Scopus, KCI, KoreaMed

Search
- Page Path
- HOME > Search
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
- Ann Clin Nutr Metab 2025;17(3):181-187. Published online December 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0027
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material 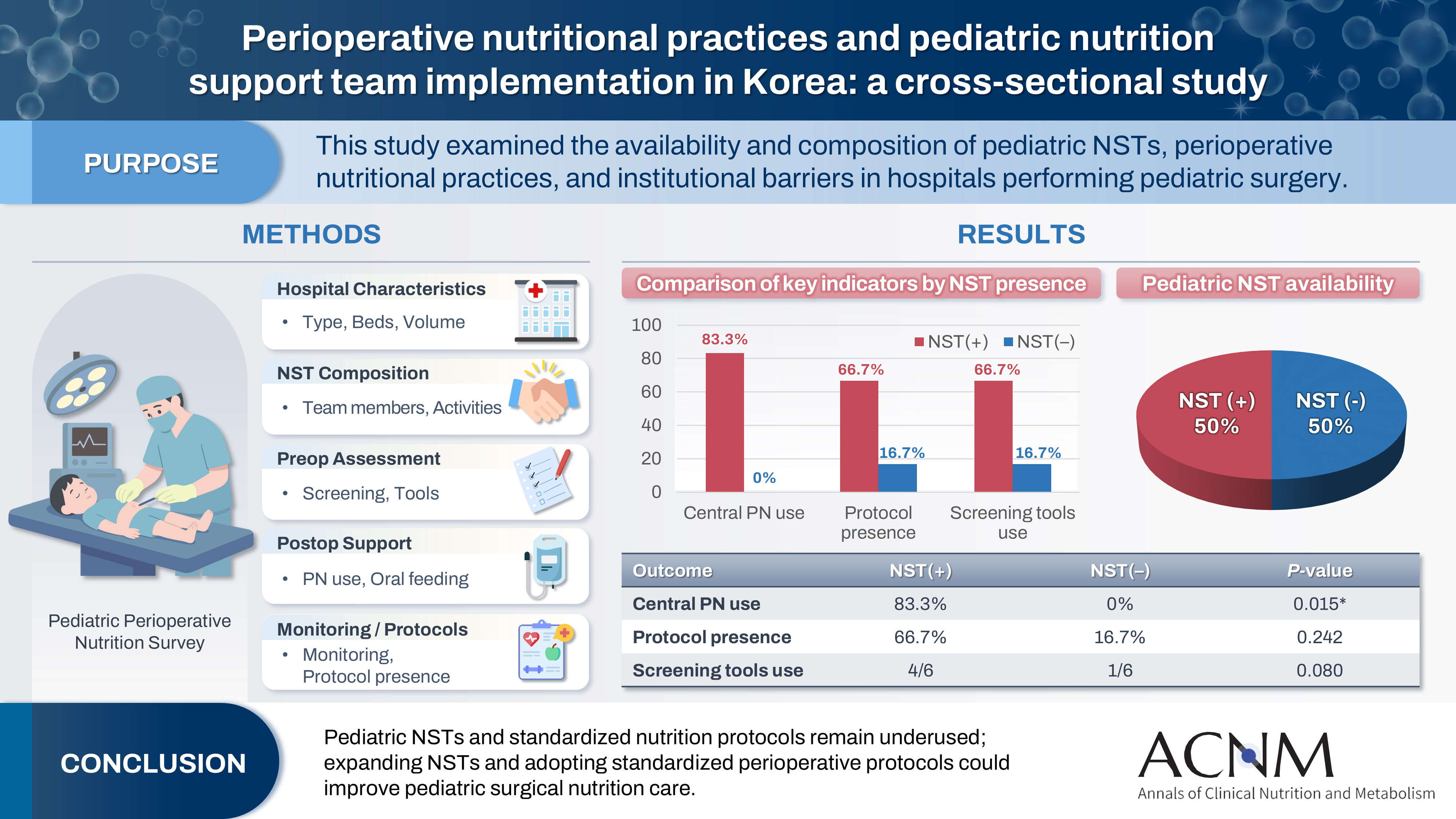
- Purpose
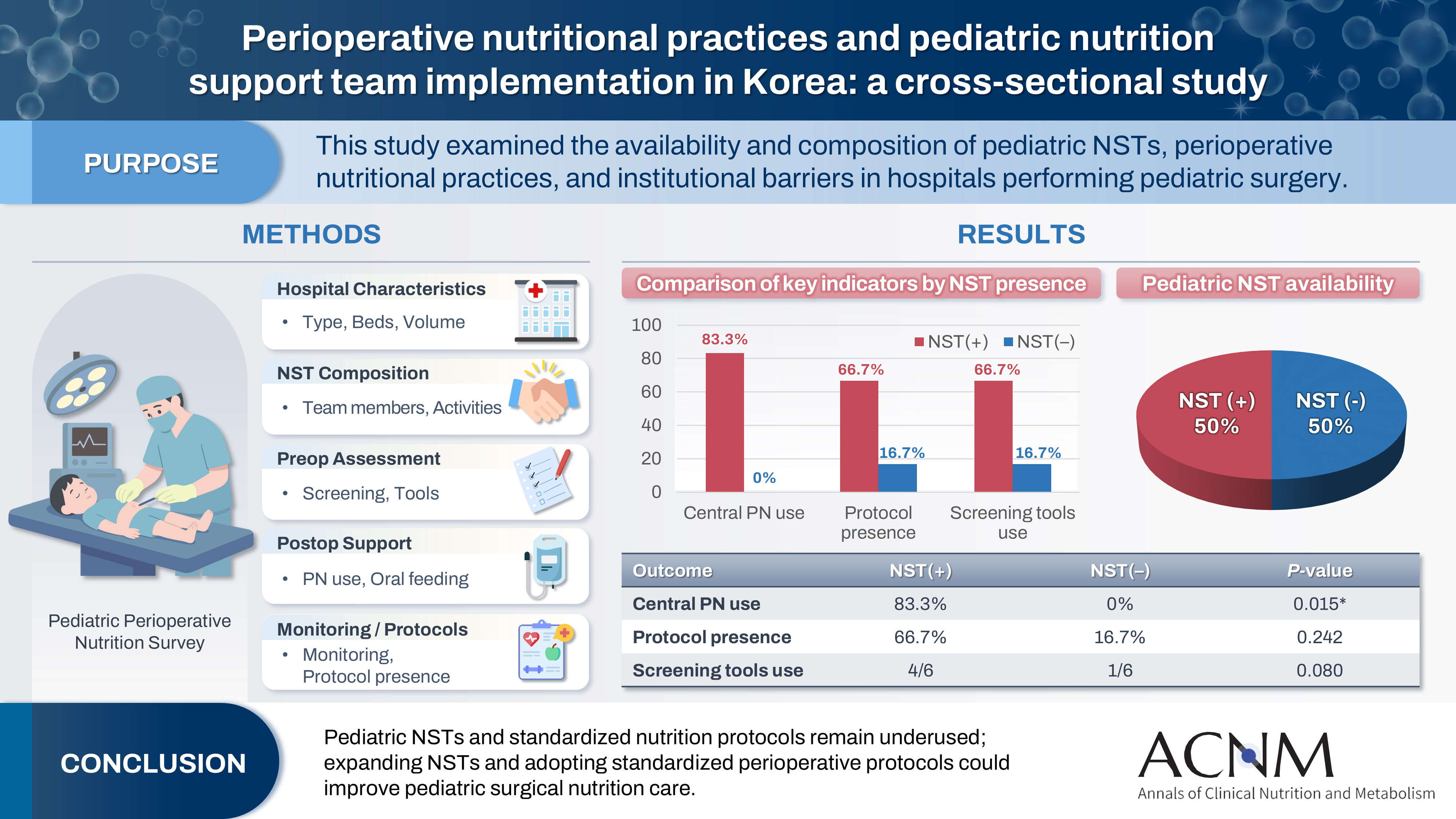
Pediatric surgical patients are vulnerable to perioperative malnutrition, yet standardized nutritional care and structured nutrition support team (NST) involvement remain inconsistent across institutions. Although multidisciplinary nutritional support has gained increasing attention, data on pediatric NST practices within surgical settings in Korea are limited. This study examined the availability and composition of pediatric NSTs, perioperative nutritional practices, and barriers in hospitals performing pediatric surgery.
Methods
A nationwide cross-sectional survey was conducted among tertiary and secondary hospitals that perform pediatric surgery in Korea. The questionnaire assessed hospital characteristics, the presence and composition of pediatric NSTs, perioperative nutritional screening and support practices, monitoring protocols.
Results
A total of 12 hospitals participated. Although all were high-capacity institutions, only half reported having a pediatric NST. Routine preoperative nutritional screening was performed in 50% of hospitals, and validated tools such as Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP) and Pediatric Yorkhill Malnutrition Score (PYMS) were used in 41.7%. Hospitals with a pediatric NST more frequently had institutional protocols for nutritional evaluation (66.7% vs. 16.7%) and were more likely to administer central venous parenteral nutrition postoperatively (83.3% vs. 0%, P=0.015). Enhanced Recovery After Surgery protocols were implemented in only two hospitals (16.7%). Major barriers to pediatric NST operation included insufficient staffing and time constraints.
Conclusion
Pediatric NSTs and standardized perioperative nutrition protocols remain underutilized in Korean surgical centers. Institutions with a pediatric NST demonstrated more structured nutritional practices. Expanding NST infrastructure and establishing standardized perioperative protocols for pediatric surgical patients may enhance the quality and consistency of nutritional care.
- 1,445 View
- 23 Download

