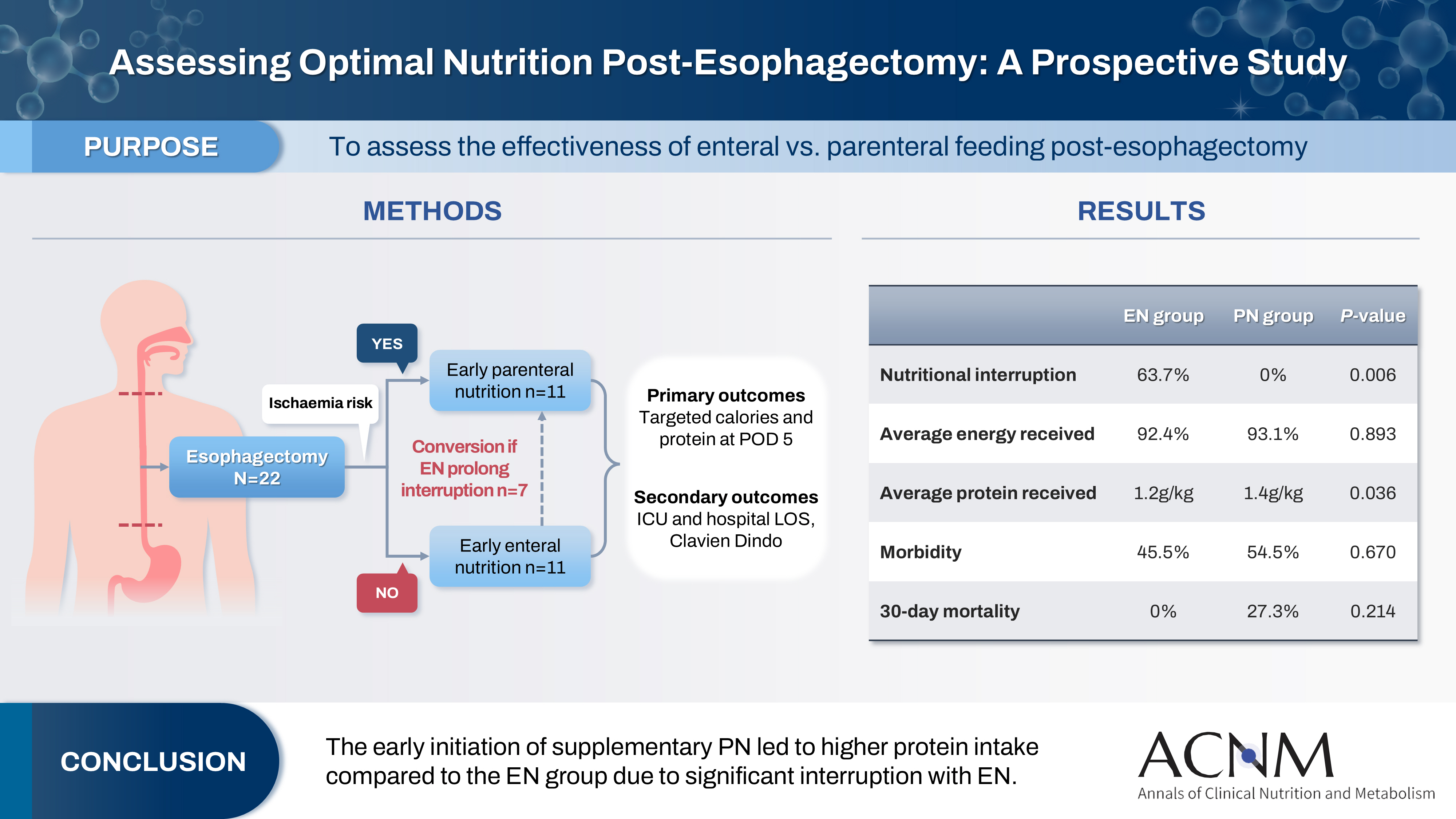
- Purpose
This study aims to assess the effectiveness of enteral versus parenteral feeding in patients after esophagectomy.
Methods
This a prospective cohort study of post-esophagectomy intensive care unit (ICU) patients over 12 months in the National Cancer Institute, Malaysia. Early enteral feeding followed the Enhanced Recovery After Surgery protocol, and parenteral nutrition (PN) was considered if there was a risk for conduit ischemia. It compared the effectiveness of enteral versus PN following esophagectomy, and assessed the correlations between biochemical nutritional markers and hospital lengths of stay or ventilation days.
Results
It included two cohorts receiving PN (n=11) or enteral nutrition (EN) (n=11) following elective esophagectomy. Preoperative weight, body mass index, and Subjective Global Assessment were higher in the EN group (P=0.033, P=0.021, P=0.031, respectively). Nutritional interruption occurred more frequently in the EN group (63.7%) compared to the PN group (P=0.001). Mean levels of energy and protein received were 93.1 kcal/kg and 1.4 g/kg for PN versus 92.4 kcal/kg and 1.2 g/kg for EN (P=0.893, P=0.036). The median lengths of ICU stay (P=0.688) and postoperative stay (P=0.947) between groups showed no significant difference. In addition, 30-day mortality (P=0.214) and other postoperative complications (P>0.05) were comparable in the two groups.
Conclusion
Early initiation of supplementary PN due to significant interruption in EN led to higher protein intake compared to the EN group. However, there were no significant differences in postoperative outcomes, including 30-day mortality, ICU length of stay, and ventilation days. PN ensures adequate nutritional intake, especially in terms of protein delivery, without adversely affecting postoperative recovery and clinical outcomes. -
Citations
Citations to this article as recorded by- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
Ioana Alexandra Prisacariu, Konstantinos Eleftherios Koumarelas, Konstantinos Argyriou, Alexandros Charalabopoulos, Grigorios Christodoulidis
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
- 5,192 View
- 64 Download
- 1 Crossref

Guideline
- Nutritional support for critically ill patients by the Korean Society for Parenteral and Enteral Nutrition — part I: a clinical practice guideline
- Seung Hwan Lee, Jae Gil Lee, Min Kwan Kwon, Jiyeon Kim, Mina Kim, Jeongyun Park, Jee Young Lee, Ye Won Sung, Bomi Kim, Seong Eun Kim, Ji Yoon Cho, A Young Lim, In Gyu Kwon, Miyoung Choi, KSPEN Guideline Committee
- Ann Clin Nutr Metab 2024;16(3):89-111. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.89
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Nutritional support for adult critically ill patients is essential due to the high risk of malnutrition, which can lead to severe complications. This paper aims to develop evidence-based guidelines to optimize nutritional support in intensive care units (ICUs).
Methods: The Grading Recommendations, Assessment, Development and Evaluation process was used to develop and summarize the evidence on which the recommendations were based. Clinical outcomes were assessed for seven key questions.
Results: We recommend the following: (1) initiate enteral nutrition (EN) within 48 hours after treatment as it is associated with improved outcomes, including reduced infection rates and shorter ICU stays; (2) early EN is preferred over early parenteral nutrition due to better clinical outcomes; (3) the use of supplementary parenteral nutrition to meet energy targets during the first week of ICU admission in patients receiving early EN is conditionally recommended based on patient-specific needs; (4) limited caloric support should be supplied to prevent overfeeding and related complications, particularly in the early phase of critical illness; (5) higher protein intake is suggested to improve clinical outcomes, such as muscle preservation and overall recovery; (6) additional enteral or parenteral glutamine is conditionally recommended against due to the lack of significant benefit and potential harm; and (7) fish oil-containing lipid emulsions is conditionally recommended due to their potential to enhance clinical outcomes, including reduced infection rates and shorter ICU stays.
Conclusion: These evidence-based recommendations can improve clinical outcomes and support healthcare providers in making informed decisions about nutritional interventions in the ICU. -
Citations
Citations to this article as recorded by- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
Paraskevi Papanikolaou, Xenophon Theodoridis, Androniki Papaemmanouil, Niki N. Papageorgiou, Alexandra Tsankof, Anna-Bettina Haidich, Christos Savopoulos, Konstantinos Tziomalos
Journal of Clinical Medicine.2025; 14(3): 991. CrossRef
- Enteral Nutrition Versus a Combination of Enteral and Parenteral Nutrition in Critically Ill Adult Patients in the Intensive Care Unit: An Overview of Systematic Reviews and Meta-Analysis
- 24,090 View
- 599 Download
- 1 Crossref

Original Articles
- Kumamoto Earthquake NST activity report: food problems in evacuation shelters in comparison with convalescent facilities
- Joji Kotani, Isamu Yamada, Takahiro Ueda
- Ann Clin Nutr Metab 2024;16(3):173-180. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.173
-
 Abstract
Abstract
 PDF
PDF - Purpose: It aims to investigate the contents of food supplies, gastrointestinal symptoms, and stated preferences of evacuees during the first two weeks after the earthquake.
Methods: Thirty-four evacuees from evacuation shelters and 12 evacuees from geriatric care facilities were surveyed. Subjective and comprehensive nutritional assessment questionnaires were administered to the evacuees, and their dissatisfaction and preferences were also recorded in an open-ended format.
Results: Weight decreased, remained unchanged, increased, or was unknown for 4, 24, 6, and 0 evacuees from the shelters and in 0, 8, 1, and 3 evacuees from the facilities. The number of respondents who reported a decrease, change, or decrease in food intake was 4, 22, and 1 from the evacuation centers and 1, 10, and 1 from the facilities, indicating a large number of changes in the evacuation centers. Reasons for weight gain included “feeling that they should not leave food behind,” “eating a lot of high-calorie food,” and “eating sweets and cup noodles.” Constipation was the most common gastrointestinal symptom (n=5) in the evacuation centers, while diverse symptoms were reported from the facilities. Constipation in the facilities was thought to be related to the high carbohydrate content of the food. Only two respondents were satisfied with the shelter, and the majority complained of dissatisfaction. The most common complaints were “I don’t like bread in the morning (I prefer rice);” “Too sweet;” and “Onigiri (rice ball) is too big,” but there were also complaints about the eating environment on the floor, such as “I lose [my] appetite when eating on the floor due to abdominal pressure” (I prefer to eat on a chair at a table). The majority of the respondents in the facilities did not have any complaints. All of the respondents in the shelters expressed a wide variety of food preferences, including vegetables, rice in the morning, meat, fruit, and foods that were not available due to lack of refrigeration, such as carbonated beverages and ice cream. Some respondents expressed that they were tired of being given food unilaterally and having no choice, such as “I want to choose my own food” and “I want a vending machine [to choose my own food].” There were almost no requests for food at the facilities, and the majority of the respondents were satisfied with their situation. The food was supplied by volunteers and the Self-Defense Forces, which were out of sync with the needs of the evacuees at the evacuation center. However, at the facilities, food was sent to a geriatric care facility in a remote area that accounted for the needs of the victims.
Conclusion: Evacuees were grateful for the food supplies immediately after the disaster, but gradually became dissatisfied. Meals are one of the pleasures in evacuation centers and are important for reducing mental stress. Evacuation centers should consider the needs of evacuees when providing food to evacuees.
- 2,165 View
- 33 Download

- Triglyceride-glucose index predicts future metabolic syndrome in an adult population, Korea: a prospective cohort study
- Min-Su Park
- Ann Clin Nutr Metab 2024;16(3):168-172. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.168
-
 Abstract
Abstract
 PDF
PDF - Purpose: The triglyceride-glucose (TyG) index has been proposed as a reliable surrogate marker for insulin resistance. This study aimed to assess the utility of the TyG index in predicting the future presence of metabolic syndrome (MetS) in an adult population.
Methods: A total of 3,241 adults aged 40–70 years were included in this cross-sectional study. MetS was diagnosed based on the modified National Cholesterol Education Program Adult Treatment Panel III criteria, which requires the presence of at least three of the following components: abdominal obesity, elevated blood pressure, dysglycemia, hypertriglyceridemia, and low high-density lipoprotein cholesterol.
Results: In comparison to the homeostasis model assessment of insulin resistance (HOMA-IR), the TyG index exhibited superior diagnostic performance, with a higher area under the receiver operating characteristic curve of 0.854 vs. 0.702 for HOMA-IR. The 95% confidence interval for the TyG index was narrower, reflecting a more consistent predictive ability. Sensitivity for the TyG index was 79.7%, while specificity was 79.3%, compared to HOMA-IR, which showed a sensitivity of 52.7% and specificity of 78.3%.
Conclusion: The TyG index is a highly effective and robust tool for identifying individuals at risk for MetS, demonstrating superior sensitivity and predictive accuracy over HOMA-IR. This index could be a valuable clinical marker for early detection of MetS, aiding in the prevention and management of associated metabolic disorders. -
Citations
Citations to this article as recorded by- Triglyceride Glucose Index Is More Robust Surrogate Biomarker for Predicting Type 2 Diabetes Mellitus Than HOMA-IR in Population Attending Aulaqi Specialized Medical Laboratories, Yemen
Mohammed Hajar, Sami Ahmed, Basem Abdulfattah
American Journal of Laboratory Medicine.2026; 11(1): 9. CrossRef - Potential Associations of TyG Index and TG/HDL Ratio with Semen Parameters in Infertile Men
Ekrem Başaran, Ahmet Yıldırım Balık, Arda Taşkın Taşkıran, Dursun Baba, Muhammet Ali Kayıkçı
Sağlık Bilimlerinde Değer.2026; 16(1): 98. CrossRef - Elevated triglyceride-glucose index and risk of thymoma-associated myasthenia gravis: a prospective analysis from the UK Biobank
Kangle Zhu, Jingwei Shi, Jingwei Zhao, Yi Zhao, Yao Zhang, Wuji Zhang, Mingjun Wei, Chu Zhou, Rusong Yang, Zhengcheng Liu, Zhuo Liu, Zhixiang Shen
Cardiovascular Diabetology.2025;[Epub] CrossRef - Association Between Triglyceride-Glucose Index and HbA1c in Prediabetes: A Preliminary Evaluation of a Potential Biomarker
Dharani A, Aravind Raj
Journal of MedVerse Research & Practice.2025; : 32. CrossRef
- Triglyceride Glucose Index Is More Robust Surrogate Biomarker for Predicting Type 2 Diabetes Mellitus Than HOMA-IR in Population Attending Aulaqi Specialized Medical Laboratories, Yemen
- 9,602 View
- 99 Download
- 4 Crossref