- Improving the usability of lipid emulsions and optimizing their user-friendliness: a narrative review
- Keisuke Kubota, Natsuko Ichikawa, Kazuhiro Isoda, Misato Enomoto, Miyoko Kosugi, Mari Tanabe, Naoya Sakuraba, Sayuri Endo, Atsushi Suzuki, Masanori Hashimoto
- Ann Clin Nutr Metab 2025;17(2):104-113. Published online August 1, 2025
- DOI: https://doi.org/10.15747/ACNM.25.0015
-
 Abstract
Abstract
 PDF
PDF - Purpose
Reluctance to administer lipid emulsions to patients receiving treatment, or as recommended by a nutritional support team, often stems from various restrictions or concerns about potential adverse effects. This paper aims to discuss the appropriate clinical use of lipid emulsions to enhance both patient safety and convenience.
Current concept
We conducted a literature review to assess the importance of nutritional therapy and nutritional intervention, the advantages and disadvantages of lipid-emulsion administration, the current situation in Japan, and differences between lipid formulations. Here, we address issues regarding lipid-emulsion use, including: administration rate, drug mixing, administration in critically ill patients, and early postoperative use. Our findings suggest the following solutions to each issue: although a rate below 0.1 g/kg/hr is generally recommended, faster administration is possible if needed, depending on the case; administration via a piggy tube to basic infusion formulations is unproblematic; second- and third-generation fat emulsions are safe for critically ill patients, though soybean oil should be used with caution; and while fat emulsion administration is feasible immediately after surgery, due to endogenous energy mobilization, it is preferable to initiate administration from the third to fourth postoperative day.
Conclusion
The provisional conclusions of this study are as follows: the introduction of medium-chain triglyceride formulations and fish oil (second- and third-generation lipid emulsions), which are not yet available in Japan, is urgently needed; and individualized administration is essential due to substantial interindividual variability in lipid emulsion usage. -
Citations
Citations to this article as recorded by- Impact of soybean oil lipid emulsion on clinical outcomes in critically ill pediatric patients
Yuki Yamano, Yoshiyuki Shimizu, Yu Inata, Takeshi Hatachi, Yuri Etani
Clinical Nutrition ESPEN.2026; 72: 102907. CrossRef
- Impact of soybean oil lipid emulsion on clinical outcomes in critically ill pediatric patients
- 4,808 View
- 39 Download
- 1 Crossref

- Comparison of efficacy of enteral versus parenteral nutrition in patients after esophagectomy in Malaysia: a prospective cohort study
- Ramizah Mohd Shariff, Sze Chee Tee, Shukri Jahit Mohammad, Khei Choong Khong
- Ann Clin Nutr Metab 2025;17(1):41-49. Published online April 1, 2025
- DOI: https://doi.org/10.15747/ACNM.24.016
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF 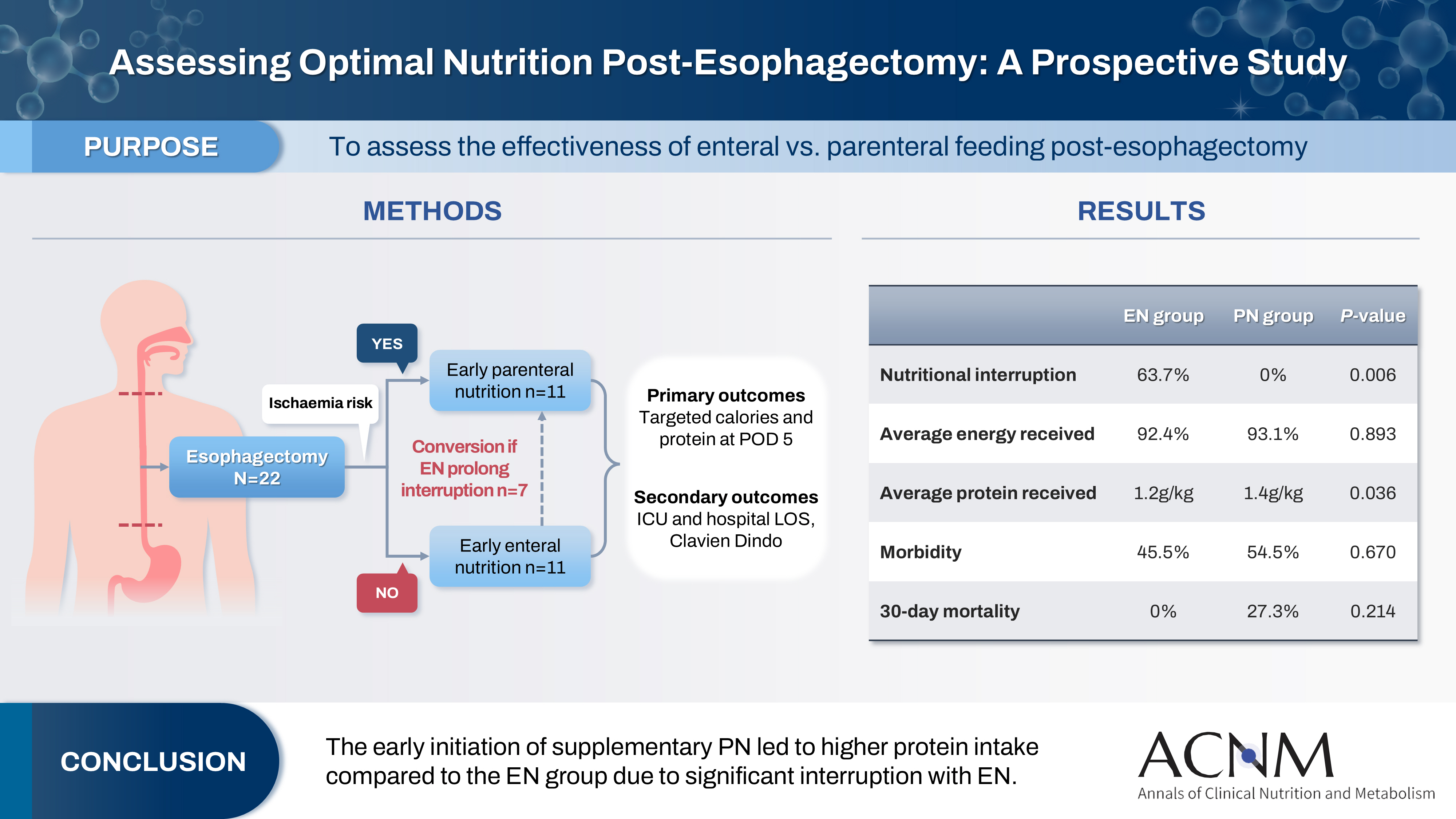
- Purpose
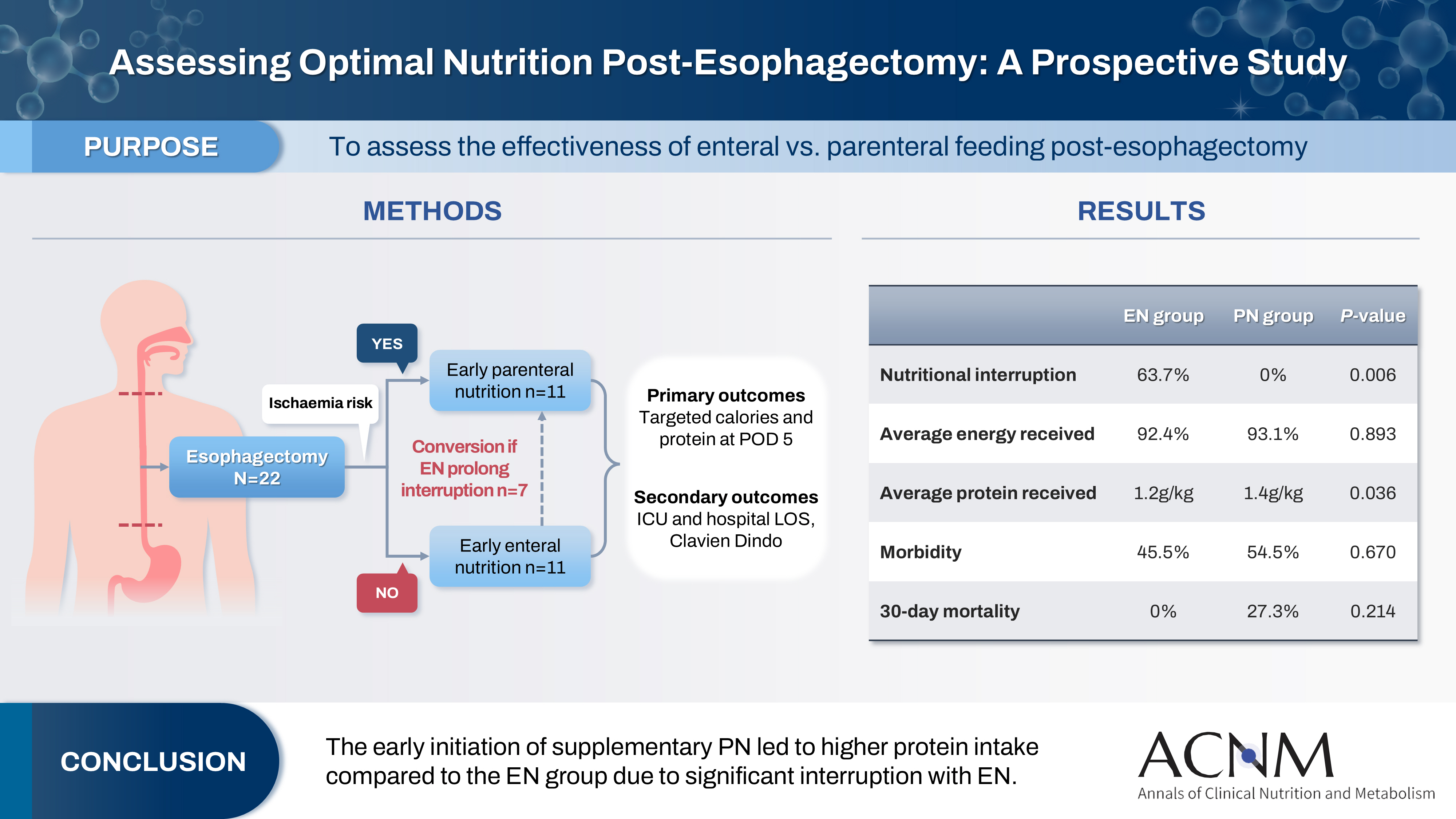
This study aims to assess the effectiveness of enteral versus parenteral feeding in patients after esophagectomy.
Methods
This a prospective cohort study of post-esophagectomy intensive care unit (ICU) patients over 12 months in the National Cancer Institute, Malaysia. Early enteral feeding followed the Enhanced Recovery After Surgery protocol, and parenteral nutrition (PN) was considered if there was a risk for conduit ischemia. It compared the effectiveness of enteral versus PN following esophagectomy, and assessed the correlations between biochemical nutritional markers and hospital lengths of stay or ventilation days.
Results
It included two cohorts receiving PN (n=11) or enteral nutrition (EN) (n=11) following elective esophagectomy. Preoperative weight, body mass index, and Subjective Global Assessment were higher in the EN group (P=0.033, P=0.021, P=0.031, respectively). Nutritional interruption occurred more frequently in the EN group (63.7%) compared to the PN group (P=0.001). Mean levels of energy and protein received were 93.1 kcal/kg and 1.4 g/kg for PN versus 92.4 kcal/kg and 1.2 g/kg for EN (P=0.893, P=0.036). The median lengths of ICU stay (P=0.688) and postoperative stay (P=0.947) between groups showed no significant difference. In addition, 30-day mortality (P=0.214) and other postoperative complications (P>0.05) were comparable in the two groups.
Conclusion
Early initiation of supplementary PN due to significant interruption in EN led to higher protein intake compared to the EN group. However, there were no significant differences in postoperative outcomes, including 30-day mortality, ICU length of stay, and ventilation days. PN ensures adequate nutritional intake, especially in terms of protein delivery, without adversely affecting postoperative recovery and clinical outcomes. -
Citations
Citations to this article as recorded by- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
Ioana Alexandra Prisacariu, Konstantinos Eleftherios Koumarelas, Konstantinos Argyriou, Alexandros Charalabopoulos, Grigorios Christodoulidis
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef
- Optimizing nutritional support in upper gastrointestinal surgery: A comprehensive review of feeding jejunostomy techniques and outcomes
- 5,566 View
- 67 Download
- 1 Crossref