- Micronutrient deficiencies in copper, zinc, and vitamin D as predictors of clinical outcomes in critically ill surgical patients in Korea: a retrospective cohort study
- Jiae Kim, Yanghee Jun, Ye Rim Chang, Jong-Kwan Baek, Hak-Jae Lee, Hyewon Han, Suk-Kyung Hong
- Ann Clin Nutr Metab 2024;16(3):158-167. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.158
-
 Abstract
Abstract
 PDF
PDF - Purpose: To investigate the prevalence of copper, zinc, and vitamin D deficiencies in surgical intensive care unit (SICU) patients and the associations between those deficiencies and clinical outcomes.
Methods: We conducted a retrospective study of 210 patients admitted to the SICU of Asan Medical Center between June 2020 and June 2022. Micronutrient levels were measured within 7 days of SICU admission. Primary outcomes were the mortality rate, length of SICU stay, hospital stay duration, and mechanical ventilation duration.
Results: Copper deficiency was found in 35% (68/193), zinc deficiency in 52% (100/193), and severe vitamin D deficiency in 46% (82/179) of patients. Copper-deficient patients showed a significantly higher mortality rate (25.0% vs. 12.8%, P=0.044), longer hospital stays (57.8±47.0 vs. 45.2±36.6 days, P=0.041), and extended mechanical ventilation duration (26.9±23.3 vs. 18.8±15.7 days, P=0.012). Zinc deficiency was associated with higher C-reactive protein levels (16.2±9.5 vs. 11.5±8.8 mg/dL, P=0.001) and lower prealbumin levels (6.5±2.8 vs. 9.9±5.6 mg/dL, P<0.001). Severe vitamin D deficiency (<10 ng/mL) was not significantly associated with mortality or other clinical outcomes (mortality: <10 ng/mL vs. ≥10 ng/mL, 13% vs. 18%, P=0.583).
Conclusion: Micronutrient deficiencies are prevalent in SICU patients. Copper deficiency significantly correlated with poor clinical outcomes, and zinc deficiency showed a strong association with inflammatory markers. Early assessment and supplementation of micronutrients could be beneficial for critically ill surgical patients.
- 4,515 View
- 64 Download

- The impact of nutritional intervention by a nutrition support team on extrauterine growth restriction in very low birth weight infants in Korea: a retrospective cohort study
- Seung Yun Lee, Hye Su Hwang, Waonsun Im, Hyojoung Kim, Mi Lim Chung
- Ann Clin Nutr Metab 2024;16(3):149-157. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.149
-
 Abstract
Abstract
 PDF
PDF - Purpose: Achieving proper weight gain through adequate nutrition is critically important in very low birth weight (VLBW) infants. Despite recent active nutritional interventions, growth restriction is still common in VLBW infants. We aimed to determine whether nutritional intervention by a nutrition support team (NST) mitigated extrauterine growth restriction (EUGR) in VLBW infants.
Methods: We retrospectively reviewed the medical records of VLBW infants admitted to Haeundae Paik Hospital between March 2010 and February 2024. EUGR was defined as a decrease in the weight-for-age-z-score>1.2 from birth to the postconceptional age of 36 weeks, using Fenton growth charts.
Results: Among the 603 enrolled VLBW infants, 434 (72.0%) were diagnosed with EUGR. When comparing the control and nutritional intervention groups, the incidence of EUGR was significantly lower in infants in the intervention group (80.6% vs. 62.8%, P<0.00). Intervention group infants started enteral feeding earlier and reached half and full enteral feeding earlier (P<0.05). In addition, intravenous protein and lipid supply started sooner, increased at a faster rate, and reached peak concentrations sooner in the intervention group (P<0.05).
Conclusion: Nutritional intervention by an NST resulted in a significant decrease in the development of EUGR in VLBW infants.
- 2,610 View
- 55 Download

- Perioperative nutritional practice of surgeons in Korea: a survey study
- Ji-Hyeon Park, Mi Ran Jung, Sang Hyun Kim, Hongbeom Kim, Gyeongsil Lee, Jae-Seok Min, Heung-Kwon Oh, Jung Hoon Bae, Yoona Chung, Dong-Seok Han, Seung Wan Ryu, The External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(3):134-148. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.134
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Enhanced recovery after surgery (ERAS) protocols advocate reduced fasting and early nutrition to improve recovery in surgical patients. However, data on ERAS implementation among Korean surgeons performing major abdominal surgeries remain sparse.
Methods: A survey conducted by the External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition assessed perioperative nutritional practices among 389 Korean general surgeons from February to September 2023. The survey covered preoperative fasting, carbohydrate drinks, nasogastric tube use, postoperative dietary progression, parenteral nutrition (PN), and oral supplements, yielding 551 responses stratified by specialty.
Results: More than 80% of respondents practiced “midnight NPO (Nil Per Os)” fasting, often at the anesthesiology department’s request, while 70%–80% reported no use of preoperative carbohydrate drinks. Most surgeons began dietary progression with water on postoperative day one, advancing to a liquid or soft diet by day two. PN was routinely prescribed by 49% of respondents, with a common dosage of 1,000–1,500 kcal/d. Oral supplements were selectively provided, with 21% of surgeons prescribing them universally.
Conclusion: The results reveal significant variability in perioperative nutrition practices across Korean surgical specialties, with many adhering to traditional practices despite ERAS guidelines. These findings highlight a need for standardized guidelines in Korea to optimize perioperative nutritional support and improve patient recovery outcomes following major abdominal surgeries. -
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Perioperative nutrition practices in gastrointestinal cancer surgery: A nationwide survey among German surgical departments
Rahel Maria Strobel, Katharina Beyer, Johannes Christian Lauscher, Marc Martignoni, Christoph Reißfelder, Tim Vilz, Arved Weimann, Maria Wobith
Langenbeck's Archives of Surgery.2025;[Epub] CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 6,302 View
- 85 Download
- 2 Crossref

- Incidence and risk factors of nonalcoholic fatty liver disease after pancreaticoduodenectomy in Korea: a multicenter retrospective cohort study
- Chang-Sup Lim, Hongbeom Kim, In Woong Han, Won-Gun Yun, Eunchae Go, Jaewon Lee, Kyung Chul Yoon, So Jeong Yoon, Sang Hyun Shin, Jin Seok Heo, Yong Chan Shin, Woohyun Jung
- Ann Clin Nutr Metab 2024;16(3):125-133. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.125
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study aimed to investigate the incidence, risk factors, and clinical course of nonalcoholic fatty liver disease (NAFLD) following pancreaticoduodenectomy, focusing on the role of adjuvant chemotherapy and other metabolic changes.
Methods: A retrospective analysis was conducted on 189 patients who underwent pancreaticoduodenectomy between 2013 and 2016. NAFLD was diagnosed using computed tomography (CT) imaging, defined as a liver-to-spleen attenuation ratio <0.9. Sarcopenia and sarcopenic obesity were assessed using preoperative CT scans. Logistic regression analysis was performed to identify risk factors for NAFLD development.
Results: The cumulative incidence of NAFLD increased over time, with rates of 15.9% at one year, 20.4% at three years, and 35.2% at five years post-pancreaticoduodenectomy. Adjuvant chemotherapy was identified as the only significant independent predictor of NAFLD development (odds ratio, 2.74; 95% confidence interval, 1.16-6.70; P=0.023). No significant associations were found between NAFLD and pancreatic enzyme replacement therapy (PERT), sarcopenia, or sarcopenic obesity. Serial analysis of NAFLD status in long-term survivors revealed dynamic changes, with some patients experiencing spontaneous remission or recurrence.
Conclusion: NAFLD is a common, progressive complication following pancreaticoduodenectomy, particularly in patients receiving adjuvant chemotherapy. Although no significant associations with PERT or sarcopenia were observed, these areas warrant further investigation. Long-term monitoring and targeted management strategies are recommended to address NAFLD in this population. Future prospective studies are needed to elucidate the natural history and contributing factors of NAFLD after pancreaticoduodenectomy.
- 3,422 View
- 60 Download