- Perioperative nutritional practice of surgeons in Korea: a survey study
- Ji-Hyeon Park, Mi Ran Jung, Sang Hyun Kim, Hongbeom Kim, Gyeongsil Lee, Jae-Seok Min, Heung-Kwon Oh, Jung Hoon Bae, Yoona Chung, Dong-Seok Han, Seung Wan Ryu, The External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition
- Ann Clin Nutr Metab 2024;16(3):134-148. Published online December 1, 2024
- DOI: https://doi.org/10.15747/ACNM.2024.16.3.134
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Purpose: Enhanced recovery after surgery (ERAS) protocols advocate reduced fasting and early nutrition to improve recovery in surgical patients. However, data on ERAS implementation among Korean surgeons performing major abdominal surgeries remain sparse.
Methods: A survey conducted by the External Relation Committee of the Korean Society of Surgical Metabolism and Nutrition assessed perioperative nutritional practices among 389 Korean general surgeons from February to September 2023. The survey covered preoperative fasting, carbohydrate drinks, nasogastric tube use, postoperative dietary progression, parenteral nutrition (PN), and oral supplements, yielding 551 responses stratified by specialty.
Results: More than 80% of respondents practiced “midnight NPO (Nil Per Os)” fasting, often at the anesthesiology department’s request, while 70%–80% reported no use of preoperative carbohydrate drinks. Most surgeons began dietary progression with water on postoperative day one, advancing to a liquid or soft diet by day two. PN was routinely prescribed by 49% of respondents, with a common dosage of 1,000–1,500 kcal/d. Oral supplements were selectively provided, with 21% of surgeons prescribing them universally.
Conclusion: The results reveal significant variability in perioperative nutrition practices across Korean surgical specialties, with many adhering to traditional practices despite ERAS guidelines. These findings highlight a need for standardized guidelines in Korea to optimize perioperative nutritional support and improve patient recovery outcomes following major abdominal surgeries. -
Citations
Citations to this article as recorded by- Development of the Korean enhanced recovery after surgery audit program
Soo-Hyuk Yoon, Jae-Woo Ju, Ho-Jin Lee, Jeesun Kim, Min Jung Kim, Ji Won Park, Do Joong Park, Seung Yong Jeong
Scientific Reports.2025;[Epub] CrossRef - Perioperative nutrition practices in gastrointestinal cancer surgery: A nationwide survey among German surgical departments
Rahel Maria Strobel, Katharina Beyer, Johannes Christian Lauscher, Marc Martignoni, Christoph Reißfelder, Tim Vilz, Arved Weimann, Maria Wobith
Langenbeck's Archives of Surgery.2025;[Epub] CrossRef
- Development of the Korean enhanced recovery after surgery audit program
- 6,751 View
- 88 Download
- 2 Crossref

- Consultation pattern changes of parenteral nutrition with a multidisciplinary nutrition support team in a recently opened hospital in Korea: a retrospective cohort study
- Kyoung Won Yoon, Hyo Jin Kim, Yujeong Im, Seul Gi Nam, Joo Yeon Lee, Hyo Gee Lee, Joong-Min Park
- Ann Clin Nutr Metab 2023;15(2):57-63. Published online August 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.2.57
-
 Abstract
Abstract
 PDF
PDF - Purpose: Parenteral nutrition (PN) is essential for the treatment of patients with malnutrition. The provision of central PN should be recommended by a nutrition support team (NST) made up of a team of experts, even in a newly established hospital. This study sought to evaluate the effectiveness of PN delivered by a multidisciplinary NST in a recently opened hospital.
Methods: This was a retrospective study of the effectiveness of a central PN recommendation pop-up message by the electronic medical record (EMR) software to prompt physicians to either calculate the required calorie and protein intake or consult with the NST. The study period was divided into pre-NST and post-NST based on the time of recruitment of NST-dedicated personnel.
Results: Patients in the 12-week pre-NST period (n=50) and 12-week post-NST period (n=74) were compared retrospectively. Baseline characteristics were not significantly different between the two groups, except for the median Acute Physiology and Chronic Health Evaluation II score (pre-NST group, 8 [interquartile range, IQR 5–15.5] vs. post-NST group, 15 [IQR 9–24], P=0.012) of the 45 patients total admitted to the intensive care unit. The percentage of patients for whom physicians requested a consultation with the NST for central PN was significantly higher in the post-NST group (52.0% vs. 75.7%, P=0.011). There was no significant difference in achievement of nutrition targets or mortality.
Conclusion: Building a multidisciplinary NST may increase awareness of nutritional status and affect the behavior of physicians in recently-opened hospitals.
- 2,070 View
- 13 Download

- Efficacy of monounsaturated fatty acids in reducing risk of the cardiovascular diseases, cancer, inflammation, and insulin resistance: a narrative review
- Ki Hyun Kim, Yoonhong Kim, Kyung Won Seo
- Ann Clin Nutr Metab 2023;15(1):2-7. Published online April 1, 2023
- DOI: https://doi.org/10.15747/ACNM.2023.15.1.2
-
 Abstract
Abstract
 PDF
PDF - Purpose: The purpose of this review is to explore the potential benefits of monounsaturated fatty acids (MUFAs), specifically those found in olive oil, on weight loss, cardiovascular disease, cancer, inflammation, and insulin resistance. Additionally, this review examines the use of olive oil–based intravenous lipid emulsions (ILEs) in providing parenteral nutrition to patients with diverse needs.
Current concept: MUFAs, found in olive oil, nuts, and some animal foods, have been found to have numerous health benefits. A diet high in MUFAs can aid in weight loss and reduce the risk of cardiovascular disease. Olive oil, in particular, has been linked to a lower risk of cancer, inflammation, and insulin resistance. In addition, olive oil–based ILEs have been utilized for over two decades and are well tolerated by patients requiring parenteral nutrition.
Conclusion: A diet rich in MUFAs, specifically from olive oil, can provide numerous health benefits, including weight loss and reducing the risk of cardiovascular disease, cancer, inflammation, and insulin resistance. Additionally, olive oil–based ILEs have been shown to effectively provide nutrients to diverse populations requiring parenteral nutrition and have demonstrated the ability to preserve immune function and induce less lipid peroxidation than other ILEs. Further research is needed to fully understand the potential benefits of MUFAs and olive oil-based ILEs, but current evidence suggests that they may be a valuable addition to a healthy diet and medical treatment. -
Citations
Citations to this article as recorded by- Effects of daily extra virgin olive oil consumption on biomarkers of inflammation and oxidative stress: a systematic review and meta-analysis
Jéssica Vidal Damasceno, Anderson Garcez, Andressa Anelo Alves, Isabella Rosa da Mata, Simone Morelo Dal Bosco, Juliano Garavaglia
Critical Reviews in Food Science and Nutrition.2026; 66(2): 392. CrossRef - Applying Wild Mistol Fruits (Sarcomphalus Mistol) from the Paraguayan Chaco as Value-Added Food Ingredients
Villalba R., Belotto J., Coronel E., Carvajal M., Recalde C., Caballero S., Friesen A., Mereles L.
Plant Foods for Human Nutrition.2026;[Epub] CrossRef - Multi-Omics Integration Reveals Key Genes, Metabolites and Pathways Underlying Meat Quality and Intramuscular Fat Deposition Differences Between Tibetan Pigs and Duroc × Tibetan Crossbred Pigs
Junda Wu, Qiuyan Huang, Baohong Li, Zixiao Qu, Xinming Li, Fei Li, Haiyun Xin, Jie Wu, Chuanhuo Hu, Sen Lin, Xiangxing Zhu, Dongsheng Tang, Chuang Meng, Zongliang Du, Erwei Zuo, Fanming Meng, Sutian Wang
Animals.2026; 16(2): 214. CrossRef - The MetaboHealth Score Enhances Insulin Resistance Metabotyping for Targeted Fat Loss: The PERSON Study
Jordi Morwani‐Mangnani, Fatih A. Bogaards, Alexander Umanets, Gabby B. Hul, Anouk Gijbels, Gijs H. Goossens, Joris Deelen, Marian Beekman, Lydia Afman, Ellen E. Blaak, P. Eline Slagboom
Obesity.2026;[Epub] CrossRef - Video and Text‐Based Supplemental Health Information and Consumer Willingness to Pay for Nutrient‐Enhanced Eggs
Edeoba W. Edobor, Michael J. Best, Anita R. Best, Ondulla T. Toomer
Agribusiness.2026;[Epub] CrossRef - The impact of Lactiplantibacillus plantarum on the cream composition: Insight into changes of vitamin D3 content and fatty acid composition
Tetiana Dyrda-Terniuk, Viorica Railean, Aleksandra Bogumiła Florkiewicz, Justyna Walczak-Skierska, Mateusz Kolankowski, Joanna Rudnicka, Dorota Białczak, Paweł Pomastowski
International Dairy Journal.2025; 161: 106118. CrossRef - Palmitoleic and oleic fatty acids as biomarkers for coronary heart disease: A predictive model
Guangzhou Wang, Lin Zhou, Zhengfang Wang, Asmaa Ali, Liang Wu
Irish Journal of Medical Science (1971 -).2025; 194(1): 59. CrossRef - Macrophages: their role in immunity and their relationship with fatty acids in health and disease
Mayte Rueda-Munguía, Luis Alberto Luévano-Martínez, Gerardo García-Rivas, Elena Cristina Castillo, Omar Lozano
Frontiers in Immunology.2025;[Epub] CrossRef - Evaluation of the Nutritional Value of Prunus dulcis Blossoms and the Antioxidant Compounds of Their Extracted Oil Using Green Extraction Method
Theodoros Chatzimitakos, Vassilis Athanasiadis, Konstantina Kotsou, Ioannis Makrygiannis, Eleni Bozinou, Stavros I. Lalas
Applied Sciences.2024; 14(5): 2001. CrossRef - Oleic Acid and Succinic Acid: A Potent Nutritional Supplement in Improving Hepatic Glycaemic Control in Type 2 Diabetic Sprague–Dawley Rats
Kemmoy G. Lattibeaudiere, Ruby Lisa Alexander-Lindo, Mozaniel Oliveira
Advances in Pharmacological and Pharmaceutical Sciences.2024;[Epub] CrossRef
- Effects of daily extra virgin olive oil consumption on biomarkers of inflammation and oxidative stress: a systematic review and meta-analysis
- 33,190 View
- 96 Download
- 10 Crossref

- Development of Wernicke’s Encephalopathy during Total Parenteral Nutrition Therapy without Additional Multivitamin Supplementation in a Patient with Intestinal Obstruction: A Case Report
- Cheong Ah Oh
- Ann Clin Nutr Metab 2022;14(2):93-96. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.93
-
 Abstract
Abstract
 PDF
PDF - Wernicke’s encephalopathy (WE) is a serious neurological disorder that can be fatal if not properly treated. In this current paper, I present the case of a 51-year-old male with a perivesical fistula between a presacral abscess and the rectus abdominis muscle. He received total parenteral nutrition therapy during a fasting period because of small bowel obstruction and later developed WE. The patient’s WE-related symptoms improved following rapid treatment with high doses of thiamine.
- 3,550 View
- 35 Download

- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
- Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
- Ann Clin Nutr Metab 2022;14(2):66-71. Published online December 1, 2022
- DOI: https://doi.org/10.15747/ACNM.2022.14.2.66
-
 Abstract
Abstract
 PDF
PDF - Purpose: Timely enteral nutrition (EN) is important in critically ill patients. However, use of EN with critically ill surgical patients has many limitations. This study aimed to analyze the current status of EN in surgical intensive care units (ICUs) in South Korea.
Materials and Methods: A multicenter, prospective, observational study was conducted on patients who received EN in surgical ICUs at four university hospitals between August 2021 and January 2022.
Results: This study included 125 patients. The mean time to start EN after admission to the surgical ICU was 6.2±4.6 days. EN was provided to 34 (27.2%) patients within 3 days after ICU admission. At 15.7±15.9 days, the target caloric requirement was achieved by 74 (59.2%) patients through EN alone. Furthermore, 104 (83.2%) patients received supplemental parenteral nutrition after a mean of 3.5±2.1 days. Only one of the four hospitals regularly used enteral feeding tubes and post-pyloric feeding tubes.
Conclusion: Establishing EN guidelines for critically ill surgical patients and setting an appropriate insurance fee for EN-related devices, such as the feeding pump and enteral feeding tube, are necessary.
- 4,011 View
- 33 Download

- Characteristics and Practice of Parenteral Nutrition in Hospitalized Adult Cancer Patients in Korea
- Hyo Jung Park, You Min Sohn, Jee Eun Chung, Jung Tae Kim, Jin A Yang, Hye Jung Bae, Ye Won Sung, Sun Hwa Kim,Ji Yoon Cho, Kyung Mi Jung, Hee Kyung Bae
- J Clin Nutr 2020;12(2):34-40. Published online December 31, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.2.34
-
 Abstract
Abstract
 PDF
PDF - Purpose: There have been no clinical studies on the characteristics of parenteral nutrition (PN) for adult cancer inpatients in South Korea. The published evidence describing modern PN practices in these patients is also extremely limited. Therefore in this retrospective multicenter cross-sectional study, we aimed to investigate the PN support practice in hospitalized adult cancer patients.
Methods: The study included adult cancer patients hospitalized in nine hospitals in South Korea and received PN, during the period from August 1st, 2017 to October 30th, 2017. We evaluated the relevant hospital-based PN practices in this group.
Results: Among the 11,580 inpatient admissions during this period, 759 cancer patients received PN (6.6%). The majority of enrolled patients (97.2%) used commercially available PN and 71.2% of these used peripheral PN formulations. The average in-hospital PN duration was 16.1±19.9 days. Patients received only 65.4±25.4% calories of the recommended target calories. The in-hospital mortality of enrolled patients was 26.1%.
Conclusion: We conclude that commercial PN is the most common form of PN administered to hospitalized adult cancer patients and the overall in-hospital mortality in the patients using PN is higher in South Korea compared to other countries.
- 987 View
- 6 Download

- The Influence of Pediatric Nutrition Support Team on Hospitalized Pediatric Patients Receiving Parenteral Nutrition
- Sijin Baek, Juhyun Rho, Hyung Wook Namgung, Eunsook Lee, Euni Lee, Hye Ran Yang
- J Clin Nutr 2020;12(1):7-13. Published online June 30, 2020
- DOI: https://doi.org/10.15747/jcn.2020.12.1.7
-
 Abstract
Abstract
 PDF
PDF - Purpose: Malnutrition is a common problem in hospitalized patients that can increase the risk of complications, including infections and length of hospitalization. Appropriate nutritional support is important, particularly in pediatric patients, because growth and development are closely related to the nutritional supply. This study examined the status of nutritional support for pediatric patients in general wards to determine if interventions of the pediatric nutrition support team (pNST) contribute to appropriate nutritional support and help improve their nutritional status.
Methods: Between July 2016 and June 2017, all pediatric inpatients who received parenteral nutrition support at the Seoul National University Bundang Hospital were recruited and divided into the NST group and non-NST group according to the activities of pNST. The nutritional status was assessed in all subjects, and the calories and proteins delivered through nutritional support in each group were calculated and then compared with the recommended requirements in pediatric patients.
Results: The number of patients recruited was 174: 100 (57.5%) in the NST group and 74 (42.5%) in the non-NST group. Significantly more calories and protein were supplied in the NST group than the non-NST group in hospitalized children aged between four and 17 years (P<0.05). In the non-NST group, the amounts of calories supplied were insufficient compared to the recommended requirements. The proportion of patients supplied with the appropriate number of calories was 60.0% in the NST group and 20.0% in the non-NST group (P<0.001), and the proportion of cases supplied with the appropriate amount of protein was 87.0% in the NST group and 62.2% in the non-NST group (P<0.001).
Conclusion: Interventions of the pediatric nutrition support team contributed to the sufficient supply of calories and protein and the improvement of clinical outcomes in hospitalized children on parenteral nutrition therapy. -
Citations
Citations to this article as recorded by- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
Dayoung Ko, Honam Hwang, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Clin Nutr Metab.2025; 17(3): 181. CrossRef
- Perioperative nutritional practices and pediatric nutrition support team implementation in Korea: a cross-sectional study
- 870 View
- 6 Download
- 1 Crossref

- Analysis of Compliance and Clinical Outcomes by Expanding Physician’s Departments in Pediatric Nutrition Support Team
- Hae Won Lee, Min Jae Jung, Ji Eun Park, Hee Kwon, Jae Song Kim, Hong Go, Eun Sun Son
- J Clin Nutr 2019;11(2):42-51. Published online December 31, 2019
- DOI: https://doi.org/10.15747/jcn.2019.11.2.42
-
 Abstract
Abstract
 PDF
PDF Purpose:
Malnutrition in hospitalized children has an impact on growth, morbidity, and mortality. For this reason, the implementation of pediatric nutrition support team (PNST) has been suggested. On April 2017, in Severance Hospital, more PNST physician’s departments participated in PNST, and a PNST physician assigning system was changed to be the same departments with the attending physician and PNST physician. This study performed a comparative analysis of the compliance and clinical outcomes after expanding the participation of the PNST physician’s department.
Methods:
Pediatric patients, who were referred to a PNST consultant, were divided into two groups: an unmatched group (different departments with the attending physician and PNST physician [154 patients, 233 consultations from May 2016 to October 2016]), and a matched group (same departments with the attending physician and PNST physician [169 patients, 302 consultations from May 2017 to October 2017]). The PNST compliance and clinical outcomes, such as the total delivered/required caloric and protein ratio, % ideal body weight (%IBW), serum total protein, and serum albumin, in the two groups were compared.
Results:
The compliance was significantly higher in the matched group than the unmatched group (63.4% vs. 47.3%, P=0.005). Although there was no significant difference, the total delivered/required caloric and protein ratio, and %IBW in the matched group tended to increase. The serum total protein (0.7±0.7 g/dL vs. –0.4±1.3 g/dL, P=0.004) and serum albumin (0.5±0.5 g/dL vs. –0.1±0.6 g/dL, P=0.003) were significantly higher in the matched group.
Conclusion:
After expanding the physician’s departments in PNST, the compliance was significantly higher in the matched group and the clinical outcomes tended to better. The physician assigning system to be matched with the departments between the attending physician and the PNST physician may help increase the compliance of NST consultations, resulting in an improvement of the patient’s clinical outcomes.
- 756 View
- 0 Download