Reviews
- Changes in perceptions of taste after bariatric surgery: a narrative review
- Young Suk Park
- Ann Clin Nutr Metab 2024;16(3):120-124. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.120
-
 Abstract
Abstract
 PDF
PDF - Purpose: Bariatric surgery effectively treats severe obesity, leading to significant weight loss and improved comorbidities. However, many patients experience postoperative alterations in taste perception, affecting food selection and eating behavior. This narrative review examines the current understanding of taste perception changes following bariatric surgery, including patterns, potential mechanisms, impact on weight loss outcomes, and implications for patient care.
Current concept: Changes in taste perception are frequently reported after bariatric procedures, with prevalence rates from 36% to 72%. Common alterations involve decreased preference and increased sensitivity to sweet and fatty tastes, potentially leading to reduced calorie intake and healthier food choices. Persistence of these changes varies and may depend on surgery type, with Roux-en-Y gastric bypass patients often experiencing more substantial effects than sleeve gastrectomy patients. Potential mechanisms include alterations in gut hormone secretion (e.g., GLP-1, peptide YY, ghrelin), modifications in neural pathways (e.g., vagus nerve), and shifts in the gut microbiome. These factors may collectively influence taste sensitivity and preferences, contributing to weight loss outcomes. Altered reward processing may reduce the appeal of high-calorie foods.
Conclusion: Alterations in taste perception are common after bariatric surgery and may significantly impact dietary behaviors, weight loss, and quality of life. While exact mechanisms are not fully understood, changes in gut hormones, neural pathways, and microbiota are likely involved. Patient counseling and postoperative management of bariatric surgery patients should address potential changes in taste. Further research is needed to elucidate the long-term impacts of taste alterations on weight-loss maintenance and nutritional status.
- 5,372 View
- 57 Download

- Mental health and micronutrients: a narrative review
- Hyun Wook Baik
- Ann Clin Nutr Metab 2024;16(3):112-119. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.112
-
 Abstract
Abstract
 PDF
PDF - Purpose: It aims to summarizes the evidence for the association between specific individual nutrients and mental disorders, focusing on vitamin B12 and related B vitamins, vitamin D, probiotics, and zinc.
Current concept: Vitamin D deficiency is linked to depression, anxiety, and cognitive decline. Vitamin D enhances serotonin synthesis, has anti-inflammatory and neuroprotective effects, and regulates the hypothalamic-pituitary-adrenal axis and circadian rhythms. Vitamin B12 deficiency causes neurological dysfunction, mood disorders, cognitive decline, and psychotic symptoms, especially in the elderly. Vitamin B12 is involved in myelin formation, neurotransmitter synthesis, and preventing homocysteine-related neurodegeneration. Zinc deficiency affects neurotransmitters, neurogenesis, and antioxidant function, contributing to depression, anxiety, and cognitive impairment. Zinc supplementation improves symptoms and increases brain-derived neurotrophic factor levels. The gut-brain axis involves bidirectional communication between the gut microbiome and the central nervous system via the vagus nerve, enteric nervous system, immune system, and neuroendocrine pathways. Probiotics can modulate the gut microbiome to improve depression, anxiety, stress response, and cognitive function by influencing neurotransmitter production, reducing inflammation, and supporting the gut-brain connection.
Conclusion: Nutritional interventions, including vitamin D, B12, zinc, and probiotics, show promise as adjunctive therapies or preventive strategies for mental disorders. These nutrients have specific mechanisms of action on brain function and the gut-brain axis. Further research is needed to establish optimal dosage, timing, and administration methods for these nutritional approaches in supporting mental health. -
Citations
Citations to this article as recorded by- The Mouth–Mind Connection: Interplay of Oral and Mental Health in Older Adults
Alice Kit Ying Chan, Joanna Cheuk Yan Hui, Lindsey Lingxi Hu, Chun Hung Chu
Geriatrics.2026; 11(1): 8. CrossRef - Associations between antioxidant vitamin intake and mental health in Swedish adolescents: a cross-sectional study
Martina Pensa, Karin Kjellenberg, Emerald Heiland, Örjan Ekblom, Gisela Nyberg, Björg Helgadóttir
European Journal of Nutrition.2025;[Epub] CrossRef - A Study of Nutritional and Sensory Qualities of Pea Protein Isolate Beverages with a View to Their Potential Use in Patients with Psychiatric Disorders
Lasma Plocina, Ilze Beitane
Foods.2025; 14(17): 2991. CrossRef - The association between animal‑based and plant‑based protein intake with sleep quality, mood, anxiety, depression and stress among elderly: a cross-sectional study
Batoul Ghosn, Hanieh Abbasi, Parisa Nezhad Hajian, Leila Azadbakht
BMC Public Health.2025;[Epub] CrossRef - Pediatric Culinary Medicine: Current Status, Challenges and Opportunities
Michelle Loy, Ashish Chogle, Hanna Tracy, Neha R Santucci, Khyati Mehta, Liane S. Sadder, Rima Jibaly, Alain J. Benitez, Maria R. Mascarenhas
Current Gastroenterology Reports.2025;[Epub] CrossRef - ВІТАМІН В12, ДЕПРЕСІЯ І ЦУКРОВИЙ ДІАБЕТ 2 ТИПУ (огляд лiтератури)
Вікторія Сергієнко, Вероніка Сегін, Олександр Сергієнко
Problems of Endocrine Pathology.2025; 82(4): 54. CrossRef
- The Mouth–Mind Connection: Interplay of Oral and Mental Health in Older Adults
- 51,547 View
- 648 Download
- 6 Crossref

Interesting image
- Pneumothorax due to malpositioned nasogastric enteral feeding tube
- Hyebeen Kim, Suk-Kyung Hong
- Ann Clin Nutr Metab 2024;16(2):87-88. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.87
- 1,943 View
- 30 Download

Original Articles
- Impact of immune-supplementation on muscle health and inflammation status of South Indian patients who have undergone gastrointestinal resection: a pilot randomized-controlled study
- Nivedita Pavithran, Catherine Bompart, Alisa Alili, Sudheer Othiyil Vayoth
- Ann Clin Nutr Metab 2024;16(2):78-86. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.78
-
 Abstract
Abstract
 PDF
PDF - Purpose: Gastrointestinal (GI) resection significantly impacts nutritional and physical health, causing stress and inflammation that increase energy needs. Post-operative caloric intake often falls short, disrupting protein homeostasis and compromising muscle health. Nutritional supplementation is crucial to reduce inflammation and maintain muscle health. This study aimed to evaluate the impact of a three-week oral nutritional immuno-supplement (IMM) intervention compared to a control (CTL) on post-operative inflammatory status and muscle health in patients receiving limb and chest physiotherapy from June to August 2023.
Methods: A randomized, controlled, blinded cohort of 20 patients (ages 30–75) undergoing GI surgery was established. Participants were recruited on the day of surgery and assigned to either the CTL, which received standard protein supplementation, or the IMM group, which received protein immune-enriched supplementation for three weeks. All participants also received chest and limb physiotherapy. Follow-up and data collection were conducted at three post-surgery time points: 3 days, 7 days, and 3 weeks. Assessments included body composition, handgrip strength, basal metabolic rate, 24-hour dietary intake, and C-reactive protein (CRP) levels.
Results: Fifteen patients completed the study (IMM=9, CTL=6). After three weeks of supplementation, the IMM group showed a significant increase in lean mass percentage and handgrip strength, along with a significant decrease in CRP levels, compared to the CTL.
Conclusion: A 3-week oral immuno-supplement provided to patients post-GI resection, in conjunction with limb and chest physiotherapy, is more effective in reducing inflammation and preserving muscle health compared to standard protein supplementation.
- 1,499 View
- 14 Download