- Nutritional Support for Cancer Patients
- Yoontaek Lee
- Surg Metab Nutr 2019;10(2):27-31. Published online December 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.2.27
-
 Abstract
Abstract
 PDF
PDF Cancers are the leading cause of death worldwide, and various modalities of cancer treatment, such as surgery, radiation therapy, and pharmacological therapies, have been applied. Malnutrition and a loss of muscle mass are encountered frequently in cancer patients and adversely affect the clinical outcomes. Therefore, screening for, monitoring, and treating malnutrition are important procedures in treating cancer patients. This paper reviews the guidelines as well as comparative studies describing the nutritional support provided to cancer patients and describes the evidence-based guidelines and recommendation for each topic.
- 1,602 View
- 18 Download

- Nutrition Support for Pediatric Surgical Patients
- Jun Beom Park
- Surg Metab Nutr 2019;10(1):9-14. Published online June 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.1.9
-
 Abstract
Abstract
 PDF
PDF Pediatric patients have characteristics such as a low capacity for storing energy/nutrients and high energy metabolism as compared those of adults. Because of the inherent characteristics that they are continually growing, supplying both rapid and adequate nutrition is of the utmost importance. In the case of children undergoing surgery (and particularly gastrointestinal surgery), there is a high possibility of a restricted supply of nutrition, and so active intervention to supply sufficient nutrition must be carried out. Of course, enteral nutrition is preferred, but continuous monitoring of nutrition is of paramount importance; thus, parenteral nutrition should be provided when necessary. Nutritional support requires continuous monitoring when and if complications arise. The complications of parenteral nutrition have yet to be overcome, so further research on this topic is certainly warranted.
- 804 View
- 6 Download

- Physiological Change of Serum Bilirubin Level by ω-3 Enriched Parenteral Nutrition Versus ω-3 Free Parenteral Nutrition in Healthy Male Subjects
- Mi Rin Lee, Min-Gul Kim, Jae Do Yang, Hong Pil Hwang, Yunjeong Kim, Ji-Young Jeon, Sungwoo Ahn, Hee Chul Yu
- Surg Metab Nutr 2019;10(1):20-26. Published online June 30, 2019
- DOI: https://doi.org/10.18858/smn.2019.10.1.20
-
 Abstract
Abstract
 PDF
PDF Purpose:
Bilirubin is a biomarker for the diagnosis of liver diseases or bile duct dysfunction. This study assessed the physiological changes in the blood bilirubin level infusing ω-3 enriched parenteral nutrition (PN) and ω-3 free PN in healthy male subjects.
Materials and Methods:
This study was a randomized, open-label, two-treatment, two-way crossover trial. Sixteen subjects were assigned randomly to one of two sequences of the two treatments: ω-3 enriched PN or ω-3 free PN was infused via aperipheral venous catheter for six hours at 3 mL/kg/h. Blood samples were collected every one hour from 0 to 12 hours after starting an intravenous infusion for bilirubin concentrations. The total bilirubin and direct bilirubin concentrations in the blood were analyzed using an enzymatic method.
Results:
The bilirubin concentration in the blood was reduced while infusing the ω-3 enriched PN and ω-3 free PN. When it stopped infusing, the bilirubin concentration was recovered. A similar pattern was observed, but there was a further decline and recovery in ω-3 free PN.
Conclusion:
When ω-3 enriched PN and ω-3 free PN are infused in healthy male subjects, the blood bilirubin level decreasedand there is no difference between the two groups.
- 1,907 View
- 6 Download

- Nutritional Therapy Related Complications in Hospitalized Adult Patients: A Korean Multicenter Trial
- Eun-Mi Seol, Kye Sook Kwon, Jeong Goo Kim, Jung-Tae Kim, Jihoon Kim, Sun-Mi Moon, Do Joong Park, Jung Hyun Park, Je Hoon Park, Ji Young Park, Jung-Min Bae, Seung Wan Ryu, Ji-Young Sul, Dong Woo Shin, Cheung Soo Shin, Byung Kyu Ahn, Soo Min Ahn, Hee Chul Yu, Gil Jae Lee, Sanghoon Lee, A Ran Lee, Jae Young Jang, Hyun Jeong Jeon, Sung Min Jung, Sung-Sik Han, Suk-Kyung Hong, Sun-Hwi Hwang, Yunhee Choi, Hyuk-Joon Lee
- J Clin Nutr 2019;11(1):12-22. Published online June 30, 2019
- DOI: https://doi.org/10.15747/jcn.2019.11.1.12
-
 Abstract
Abstract
 PDF
PDF Purpose:
Nutritional therapy (NT), such as enteral nutrition (EN) or parenteral nutrition (PN), is essential for the malnourished patients. Although the complications related to NT has been well described, multicenter data on symptoms in the patients with receiving NT during hospitalization are still lacking.
Methods:
Nutrition support team (NST) consultations, on which NT-related complications were described, were collected retrospectively for one year. The inclusion criteria were patients who were (1) older than 18 years, (2) hospitalized, and (3) receiving EN or PN at the time of NST consultation. The patients’ demographics (age, sex, body mass index [BMI]), type of NT and type of complication were collected. To compare the severity of each complication, the intensive care unit (ICU) admission, hospital stay, and type of discharge were also collected.
Results:
A total of 14,600 NT-related complications were collected from 13,418 cases from 27 hospitals in Korea. The mean age and BMI were 65.4 years and 21.8 kg/m2. The complications according to the type of NT, calorie deficiency (32.4%, n=1,229) and diarrhea (21.6%, n=820) were most common in EN. Similarly, calorie deficiency (56.8%, n=4,030) and GI problem except for diarrhea (8.6%, n=611) were most common in PN. Regarding the clinical outcomes, 18.7% (n=2,158) finally expired, 58.1% (n=7,027) were admitted to ICU, and the mean hospital days after NT-related complication were 31.3 days. Volume overload (odds ratio [OR]=3.48) and renal abnormality (OR=2.50) were closely associated with hospital death; hyperammonemia (OR=3.09) and renal abnormality (OR=2.77) were associated with ICU admission; “micronutrient and vitamin deficiency” (geometric mean [GM]=2.23) and volume overload (GM=1.61) were associated with a longer hospital stay.
Conclusion:
NT may induce or be associated with several complications, and some of them may seriously affect the patient’s outcome. NST personnel in each hospital should be aware of each problem during nutritional support.
-
Citations
Citations to this article as recorded by- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
Chan-Hee Park, Hak-Jae Lee, Suk-Kyung Hong, Yang-Hee Jun, Jeong-Woo Lee, Nak-Jun Choi, Kyu-Hyouck Kyoung
Annals of Clinical Nutrition and Metabolism.2022; 14(2): 66. CrossRef - Pathophysiology and protective approaches of gut injury in critical illness
Chang Yeon Jung, Jung Min Bae
Yeungnam University Journal of Medicine.2021; 38(1): 27. CrossRef - Nutrition Support Team Reconsultation During Nutrition Therapy in Korea
Eun‐Mi Seol, Yun‐Suhk Suh, Dal Lae Ju, Hye Jung Bae, Eunjung Kim, Hyuk‐Joon Lee
Journal of Parenteral and Enteral Nutrition.2021; 45(2): 357. CrossRef
- Provision of Enteral Nutrition in the Surgical Intensive Care Unit: A Multicenter Prospective Observational Study
- 1,268 View
- 8 Download
- 3 Crossref

- In-line Filtration in Parenteral Nutrition
- Eunjung Kim, Eun-Mi Seol
- J Clin Nutr 2019;11(1):1-4. Published online June 30, 2019
- DOI: https://doi.org/10.15747/jcn.2019.11.1.1
-
 Abstract
Abstract
 PDF
PDF Metabolic abnormalities and catheter-related infections are common complications of parenteral nutrition (PN). Particulate contamination is a catheter-related complication can occur when administering PN: mixing the electrolytes, trace elements, vitamins into the PN, or puncturing a rubber stopper at the PN formulation. In addition, the aggregation of the components of the PN solution by a drug incompatibility reaction could be related to particulate contamination. PN contaminated with precipitates, insoluble particles, and bacteria was reported as the cause of the death of a patient. The Food and Drug Administration recommended that the filters be used during PN administration. In-line filters can retain the bacteria and insoluble particles in PN solutions, and prevent their infusion into the patient. Therefore, in-line filters are recommended to prevent catheter-related complications that can occur during PN infusion. A 0.2
µ filter for lipid-free PN and a 1.2µ filter for lipid-containing PN solutions can be used. On the other hand, when a filter is applied, the infusion rate can decrease and the economic burden will increase for patients requiring long-term PN. In addition, small particles, such as viruses, polymers, and proteins cannot be filtered out completely. In conclusion, in-line filers are recommended to prevent catheter-related complications that can occur during PN administration, but there are no international standardized guidelines. Therefore, standardized guidelines will be needed based on evidence accompanied by clinical trials. In addition, in-line filter applications should be considered in the clinical field depending on the patient’s condition.
- 1,098 View
- 17 Download