- Prognostic significance of serum creatinine and sarcopenia for 5-year overall survival in patients with colorectal cancer in Korea: a comparative study
- Jiahn Choi, Hye Sun Lee, Jeonghyun Kang
- Ann Clin Nutr Metab 2024;16(2):66-77. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.66
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Previous studies have demonstrated that the serum creatinine level and skeletal muscle index (SMI) (correlated with the overall survival [OS] of patients with colorectal cancer [CRC]). However, the combined significance of these 2 factors is not fully understood. The goal of this study was to investigate the prognostic potential of the combination of these two factors in patients with CRC.
Methods: The patients were categorized into subgroups based on preoperative serum creatinine level, with a cut-off value of 1.01 mg/dL for males and 0.80 mg/dL for females. The patients were further categorized into 4 groups based on SMI. Data were analyzed using the Cox proportional hazards model and Harrell’s concordance index (C-index).
Results: Poor 5-year OS was observed in patients with high SMI and high serum creatinine levels (hazard ratio [HR]=1.676, 95% confidence interval [CI]=1.110–2.529, P=0.013), low SMI and low serum creatinine levels (HR=1.916, 95% CI=1.249–2.938, P=0.002), and low SMI and high serum creatinine levels (HR=2.172, 95% CI=1.279–3.687, P=0.004) compared to those of patients with high SMI and low serum creatinine levels. Grouping patients based on both SMI and serum creatinine levels led to improved prognostic stratification (C-index, 0.626; 95% CI=0.587–0.666) compared to grouping based on SMI (CI difference=0.062, 95% CI=0.031–0.103, P=0.0011) or serum creatinine (CI difference=0.043, 95% CI=0.017–0.081, P=0.0072) alone.
Conclusion: Incorporating both SMI and serum creatinine levels enhances the prognostic stratification for 5-year OS in patients with CRC, surpassing the prognostic power of grouping solely based on SMI or creatinine.
- 2,969 View
- 18 Download

- Early nutritional support for inpatients reduces admission rates to intensive care units in Korea: a single-center case-control study
- Hyun Suk Kim, Jae Do Yang, Se Wung Han, Mi Rin Lee, Da-Sol Kim, Sejin Lee, Seon-Hyeong Kim, Chan-Young Kim
- Ann Clin Nutr Metab 2024;16(2):57-65. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.57
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Early nutritional support (ENS) for critically ill patients is promoted by many studies. However, there is a lack of data evaluating its necessity in general wards. This study aims to determine the impact of ENS on patients in general wards.
Methods: Patients aged 18 and above, admitted to the Jeonbuk National University Hospital in Jeonju from January 2020 to December 2020, who were eligible for nutritional support and hospitalized for at least 7 days were included in the study. We divided the patients into two groups: the ENS group, who received nutritional support within 48 hours of admission, and the control group, who received it after 48 hours.
Results: Among 1,077 patients, 146 met the inclusion criteria. The ENS group (n=38) and the control group (n=108) were compared retrospectively. There was a significant age difference between the two groups (P=0.028). The admission ratio to the intensive care unit (ICU) in the ENS group was significantly lower than that in the control group (10.2% vs. 26.3%, P=0.019). The calorie support rate (%) and protein support rate (%) in the ENS group were significantly higher than in the control group (50.12%±23.30% vs. 38.56%±18.02%, P=0.006; 44.61%±25.07% vs. 32.07%±22.76%, P=0.002, respectively). After propensity score matching, the ENS was significantly associated with ICU low admissions (odds ratio 0.08, 95% confidence interval 0.01–0.69, P=0.022).
Conclusion: A future multi-center study considering underlying diseases is needed to provide additional scientific evidence to support the effects of ENS.
- 2,387 View
- 25 Download

Reviews
- Definition, assessments, and current research on sarcopenia in children: a narrative review
- Min-Jung Bang
- Ann Clin Nutr Metab 2024;16(2):49-56. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.49
-
 Abstract
Abstract
 PDF
PDF - Purpose: Sarcopenia is a well-established prognostic factor for the clinical outcomes of adult patients with cancer and chronic diseases and correlates with increased intensive care unit admissions and prolonged hospital stays. However, research on sarcopenia in children is limited due to its undefined criteria and a lack of studies exploring its impact on clinical outcomes.
Current concept: The challenges in pediatric sarcopenia research include the absence of standardized body composition methods to quantify muscle mass and muscular function, as well as inconsistencies in definitions. Additionally, there is a lack of age- and gender-specific normative data, particularly for young children and infants. Most studies also lack assessments of muscle function, which can lead to bias and misclassification of sarcopenia. The field is further hindered by poor study quality, limited outcome-focused research, and a dearth of longitudinal data. While some studies suggest that various diseases can affect children’s lean muscle mass, few have linked changes in muscle mass to clinical outcomes.
Conclusion: The existing literature on pediatric sarcopenia and its relationship with medical and surgical outcomes is sparse and indicates poorer outcomes associated with sarcopenia. Although extensive research has established a link between sarcopenia and adverse outcomes in adults, information on its impact in pediatric populations remains scarce. Further studies are needed to elucidate the association between muscle mass and outcomes in pediatric surgical patients. -
Citations
Citations to this article as recorded by- Newer Insights on the Occurrence of Sarcopenia in Pediatric Patients with Cancer: A Systematic Review of the Past 5 Years of Literature
Georgios Kiosis, Despoina Ioannou, Kanellos Skourtsidis, Vasilis Fouskas, Konstantinos Stergiou, Dimitrios Kavvadas, Theodora Papamitsou, Sofia Karachrysafi, Maria Kourti
Cancers.2025; 17(19): 3188. CrossRef
- Newer Insights on the Occurrence of Sarcopenia in Pediatric Patients with Cancer: A Systematic Review of the Past 5 Years of Literature
- 3,783 View
- 86 Download
- 1 Crossref

- Dysphagia and quality of life: a narrative review
- Jung Mi Song
- Ann Clin Nutr Metab 2024;16(2):43-48. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.43
-
 Abstract
Abstract
 PDF
PDF - Purpose: Dysphagia is a chronic health condition that causes impairment of eating and drinking functions. It occurs in various diseases such as stroke, neurodegenerative disease, brain tumor, and head and neck cancer, and can also occur during the normal aging process.
Current concept: As patients experience symptoms of dysphagia, they no longer feel the pleasure of eating, depression and anxiety increase, and self-esteem decreases. Prolonged loss of appetite can lead to malnutrition, which can lead to death due to serious complications such as aspiration pneumonia and airway obstruction. Dysphagia reduces quality of life by affecting basic activities of daily living, limitations in social life, nutritional deficiencies, and mood disorders.
Conclusion: Accordingly, I plan to conduct a literature review on the quality of life of patients with dysphagia. First, to determine the relationship between quality of life and sociodemographic, physical health, and mental health characteristics of patients with dysphagia. I also aim to review quality of life measurement tools and intervention programs for patients with dysphagia. -
Citations
Citations to this article as recorded by- Incidence and Risk Factors of Dysphagia After Cardiac Surgery: A Scoping Review
Christos Kourek, Vania Labropoulou, Emilia Michou, Stavros Dimopoulos
Journal of Clinical Medicine.2025; 14(12): 4279. CrossRef - Psychometric Properties of the Spanish Version of the Swallowing Quality of Life Questionnaire in Fibromyalgia Patients
Irene Calles-Plata, Araceli Ortiz-Rubio, Laura Pérez-Gisbert, Irene Torres-Sánchez, Andrés Calvache Mateo, Marie Valenza, Alejandro Heredia-Ciuró
Healthcare.2025; 13(22): 2948. CrossRef - Association Between Swallowing Dysfunction and Multidimensional Quality of Life Among Community-Dwelling Healthy Korean Older Adults: A Pilot Cross-Sectional Study
Hyun-Ah Jang, Jun-Seon Choi
Healthcare.2025; 13(22): 2964. CrossRef
- Incidence and Risk Factors of Dysphagia After Cardiac Surgery: A Scoping Review
- 15,928 View
- 296 Download
- 3 Crossref