- Multidisciplinary Intestinal Rehabilitation for Short Bowel Syndrome in Adults: Results in a Korean Intestinal Rehabilitation Team
- Sojeong Yoon, Sanghoon Lee, Hyo Jung Park, Hyun-Jung Kim, Jihye Yoon, Ja-Kyung Min, Jeong-Meen Seo
- J Clin Nutr 2018;10(2):45-50. Published online December 31, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.2.45
-
 Abstract
Abstract
 PDF
PDF Purpose:
Intense multidisciplinary team effort is required for the intestinal rehabilitation of patients afflicted with the short bowel syndrome (SBS). These include enteral and parenteral nutrition (PN) support, monitoring of complications related to treatment, and considering further medical or surgical options for intestinal adaptation.
Methods:
In the Intestinal Rehabilitation Team (IRT) at the Samsung Medical Center, we have experienced 20 cases of adult SBS requiring multidisciplinary intestinal rehabilitation. This study is a retrospective review of the collected medical records.
Results:
Of the 20 subjects treated, 12 patients were male and 8 patients were female. At the time of referral to the IRT, the mean age was 51.5 years, and the mean body weight was 50.1 kg, which was 90% of the usual body weight. The diseases or operative managements preceding massive bowel resection were malignancy in 11 cases, cardiac surgery in 2 cases, trauma in 2 cases and one case, each of tuberculosis, corrosive esophagitis, atrial fibrillation, simultaneous pancreas and kidney transplantation, and perforated appendicitis. Of these, there were 14 survivals and 6 mortalities. The fatalities were attributed to progression of disease, intestinal failure-associated liver disease, and sepsis (unrelated to intestinal failure) (2 cases each). Among the 14 surviving patients, 8 patients have been weaned off PN, whereas 6 are still dependent on PN (mean PN dependence 36%).
Conclusion:
This paper reports the results of multidisciplinary intestinal rehabilitation of adult short bowel patients treated at the Samsung Medical Center. Further studies are required to improve survival and enteral tolerance of these patients.
-
Citations
Citations to this article as recorded by- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
Yunhyung Kim, Yeon Hee Kim, Jae Sim Jeong
Journal of Korean Association for Qualitative Research.2024; 9(1): 1. CrossRef - Intestinal Rehabilitation Program for Adult Patients with Intestinal Failure: A 20-Year Analysis of Outcomes in the Single-Center Experience at a Tertiary Hospital
Kyoung Moo Im, Jae Hee Chung
Digestive Diseases and Sciences.2024; 69(5): 1770. CrossRef - Vitamin D Deficiency is Prevalent in Short Bowel Syndrome Patients on Long-Term Parenteral Nutrition Support
SungHyo An, Sanghoon Lee, Hyun-Jung Kim, Hyo Jung Park, Jeong-Meen Seo
Journal of Clinical Nutrition.2021; 13(1): 12. CrossRef - Multidisciplinary Intestinal Rehabilitation in Children: Results from a Korean Intestinal Rehabilitation Team
Cheolgu Lee, Sanghoon Lee, Hyo Jung Park, Hyun-Jung Kim, Ja-Kyung Min, Jeong-Meen Seo
Advances in Pediatric Surgery.2020; 26(2): 61. CrossRef
- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
- 1,223 View
- 1 Download
- 4 Crossref

- Parenteral Nutrition in Hospitalized Adult Patients in South Korea
- Miyoung Ock, Sera Lee, Hyunah Kim
- J Clin Nutr 2018;10(2):38-44. Published online December 31, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.2.38
-
 Abstract
Abstract
 PDF
PDF Purpose:
Parenteral nutrition (PN) is known to provide therapeutic beneficial improvements in malnourished patients for whom enteral nutrition is not feasible. The objective of this study was to investigate the current clinical characteristics and utilization of PN in Korea.
Methods:
We analyzed the Health Insurance Review Agency National Inpatients Sample database from 2014 to 2016, which included 13% of all hospitalized patients in Korea. Adult patients aged 20 years or older and receiving premixed multi-chamber bag containing PN were included for this study. Patient characteristics, admission type, primary diagnosis, and hospital demographics were evaluated. SAS version 9.4 was used for data analysis.
Results:
From 2014 to 2016, 149,504 patients received premixed PN, with 226,281 PN prescriptions being written. The mean patient age was 65.0 years, and 81,876 patients (54.8%) were male. Premixed 3-chamber bag and 2-chamber bag PN solutions were utilized in 131,808 (88.2%) and 32,033 (21.4%) patients, respectively. The number of patients hospitalized through the emergency department were 70,693 (47.3%), whereas 43,125 patients (28.8%) were administered PN in intensive care units. In the adult PN patients, the highest primary diagnosis was malignant neoplasm of the stomach (8,911, 6.0%), followed by organism unspecified pneumonia (7,008, 4.7%), and gastroenteritis and colitis of unspecified origin (6,381, 4.3%). Overall, 34% of adult PN patients were diagnosed with malignancies, the most common being neoplasm of the stomach (17.7%), neoplasm of bronchus/lung (11.2%), neoplasm of colon (11.1%), and neoplasm of liver/intrahepatic bile ducts (10.0%). PN solutions were most frequently administered in the metropolitan area (55.0%) and in hospitals with more than 1,000 beds (23.6%).
Conclusion:
PN was commonly administered in older patients, with primary diagnosis of malignancy in a significant number of cases. This study is the first large-scale description of PN-prescribing patterns in real-world clinical practice in South Korea.
- 1,005 View
- 8 Download

- Effect of Total Parenteral Nutrition Therapy in Palliative Gastrojejunostomy Status Patients
- Yung Kil Kim, Geum Jong Song, Tae Sung Ahn, Myoung Won Son, Sun Wook Han, Joon-Hwan Song, Ho Kim, Sang Ho Bae, Sung Yong Kim, Moo Jun Baek, Moon Soo Lee
- Surg Metab Nutr 2018;9(1):26-30. Published online June 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.1.26
-
 Abstract
Abstract
 PDF
PDF Purpose:
Gastric outlet obstruction (GOO) is a common problem associated with advanced malignancies of the upper gastrointestinal tract. Adverse events, such as malnutrition, can affect the quality of life, and gastrojejunostomy can be performed for palliative care. This study evaluated effects of total parenteral nutrition (TPN) therapy in post-operation state patients who underwent a palliative gastrojejunostomy (PGJ).
Materials and Methods:
Between January 2011 and June 2015, a total of 65 patients underwent PGJ at Soonchunhyang University Cheonan Hospital and all consecutive patients were included in this retrospective study. All patients were divided into the preoperative TPN group and non-TPN group. A nutritional status assessment included the body weight (BW), body mass index (BMI), CRP level, serum albumin, serum total protein, hemoglobin, and total lymphocyte count (TLC).
Results:
Thirty-one patients did not receive the TPN treatment, and 34 patients received the TPN treatment before surgery. Significant differences between preoperative and postoperative BW, BMI, CRP level, serum albumin, serum total protein, hemoglobin, and TLC were observed in the non-TPN group. On the other hand, there was no significant difference between the preoperative BW, BMI, TLC and postoperative BW, BMI, TLC in the TPN group (p=0.914, p=0.873, p=0.319).
Conclusion:
These results suggest that preoperative TPN therapy can improve the nutritional status in patients who underwent PGJ.
- 710 View
- 1 Download

- Role of Postoperative Parenteral Nutrition in Elective Surgery; Selection of Patients and Conditions for Postoperative Parenteral Nutrition
- Jong Won Kim
- Surg Metab Nutr 2018;9(1):1-4. Published online June 30, 2018
- DOI: https://doi.org/10.18858/smn.2018.9.1.1
-
 Abstract
Abstract
 PDF
PDF Postoperative early enteral nutrition or early oral ingestion is recommended in surgical patients. In this situation, this study examined the role of parenteral nutrition in the postoperative period in patients undergoing elective surgery. The nutritional status should be assessed before surgery and in the case of malnutrition, nutritional support should be provided before surgery to obtain good results. More than 2 weeks of insufficient nutritional support after surgery may worsen the patient’s progress. Therefore, it is recommended to start nutritional care if the oral intake is not appropriate until 7 days or 5 to 7 days after surgery. Enteral nutrition is related to the quick restoration of the bowel function and reduction of infection-related complications. Therefore, enteral nutrition has priority. On the other hand, depending on the patient’s condition, it may not be possible to perform enteral nutrition, and the uniform implementation of the early enteral nutrition may be a burden to the patient. Parenteral nutrition has the advantage that it can supply nutrition without being affected by the intestinal condition, and it can be calculated to supply as much energy as required. The situation, where parenteral nutrition is required after elective surgery, could be summarized as 1) the patients who underwent nutritional therapy before surgery and could not tolerate oral intake or enteral nutrition after surgery. or 2) in the case where enteral nutrition did not satisfy 50% of the demand at 7 days after surgery, and it is judged that this situation should continue for 7 days.
- 640 View
- 1 Download

- Effects of Parenteral Nutrition in Pediatric Patients with Hematopoietic Stem Cell Transplantation
- Soo Young Lim, Min Jae Jung, Ji Eun Park, Jae Song Kim, Soo Hyun Kim, Chuhl Joo Lyu, Eun Sun Son
- J Clin Nutr 2018;10(1):9-19. Published online June 30, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.1.9
-
 Abstract
Abstract
 PDF
PDF Purpose:
This study examined the effects of parenteral nutrition (PN) on the nutritional status, clinical improvement, and PN-related complications in pediatric patients who had undergone hematopoietic stem cell transplantation (HSCT).
Methods:
A retrospective audit of 110 pediatric patients (age≤18), who underwent HSCT from March 2015 to February 2017 was undertaken. The patients were divided into 3 groups based on the ratio of daily calorie supplementation to the daily calorie requirement (ROCS). The clinical factors related to the nutritional status, such as difference in body weight (BW), body mass index (BMI), percent ideal body weight (PIBW), total protein (T.protein), and albumin; the early clinical outcome, such as PN-duration, length of hospitaliaztion (LOH), engraftment day (ED), graft-versus-host disease, sepsis, pneumonia and mucositis; and PN-related complications, including elevation of total bilirubin (T.bil), direct bilirubin (D.bil), aspartate aminotransferase, alanine aminotransferase, glucose and cholesterol levels, and hepatic veno-occlusive disease were analyzed using the electronic medical records. Additional analysis subject to auto-HSCT and allo-HSCT patients was also performed.
Results:
The very-low-ROCS, low-ROCS, and satisfied-ROCS group were 30 (27.3%), 47 (42.7%), and 33 (30.0%) patients, respectively. The PN-duration (P=0.005, z=–2.271), LOH (P=0.023, z=–2.840), ED (P<0.001, z=–3.695), T.bil elevation (P<0.001, z=–3.660), and D.bil elevation (P=0.002, z=–3.064) tended to decrease with increasing ROCS. The difference in the PN-duration (P=0.017), ED (P=0.001), T.bil elevation (P=0.001), and D.bil elevation (P=0.011) in the 3 groups was statistically significant. In the auto-HSCT patients, the change in BW (P=0.031, z=+2.154), PIBW (P=0.029, z=+2.187), and BMI (P=0.021, z=+2.306) tended to increase. In the allo-HSCT patients, the change in T.protein (P=0.022, z=+2.286) increased but the ED (P=0.021, z=–2.304) decreased.
Conclusion:
Aggressive PN supplementation has an effect on maintaining the nutritional status and achieving better early outcomes in pediatric HSCT patients, whereas it has no effect on increasing the PN-related complications.
- 681 View
- 4 Download