Guideline
- The 2024 Korean Enhanced Recovery After Surgery guidelines for colorectal cancer
- Kil-yong Lee, Soo Young Lee, Miyoung Choi, Moonjin Kim, Ji Hong Kim, Ju Myung Song, Seung Yoon Yang, In Jun Yang, Moon Suk Choi, Seung Rim Han, Eon Chul Han, Sang Hyun Hong, Do Joong Park, Sang-Jae Park, The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(2):22-42. Published online August 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.2.22
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The Korean Enhanced Recovery After Surgery (ERAS) Committee within the Korean Society of Surgical Metabolism and Nutrition was established to develop ERAS guidelines tailored to the Korean context. This guideline focuses on creating the most current evidence-based practice guidelines for ERAS based on systematic reviews. All key questions targeted randomized controlled trials (RCTs) exclusively. If fewer than two RCTs were available, studies using propensity score matching were also included. Recommendations for each key question were marked with strength of recommendation and level of evidence following internal and external review processes by the committee.
-
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Optimizing postoperative pain management in minimally invasive colorectal surgery
Soo Young Lee
Annals of Coloproctology.2024; 40(6): 525. CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 9,501 View
- 125 Download
- 2 Crossref

Review
- Recent advances in refeeding syndrome in critically ill patients: a narrative review
- Sang Woo Ha, Suk-Kyung Hong
- Ann Clin Nutr Metab 2024;16(1):3-9. Published online April 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.1.3
-
 Abstract
Abstract
 PDF
PDF - Purpose: The aim of this article is to provide a narrative review of the most recent studies on refeeding syndrome (RS) in critically ill patients and to summarize recent advancements that can be referenced in the treatment of these patients.
Current concept: RS in critically ill patients is a potentially lethal nutrition-related condition leading to sudden death. Initiation of food intake after a period of fasting can trigger rapid electrolyte uptake due to increased insulin release, leading to a decline in serum electrolytes with thiamine. This depletion may cause severe complications, such as cardiac arrhythmias, respiratory failure, seizures, and even death. The incidence of RS varies significantly, ranging from 7.4%–89%. Despite updates in diagnostic criteria over time, there remains a crucial need for criteria applicable to critically ill patients with underlying disorders such as metabolic derangement and organ dysfunction. To prevent RS, it is strongly recommended to start food intake after a fast at 20%–25% of estimated goals, gradually increasing the intake over several days. Close monitoring and electrolyte supplementation—especially of phosphorus, potassium, magnesium, and thiamine—are crucial, especially in critically ill patients. If electrolyte imbalances persist, slowing down or halting the progression of nutrition should be considered.
Conclusion: Clinicians should continue their efforts to promptly identify high-risk patients and to provide prevention and treatment for RS, particularly during the initiation of nutritional therapy in critically ill patients. Developing evidence-based protocols through further well-designed research is essential for effectively managing critically ill patients at risk of RS. -
Citations
Citations to this article as recorded by- Nutrition in the critically ill in resource-limited settings/low- and middle-income countries
Mervyn Mer, Martin W. Dünser
Current Opinion in Clinical Nutrition & Metabolic Care.2025; 28(2): 181. CrossRef - Nutritional Management of Liver Failure in the Intensive Care Unit
Zsófia Verzár, Rudolf Kiss, Csaba Pál Bálint, Annamária Pakai, Tímea Csákvári
Medicina.2025; 61(7): 1210. CrossRef - Comprehensive care of the patient with Refeeding Syndrome
Magdalena Kwiatkowska, Dominika Krupnik, Fabian Wesołek, Agnieszka Jonczyk, Łukasz Krzych
Polish Journal of Surgery.2025; 97(5): 64. CrossRef
- Nutrition in the critically ill in resource-limited settings/low- and middle-income countries
- 50,893 View
- 1,240 Download
- 3 Crossref

Original Articles
- Efficacy of high-protein diet protocol and education after distal gastrectomy for gastric cancer patients to prevent loss of lean body mass in Korea: a non-randomized controlled study
- Hee Kyung Yoon, Sun Ae Kim, Ji Yoon Han, Dong Jin Kim
- Ann Clin Nutr Metab 2024;16(1):10-19. Published online April 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.1.10
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: We studied whether active education of patients about the importance of a high-protein diet can prevent lean body mass loss after gastrectomy for gastric cancer.
Methods: In the study group, intensive high protein diet education and monitoring was performed immediate post operative, 1, 3, and 6 months after surgery. Study group patients were compared with data from the control group formed using propensity matching with the study group for age, sex, resection extent, and TNM stage. Clinicopathologic factors were compared between the groups, and changes in quality of life (QOL) and lean body mass between preoperative levels and 6 months after surgery were assessed.
Results: Among the 100 patients, 31 patients from each group were matched with propensity matching. The groups had no significant clinicopathologic differences. Although the changes in QOL scale and body composition did not differ statistically between the groups, a favorable trend was observed in the study group. Six months after surgery, the mean change in the QOL scale, which measured physical, role, emotional, cognitive, and social functioning, decreased less than the control group or even increased in the study group. In the body composition analysis, the study group showed greater reductions in weight, body mass index, fat mass, and body fat percentage than the control group, and their lean body mass and skeletal muscle mass decreased less.
Conclusion: A high-protein diet protocol and education might increase patient QOL and prevent a decrease in lean body weight 6 months after distal gastric resection.
- 4,509 View
- 42 Download

- Comparative assessment of nutritional characteristics of critically ill patients at admission and discharge from the neurosurgical intensive care unit in Korea: a comparison study
- Eunjoo Bae, Jinyoung Jang, Miyeon Kim, Seongsuk Kang, Kumhee Son, Taegon Kim, Hyunjung Lim
- Ann Clin Nutr Metab 2023;15(3):97-108. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.97
-
 Abstract
Abstract
 PDF
PDF - Purpose: Patients in neurosurgical (NS) intensive care units (ICUs) experience considerable energy and protein deficits associated with adverse outcomes. This study aimed to compare the nutritional status of patients at admission to (baseline) and discharge from the NS ICU.
Methods: This was a single-center, retrospective, before and after study of patients admitted in the NS ICU of the CHA Bundang Medical Center, from January 31, 2019, to February 28, 2020. All anthropometric data, biochemical data, clinical data, and dietary data were collected during the NS ICU stay. Specifically, we investigated the cumulative caloric deficit rate, phase angle and skeletal muscle index as indicators of lean muscle mass, and nitrogen balance according to demographic and clinical characteristics.
Results: A total of 140 NS patients were studied. Calf circumference decreased from 31.4±4.2 cm at baseline to 30.2±4.0 cm at discharge (P<0.001). Energy supply rate increased from 44.4% at baseline to 89.2% at discharge. Phase angle (PhA) patients with an modified Nutrition Risk in the Critically ill (mNUTRIC) score≤5 group had significantly lower PhA values than those with an mNUTRIC score>5 (P=0.005).
Conclusion: Although clinical and dietary parameters of patients in the NS ICU improved from baseline to discharge, anthropometric and biochemical markers of lean muscle mass and nutritional status decreased. PhA and nitrogen balance difference values were significantly different between those with an mNUTRIC score≤5 and those with an mNUTRIC score>5. These data indicate that the nutritional risk of critically ill patients increases during hospitalization in the NS ICU. -
Citations
Citations to this article as recorded by- Association between the Modified NUTRIC Score (mNUTRIC) and Clinical Outcomes in a Mixed Intensive Care Unit: A Retrospective Cohort Study
Thanh Luan Nguyen, Quang Dai Le, Trang Nguyen Hoai Dinh, Van Hoang Nam Ho, Cong Dang Tran, Van Phieu Duong, Hoang Ngoc Thao Duong, Phuc Tuong Pham, Thi Phuong Thao Le, Tuyet Phuong Bui
SN Comprehensive Clinical Medicine.2026;[Epub] CrossRef - A Review on the Effects of Multiple Nutritional Scores on Wound Healing after Neurosurgery.
Jingqian Ye, Bo Ning , Jianwen Zhi
International Journal of Biology and Life Sciences.2025; 9(2): 82. CrossRef - Transition from Enteral to Oral Nutrition in Intensive Care and Post Intensive Care Patients: A Scoping Review
Gioia Vinci, Nataliia Yakovenko, Elisabeth De Waele, Reto Stocker
Nutrients.2025; 17(11): 1780. CrossRef
- Association between the Modified NUTRIC Score (mNUTRIC) and Clinical Outcomes in a Mixed Intensive Care Unit: A Retrospective Cohort Study
- 3,412 View
- 28 Download
- 3 Crossref