- Clinical Outcomes of Nutritional Supply in Critically Ill Patients in the Prone Position
- Yeonju Lee, Hyung-Sook Kim, Hyungwook Namgung, Eun Sook Lee, Euni Lee, Young-Jae Cho, Yeon Joo Lee
- J Clin Nutr 2018;10(1):2-8. Published online June 30, 2018
- DOI: https://doi.org/10.15747/jcn.2018.10.1.2
-
 Abstract
Abstract
 PDF
PDF Purpose:
Enteral nutrition is recommended in critically ill patients. On the other hand, the recommendation of nutritional support is limited and often controversial in critically ill patients in the prone position. Therefore, this study evaluated the clinical outcomes of nutritional support in critically ill patients in the prone position.
Methods:
A retrospective evaluation of the electronic medical records was conducted, including adult patients who were in the medical intensive care unit (ICU) in the prone position in Seoul National University Bundang Hospital from May 1, 2015 to June 30, 2017. The patients’ characteristics, nutritional support status while they were in the prone position, mortality in ICU and during hospitalization, ICU length of stay, mechanical ventilation days, and complications, such as ventilator associated pneumonia (VAP) and vomiting were collected.
Results:
In total, 100 patients were included. Of these, 12 received enteral nutrition and parenteral nutrition and 88 received only parenteral nutrition. The groups were similar in terms of age, sex, number of comorbidity, weight, PaO2/FiO2, hours of prone position, Simplified Acute Physiology Score II (SAPS II), Acute Physiologic and Chronic Health Evaluation II (APACHE II) score, and Sequential Organ Failure Assessment (SOFA) score. No differences were observed in ICU mortality (75.0%
vs . 46.6%; P=0.065), hospital mortality (83.3%vs . 58.0%; P=0.081), ICU length of stay (22.2±14.6vs . 18.2±21.2; P=0.128) and mechanical ventilation days (19.3±14.8vs . 14.5±19.1; P=0.098). In addition, there were no differences in the possible complications of the prone position, such as VAP (8.3%vs . 4.5%; P=0.480) and vomiting (8.3%vs . 1.1%; P=0.227).Conclusion:
No significant differences in the clinical outcomes were observed. Further studies will be needed to confirm the way of nutrition support while in the prone position.
- 723 View
- 6 Download

- Parenteral Nutrition-associated Liver Disease
- Jin Hong Lim
- Surg Metab Nutr 2017;8(1):7-12. Published online June 30, 2017
- DOI: https://doi.org/10.18858/smn.2017.8.1.7
-
 Abstract
Abstract
 PDF
PDF Parenteral nutrition-associated liver disease (PNALD) is frequently observed in patients who require long-term parenteral nutrition. PNALD is diagnosed by clinical presentation, biochemical liver function test, long-term usage of parenteral nutrition, and negative workup for other liver diseases. Pathogenesis of PNALD is multifactorial and includes prematurity, nutritional excess, sepsis, and lack of enteral nutrition. Since PNALD was first reported more than 30 years ago, there have been various attempts to find effective treatments for PNALD. Cyclic parenteral nutrition and use of ω-3 polyunsaturated long-chain fatty acids (ω-3 PUFA) instead of ω-6 PUFA were reported worldwide as effective treatments. This article reviews the literature relating to PNALD.
-
Citations
Citations to this article as recorded by- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
Yunhyung Kim, Yeon Hee Kim, Jae Sim Jeong
Journal of Korean Association for Qualitative Research.2024; 9(1): 1. CrossRef - Treatment Status of Parenteral Nutrition-Associated Cholestasis in Pediatric Patients at a Single Tertiary Hospital
Soh Yeon Park, Yu Jeong Son, Min Jung Geum, Jong Hee Ko, Eun Sun Son, Yun Mi Yu, Eun Joo Lee
Journal of Korean Society of Health-System Pharmacists.2024; 41(4): 373. CrossRef
- The Post-Discharge Caregiving Experiences of Mothers of Children with Intestinal Failure
- 1,927 View
- 23 Download
- 2 Crossref

- Evaluation on the Time to Start Parenteral Nutrition in Hospitalized Cancer Patients
- Nam Hyo Kim, Hyo Jung Park, Yong Won In, Young Mee Lee
- J Clin Nutr 2017;9(1):30-35. Published online June 30, 2017
- DOI: https://doi.org/10.15747/jcn.2017.9.1.30
-
 Abstract
Abstract
 PDF
PDF Purpose:
Malnutrition is quite prevalent in hospitalized cancer patients, with a 40%∼80% rate. Malnutrition in cancer patients can result in an increase in the number of complications, length of stay, mortality, and morbidity. Therefore, cancer patients with malnutrition must have the appropriate nutritional support to improve the prognosis of cancer. This study evaluated the appropriate time point to start parenteral nutrition (PN) after admission according to the nutrition support guidance in Samsung Medical Center.
Methods:
This study enrolled patients diagnosed with the Korean standard classification of disease 6 (KCD6) code C00-C97 and discharged from March 1st to 31st, 2016. The following data were collected: patients’ age, gender, diagnosis, length of stay, body mass index, nutritional status, and whether to consult nutrition support team (NST).
Results:
Among a total of 2,944 patients, 381 patients (12.9%) were in a malnourished status upon admission. In the malnourished patients, 139 patients were prescribed PN for a median of 6 days (range, 1∼49) and moderate to severe malnourished patients were started on PN within 2 days after admission. The proportion of patients with a poor nutritional status was lower in the NST group than in the non-NST group (50.0% vs. 66.7%) on the 28th day after admission. Among the nourished patients, 229 patients were prescribed PN. Of them, 183 patients (79.9%) were started on PN within 7 days after admission.
Conclusion:
In moderate to severe malnourished cancer patients, the initiation of PN on the day after admission is appropriate.
-
Citations
Citations to this article as recorded by- Best evidence summary for the rational use of parenteral nutrition in hospitalized cancer patients
Zhengzheng Liu, Beijia Liu, Niannian Weng, Qian Gui, Di Liu, Yuchi Wu, Guiyu Huang, Mingxue Yang, Xiaoli Tang
Frontiers in Nutrition.2026;[Epub] CrossRef
- Best evidence summary for the rational use of parenteral nutrition in hospitalized cancer patients
- 785 View
- 2 Download
- 1 Crossref

- Influence of Fish Oil-Containing Lipid Emulsions on Parenteral Nutrition-Associated Liver Disease in Neonates
- Jeong-A Park, Ji-Eun Park, Min-Jae Jeong, Jae-Song Kim, Eun-Sun Son, Ho-Seon Eun
- J Clin Nutr 2017;9(1):21-29. Published online June 30, 2017
- DOI: https://doi.org/10.15747/jcn.2017.9.1.21
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material Purpose:
This study is a comparative evaluation of the incidence of parenteral nutrition-associated liver disease (PNALD) when administering intravenous fat emulsions containing fish oil.
Methods:
The medical records of patients who were in the neonatal intensive care unit at Severance Hospital from January, 2012 to December 2015, were reviewed retrospectively. Patients who were administered either soybean oil (SO) or SMOF (containing soybean oil, medium chain triglycerides, olive oil, and fish oil) more than 14 days were included. The patients were excluded if they were administered both agents or had underlying hepatic disease. An increase in bilirubin to 2 mg/dL was defined as PNALD.
Results:
PNALD occurred in only 8 out of a total of 77 patients: 6 out of 31 (19.4%) in the SO group and 2 out of 46 (4.3%) in the SMOF group (P=0.055). The number of patients, whose lab values, such as direct bilirubin, total bilirubin, asparate aminotransferase (AST), alanine amino-transferase, gamma-glutamyl transpeptidase, C-reactive protein, serum triglyceride, and alkaline phosphate, exceeded the normal range, were similar in both groups. The gestational age, birth body weight, and APGAR score at 1 min and 5 min were significantly higher in the SO group and the PN duration was significantly long in the SMOF group. Considering only term infants, there were no significant differences in baseline characteristics and incidence of PNALD. The number of patients whose AST exceeded the normal range was significantly higher in the SO group (P=0.034).
Conclusion:
The incidence of PNALD was similar in both groups. On the other hand, considering the tendency, there was a high correlation between the type of lipid emulsion and an increased direct bilirubin level in the SO group.
- 869 View
- 1 Download

- Analysis of Adverse Reactions Associated with Parenteral Nutrition Use in Korea
- Sera Lee, Miyoung Ock, Seonghee Kim, Hyunah Kim
- J Clin Nutr 2017;9(1):16-20. Published online June 30, 2017
- DOI: https://doi.org/10.15747/jcn.2017.9.1.16
-
 Abstract
Abstract
 PDF
PDF Purpose:
To evaluate the clinical manifestations of adverse drug reactions (ADRs) of parenteral nutrition (PN) use in Korea.
Methods:
The Korean Adverse Event Reporting System (KAERS) database records in 2015 on PN-treated patients were used. ADRs classified as “certain,” “probable,” and “possible” based on the WHO-Uppsala Monitoring Centre criteria were analyzed.
Results:
In total, 21,436 ADRs from 2,346 patients were included for analysis. The mean patient age was 57.1 years and the mean number of ADRs per patient was 9.1. ADRs were reported frequently with amino acids solutions (682 events, 40.8%), followed by combinations products (519 events, 31.1%), and fat emulsions (363 events, 21.7%). The frequent ADRs were gastrointestinal (507 events, 30.3%), skin (343 events, 20.5%), general disorders (239 events, 14.3%), and central/peripheral nervous system disorders (165 events, 9.9%). The common clinical symptoms were nausea (321 events, 19.2%), vomiting (105 events, 6.3%), and vein pain (102 events, 6.1%). Serious ADRs accounted for 220 patients (9.4%) and dyspnea was the most frequent clinical manifestation.
Conclusion:
This study analyzed the KAERS data in 2015 from patients treated with PN and revealed gastrointestinal and skin disorders to be the leading ADRs.
-
Citations
Citations to this article as recorded by- Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach
Hyewon Sim, Jin Soo Moon, Young Suk Park, Eunji Heo, Yoon Soo Chun, Songhwa Choi, Hyemin Ku, Jae Hee Chung
Nutrients.2025; 17(22): 3551. CrossRef
- Health State Utility Associated with Parenteral Nutrition Requirement in Patients with Short Bowel Syndrome and Intestinal Failure in Korea: A Vignette-Based Approach
- 901 View
- 5 Download
- 1 Crossref