- Multi-biomarker approach to metabolic syndrome and associated diseases in Turkey: a cross sectional study
- Semra Can Mamur, Omer Colak, Selma Metintas, Inci Arikan, Mehmet Kara
- Ann Clin Nutr Metab 2023;15(3):88-96. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.88
-
 Abstract
Abstract
 PDF
PDF - Purpose: Biomarker for cardiovascular diseases (CVDs) are important in the clinical monitoring of individuals with metabolic syndrome (MetS). The use of these biomarkers in combination may be predictive of CVDs. This study aimed to demonstrate the ability of multiple biomarkers to predict MetS, diabetes mellitus (DM), and CVDs. The use of multiple biomarkers instead of a single biomarker may be more useful in early diagnosis. We investigated the use of a multi-biomarker approach in MetS and associated diseases.
Methods: The study was performed by selecting control (n=30), MetS (n=30), MetS+DM (n=30), and MetS+CVD (n=30) groups from data of the Eskisehir Healthy Hearts Project conducted from January 2008 to October 2009 in Turkey. We recorded serum level of biomarkers, including lipid profile, liver enzyme, paraoxonase, arylesterase and arginase to find their difference among the groups.
Results: Compared to the control group, gamma-glutamyl transferase (GGT) and arginase levels increased, while paraoxonase and arylesterase activity and high-density lipoprotein–cholesterol levels were low in the patient groups (P<0.001). A negative correlation was observed between paraoxonase and arylesterase activity and MetS.
Conclusion: We believe that the combined use of biomarkers, including GGT, arginase, paraoxonase, and arylesterase, may be useful in predicting diseases such as MetS and CVDs.
- 2,286 View
- 13 Download

- Perioperative nutritional practices and attitudes among gastrointestinal oncologic surgeons in Korea: a nation-wide survey study
- Dae Hoon Kim, Jeong-Meen Seo, Min-Gew Choi
- Ann Clin Nutr Metab 2023;15(3):81-87. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.81
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: This study aimed to investigate the current perioperative nutritional practices and attitudes among gastrointestinal (GI) oncologic surgeons in Korea. Evidence-based perioperative nutritional practices are not well-established in this field.
Methods: A nationwide survey was conducted with 24 items, targeting GI oncologic surgical faculty members from March 2022 to April 2022 through social networking service messaging and email. Whole target number was 3,421.
Results: Out of responding 161 GI surgeons, 83.9% were male and 16.1% were female, and about 49.7% were in their 40s. When asked about their hospital policies, 67.1% reported the existence of formal nutritional screening programs. However, the execution and analysis of these programs varied considerably. Most surgeons conducted preoperative nutritional screening, with albumin testing the most frequently performed. In addition, nutritional supplementation—primarily protein drinks—was given before surgery. The duration for which these supplements were used varied from ≤3 days to 4–7 days. Most respondents recognized the importance of addressing nutritional deficiencies in patients with GI tumors; however, when asked about immunonutrition, 89.4% of surgeons admitted having limited knowledge.
Conclusion: Although there is recognition of the importance of evidence-based nutrition practices in GI and oncologic surgery programs, this study reveals limited implementation of such practices. This study highlights a considerable opportunity to leverage existing positive surgeon beliefs and published data on the benefits of perioperative nutrition to enhance surgical nutrition practices and to improve patient outcomes in Korea.
- 1,428 View
- 10 Download

- Body composition assessment using bioelectrical impedance analysis and computed tomography in patients who underwent pancreatoduodenectomy in Korea: a before and after study
- Juwan Kim, Seung-seob Kim, Ho Kyoung Hwang, Chang Moo Kang, Kyung Sik Kim, Sung Hyun Kim
- Ann Clin Nutr Metab 2023;15(3):72-80. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.72
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: This study focuses on the need for standardized body composition measurements in the hepatobiliary-pancreatic field. It evaluates and compares the effectiveness of bioelectrical impedance analysis (BIA) and computed tomography (CT) scans in assessing body composition of patients undergoing pancreatoduodenectomy (PD), aiming to establish correlations among different body composition indexes.
Methods: Ninety-seven patients who underwent PD between August 2022 and March 2023, were enrolled in this study. Muscular and fatty parameters related to BIA and CT were assessed both preoperatively and on postoperative day 6. The correlation between each parameter related to muscle fat was analyzed according to the measurement modalities.
Results: There was an increase of skeletal muscle area (SMA), total muscle area, and low attenuated muscle area after surgery. Skeletal muscle mass (SMM) measured using BIA exhibited a strong correlation with the SMA and normal attenuated muscle area (NAMA) measured using CT (r=0.86, P<0.001; r=0.76, P<0.001). The trunk muscle measured using BIA demonstrated moderate to strong correlations with SMA and NAMA measured using CT (r=0.84 P<0.001; r=0.73, P<0.001). Body fat measured using BIA and total fat area (TFA) measured using CT showed strong correlations (r=0.74, P<0.001). In the postoperative analysis, a similar trend was observed (SMM vs. SMA: r=0.80, P<0.001; SMM vs. NAMA: r=0.70, P<0.001), (trunk muscle vs. SMA: r=0.79, P<0.001; trunk muscle vs. NAMA: r=0.69, P<0.001), and (body fat vs. TFA: r=0.83, P<0.001).
Conclusion: BIA, akin to CT, serves as a valuable tool for assessing body composition ratios in patients undergoing PD. -
Citations
Citations to this article as recorded by- Morphomics in esophageal cancer: Validation and association with muscular and cardiorespiratory fitness
Watson Hua-Sheng Tseng, Shu-Chun Huang, Stewart C Wang, Jules Lin, Peng Zhang, Yu-Chen Liu, Yin-Kai Chao, Chien-Hung Chiu
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Morphomics in esophageal cancer: Validation and association with muscular and cardiorespiratory fitness
- 10,719 View
- 56 Download
- 1 Crossref

Review
- Role of nutrition in wound healing and nutritional recommendations for promotion of wound healing: a narrative review
- Myoungjean Ju, Yoonhong Kim, Kyung Won Seo
- Ann Clin Nutr Metab 2023;15(3):67-71. Published online December 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.3.67
-
 Abstract
Abstract
 PDF
PDF - Purpose: Addressing both malnutrition and wound healing requires strategic intervention. However, guidelines for adequate nutrition for a variety of wounds are lacking. Based on the latest literature review, we summarize the role of nutrition in each stage of wound healing and nutritional recommendations for wound healing.
Current concept: Wounds undergo three healing phases: inflammatory, proliferative, and remodeling. The inflammatory phase involves clotting and cleaning the wound. The proliferative phase builds the wound bed through tissue growth. In the remodeling phase, collagen strength increases. Proper nutrition is crucial throughout. During inflammation, calcium, vitamin K, A, and E, zinc, and proteins are essential. In proliferation, amino acids, B vitamins, lipids, zinc, and iron play key roles. During remodeling, vitamins C and E, zinc, and water are critical for collagen synthesis and skin cell maturation. Vulnerable groups like the elderly, newborns, and obese patients need proper nutrition for skin maintenance. For pressure ulcers with malnutrition risk, recommendations are 30–35 kcal/kg/day energy, 1.25–1.5 g/kg/day protein, and 30 mL/kg water. Supplements might be added if regular meals don’t meet needs. For diabetic foot ulcers, despite common deficiencies, the 2019 International Working Group on the Diabetic Foot advises against prioritizing nutritional interventions over standard care due to limited high-quality evidence.
Conclusion: Despite limited guidelines, nutrition assessment is vital for wound evaluation. A multidisciplinary approach is key, emphasizing nutrition’s role in wound healing. Implementing nutritional interventions tailored to the wound and the individual’s nutritional status is essential. This comprehensive strategy ensures the best wound care outcomes. -
Citations
Citations to this article as recorded by- Assessment of energy requirements in patients with obesity: A narrative review
Cagney Cristancho, Kris M. Mogensen, Malcolm K. Robinson
Nutrition in Clinical Practice.2026; 41(1): 54. CrossRef - Electrospun-based nanofibers as ROS-scavenging scaffolds for accelerated wound healing: a narrative review
Mohammad Ebrahim Astaneh, Narges Fereydouni
International Journal of Polymeric Materials and Polymeric Biomaterials.2025; 74(15): 1349. CrossRef - Implementing a screening protocol for food insecure patients within a long‐term acute care hospital (LTACH): A community health needs assessment (CHNA)
Molly MacDonald, Christopher Stimson, Marti Samsel, Tina Gross
Nutrition in Clinical Practice.2025; 40(6): 1598. CrossRef - Nanoformulations Loaded with Phytochemicals for Combating Wound Infections and Promoting Wound Healing: Current Applications and Innovations
Panoraia I. Siafaka, Androulla N. Miliotou, Mehmet Evren Okur, Gökçe Karaotmarlı Güven, Ioannis D. Karantas, Neslihan Üstündağ Okur
Applied Sciences.2025; 15(10): 5413. CrossRef - Combining Topical Oxygen and Negative-Pressure Wound Therapy: New Insights from a Pilot Study on Chronic Wound Treatment
Bartosz Molasy, Mateusz Frydrych, Rafał Kuchciński, Stanisław Głuszek
Journal of Clinical Medicine.2025; 14(15): 5564. CrossRef - Undifferentiated connective tissue dysplasia and skin: what to do? Dietitian’s position
E. A. Nikitina, S. V. Orlova, T. T. Batysheva, N. V. Balashova, M. V. Alekseeva
Medical alphabet.2025; 1(19): 60. CrossRef - Nutritional Immunity in Wound Infection: Unveiling the Role of Dietary Elements in Host–Pathogen Interaction
Chaoming Chen, Xuanfan Hu, Da He, Xuemei He, Lan Shen
Food Science & Nutrition.2025;[Epub] CrossRef - Role of Nutrients and Diet in Wound Healing: The Emerging Paradigm for Effective Therapy
Aishik Banerjee, Arup Ghosh, Subhrajyoty Basu, Soumitra Sahana, Amit Kundu, Sumanta Mondal
Current Indian Science.2025;[Epub] CrossRef - Lueyang Black‐Boned Chicken and Black Bean Soup Promoting the Acute Healing of Skin Wounds, Accompanying Special Flavor Substances
Mengya Zhao, Zining Luo, Pengyan Tong, Yining Jia, Xin Yang, Jing Liu, Fangyu Long
Food Chemistry International.2025;[Epub] CrossRef - Cancer-Related Malnutrition and Oxidative Stress in Colorectal Cancer Surgery: A Narrative Review of Pathophysiology and Postoperative Outcomes
Andrii Zahorodnii, Alicja Jelska, Paulina Głuszyńska, Hady Razak Hady
Antioxidants.2025; 14(11): 1289. CrossRef - UCI Sports Nutrition Project: The Role of Nutrition in the Prevention and Management of Illnesses and Injuries in Elite Cycling
Patrick B. Wilson, David B. Pyne, Adrian Rotunno
International Journal of Sport Nutrition and Exercise Metabolism.2025; : 1. CrossRef - Clinical Impact of Nutritional Intervention on Pressure Injury Healing in a Paraplegic Patient: A Case Report
Young ran Kim, Mi young Jang, Jun ho Park
Clinical Nutrition Research.2025; 14(4): 241. CrossRef - Impact of Epigenetics, Diet, and Nutrition-Related Pathologies on Wound Healing
John Hajj, Brandon Sizemore, Kanhaiya Singh
International Journal of Molecular Sciences.2024; 25(19): 10474. CrossRef
- Assessment of energy requirements in patients with obesity: A narrative review
- 65,047 View
- 1,678 Download
- 13 Crossref

Original Articles
- Consultation pattern changes of parenteral nutrition with a multidisciplinary nutrition support team in a recently opened hospital in Korea: a retrospective cohort study
- Kyoung Won Yoon, Hyo Jin Kim, Yujeong Im, Seul Gi Nam, Joo Yeon Lee, Hyo Gee Lee, Joong-Min Park
- Ann Clin Nutr Metab 2023;15(2):57-63. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose: Parenteral nutrition (PN) is essential for the treatment of patients with malnutrition. The provision of central PN should be recommended by a nutrition support team (NST) made up of a team of experts, even in a newly established hospital. This study sought to evaluate the effectiveness of PN delivered by a multidisciplinary NST in a recently opened hospital.
Methods: This was a retrospective study of the effectiveness of a central PN recommendation pop-up message by the electronic medical record (EMR) software to prompt physicians to either calculate the required calorie and protein intake or consult with the NST. The study period was divided into pre-NST and post-NST based on the time of recruitment of NST-dedicated personnel.
Results: Patients in the 12-week pre-NST period (n=50) and 12-week post-NST period (n=74) were compared retrospectively. Baseline characteristics were not significantly different between the two groups, except for the median Acute Physiology and Chronic Health Evaluation II score (pre-NST group, 8 [interquartile range, IQR 5–15.5] vs. post-NST group, 15 [IQR 9–24], P=0.012) of the 45 patients total admitted to the intensive care unit. The percentage of patients for whom physicians requested a consultation with the NST for central PN was significantly higher in the post-NST group (52.0% vs. 75.7%, P=0.011). There was no significant difference in achievement of nutrition targets or mortality.
Conclusion: Building a multidisciplinary NST may increase awareness of nutritional status and affect the behavior of physicians in recently-opened hospitals.
- 1,918 View
- 13 Download

- Changes in mineral and vitamin profiles after bariatric surgery in Korea: a before and after study
- Jong Seob Park, Sang-Moon Han
- Ann Clin Nutr Metab 2023;15(2):51-56. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.51
-
 Abstract
Abstract
 PDF
PDF - Purpose: Bariatric surgery induces nutritional deficiencies that require long-term monitoring and supplementation. This study aimed to evaluate the status of vitamins and minerals pre-operation and 2 years post-operation and to compare the findings according to type of bariatric surgery.
Methods: The study enrolled 302 patients who underwent bariatric surgery, adjustable gastric band (AGB), sleeve gastrectomy (SG), or Roux-en-Y gastric bypass (RYGB) between 2013 and 2017 in the CHA Gangnam Medical Center and the Seoul Medical Center, Korea. Minerals and vitamin status was assessed at baseline (pre-operatively) until 2 years after bariatric surgery.
Results: Mean age was 34.1±8.3 years, 256 patients (84.8%) were female, and mean body mass index was 35.3±5.7 kg/m2. Vitamin B1, vitamin B12, and folic acid levels were significantly different at 1 and 2 years after surgery compared to baseline. Hemoglobin, hematocrit, high-density lipoprotein, iron, calcium, and magnesium levels did not differ significantly during the study period.
Conclusion: Although enrolled patients had no clinical symptoms of nutritional deficiences, several indicators related to nutrition decreased at 2 years after bariatric surgery. Despite variations in the alteration of laboratory results across three surgical interventions, namely SG, AGB, and RYGB, a consistent reduction in fasting blood sugar was observed subsequent to the surgical procedures.
- 2,831 View
- 16 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