- Postoperative Nutritional Support for Gastrectomized Patients
- Han Hong Lee
- Surg Metab Nutr 2016;7(2):25-28. Published online December 30, 2016
- DOI: https://doi.org/10.18858/smn.2016.7.2.25
-
 Abstract
Abstract
 PDF
PDF Nutritional deficiency after gastrectomy is caused by anatomical and physiologic changes in the stomach. In the case of patients with gastric cancer, nausea and loss of appetite due to cancer cachexia syndrome can affect nutritional status after gastrectomy. Prognostic nutritional index based on preoperative nutritional conditions is used for prediction of postoperative outcomes including long-term survival. Generally, enteral nutrition is more effective for post-gastrectomy conditions than parenteral nutrition. In addition, specialized enteral formulas such as immunonutrition (amino acids, ω-3 fatty acids and nucleotide) seem to have benefits for gastrectomy patients, although there is still insufficient evidence. Ghrelin is a next generation agent to stimulate appetite in patients that underwent gastrectomy.
- 690 View
- 1 Download

- Lipids: Functional Effects and Clinical Application in Parenteral Nutrition
- Soo Jin Yang
- Surg Metab Nutr 2016;7(1):1-6. Published online June 30, 2016
- DOI: https://doi.org/10.18858/smn.2016.7.1.1
-
 Abstract
Abstract
 PDF
PDF Lipids are structural components of cellular membrane and functional components exerting an important role in different metabolic pathways through regulation of cell signaling and metabolic homeostasis. Although the human body can synthesize some fatty acids, essential fatty acids (EFA) should be exogenously provided. Parenteral nutrition (PN) can be utilized to provide EFA for patients without normal gastrointestinal functions and those at risk of malnutrition. Parenteral lipids provide more energy-dense nutrition in a reduced volume and prevent EFA deficiency. However, prolonged PN with lipid emulsions is associated with metabolic complications including PN-associated liver disease. Currently available parenteral lipid emulsions provide various combinations of soybean oil, fish oil, olive oil and medium-chain triglycerides. The effects of parenteral lipid emulsions on the lipid nutrition status and PN-associated complications vary depending on the type and dosages of main oil sources used in parenteral lipid solutions. Therefore, understanding the composition, metabolism, and functional effects of lipids can be helpful in considering their clinical applications in PN.
- 874 View
- 2 Download

- Effect of Fish Oil-based Intravenous Fat Emulsion with Parenteral Nutrition in Patients Undergoing Allogeneic Hematopoietic Stem Cell Transplantation
- Ji Hyeong Choe, Young Joo Lee, Hye Jung Bae, Sun Hoi Jung, Hyeon Joo Hahn, Yungil Koh
- J Clin Nutr 2016;8(1):29-35. Published online April 30, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.1.29
-
 Abstract
Abstract
 PDF
PDF Purpose:
Omega-3 fatty acid is known for immunonutrition in that it has anti-inflammatory properties and improves the patients’ immune function. The objective of this study was to determine the effects of a fish oil-based lipid emulsion for adult patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT).
Methods:
This was a retrospective study of 90 adult allogeneic HSCT patients from July 2011 to June 2015. The patients were divided into two groups according to the lipid type provided; fish oil group (FO group, n=55) and non-fish oil group (NFO group, n=35). The demographics, parenteral nutrition and lipid emulsion duration, length of hospital stay (LOS), weight change, 30 day mortality, survival period, incidence of acute graft-versus-host disease (aGVHD), neutropenic fever, sepsis, and re-hospitalization were collected from the electronic medical records.
Results:
The patients’ characteristics including age, sex, body mass index, and underlying disease were similar in the two groups. The incidence of aGVHD and infectious complications, mortality, LOS, re-hospitalization were also similar. The FO group showed weight gains, whereas the NFO group showed weight loss (FO
vs. NFO=0.34%vs. ?1.08%, P=0.245).Conclusion:
The clinical outcomes were similar in the two groups but there was a tendency for gain weight in the FO group. A large, well designed study, and a dosing study will also be needed to determine the optimal dose range for HSCT patients.
- 720 View
- 2 Download

- Economic Evaluation of Home Total Parenteral Nutrition
- Ja Kyung Min
- J Clin Nutr 2016;8(1):19-23. Published online April 30, 2016
- DOI: https://doi.org/10.15747/jcn.2016.8.1.19
-
 Abstract
Abstract
 PDF
PDF The restricted resources on healthcare highlights the importance of clinical and cost effectiveness. The social and economic costs of chronic diseases are increasing. Home total parenteral nutrition (home TPN) for the patients with intestinal failure is a life-sustaining therapy until intestinal transplantation. An economic evaluation of home TPN has not been conducted in Korea. Three types of economic evaluations for home TPN are cost benefit analysis, cost effectiveness analysis, and cost utility analysis. Korea’s medical market is competitive due to the limited health care resources. A health care delivery system from hospital to home needs to be established under the supervision of professional Nutrition Support Team staff including the systematic policies and social recognition.
- 943 View
- 3 Download

- Evaluation of Postoperative Nutrition Support with Commercial Peripheral Parenteral Nutrition after an Ivor-Lewis Esophagectomy in Patients with Esophageal Cancer
- Sun-woo Lee, Na-ri Lim, Hyo Jung Park, Yong-won In, Jeong-meen Seo, Young-mee Lee
- J Clin Nutr 2015;7(3):87-92. Published online December 31, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.3.87
-
 Abstract
Abstract
 PDF
PDF Purpose:
Deteriorated nutritional status is common during a hospital stay for esophagectomy in patients with esophageal cancer. Malnutrition in those patients is often marked compared with other gastrointestinal cancer. The purpose of this study is to evaluate the appropriateness of commercial peripheral parenteral nutrition (CPPN) use in patients who underwent Ivor-Lewis esophagectomy (I-L op).
Methods:
Patients who were provided with CPPN after I-L op were enrolled in this study from January to May 2015. Body weight, height, nutritional status, length of hospital stay, duration of CPPN therapy, and parenteral nutrition (PN) induced complications were assessed, respectively, using electronic medical records.
Results:
Thirty-nine patients were enrolled. Average age was 65.9 years and 36 patients were male. All patients were provided with the same CPPN. The duration of fasting and CPPN use was 5.8±1.4 days and 7.5±1.8 days, respectively. Calorie supported by CPPN was 22.6±3.5 kcal/kg/day and only 20.5% of patients (n=8) reached the daily target calories. Most frequent PN induced complication was phlebitis which occurred in 8 patients (20.5%). Calcium, magnesium, and transthyretin levels in serum were not monitored during the PN support period.
Conclusion:
The indications for CPPN were appropriate because the fasting duration in patients with I-L op was 5 to 10 days. Although a large portion of patients could not be supplied daily target calories, their nutrition status was not significantly changed on admission and at discharge. We did not find it necessary to individualize PN support for a short period after an I-L op in patients with esophageal cancer. Further study will be needed to determine why the incidence of phlebitis was dominant.
- 768 View
- 1 Download

- Analysis of Current Use of Early Parenteral Nutrition and Clinical Significance of Non-protein Calorie: Nitrogen in Surgical Critically Ill Patients
- Eunjeong Heo, Kayoung Park, Sujeong Jeon, Hyungwook Namgung, Eunsook Lee, Inae Song
- J Clin Nutr 2015;7(3):75-80. Published online December 31, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.3.75
-
 Abstract
Abstract
 PDF
PDF Purpose:
Surgical critically ill patients require adequate nutrition support and the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) guidelines recommend low non-protein calorie:nitrogen ratio (NPC:N ratio, 70∼100) for critically ill pateints. In this study, we assess the current use of early parenteral nutrition of surgical critically ill patients and analyze the clinical significance of NPC:N.
Methods:
This is a retrospective study of critically ill adult patients who remained in the intensive care unit (ICU) for over 3 days and could not receive enteral nutrition for the first 7 days. Data on parenteral intake of patients were collected from electronic medical records. Association of NPC:N scores with clinical outcome (length of ICU stay, length; of hospital stay, duration of ventilation, and mortality) were analyzed using Pearson correlation and multiple regression.
Results:
The study included 72 cases, average parenteral calorie intake was 14.6 kcal/kg/day and protein intake was 0.5 g/kg/day. We assessed the NPC:N scores to determine the patients’ NPC:N for the first 7 days in ICU close to the A.S.P.E.N guidelines. NPC:N scores showed weak negative correlation with length of hospital stay and duration of mechanical ventilation (r=−0.259, P=0.028; r=−0.495, P=0.001). Multiple regression adjusted with APACHE (Acute Physiology and Chronic Health Evaluation) II score, age, and body mass index showed correlation of higher NPC:N score with decreased length of hospital stay and shorter duration of ventilation (P=0.0001, P=0.035, respectively). However, length of ICU stay and mortality within 60 days showed no significant correlation with NPC:N scores.
Conclusion:
Parenteral calories and protein intakes of critically ill patients in ICU were lower in comparison to A.S.P.E.N. recommendation in this study. Low NPC:N scores might be related to shorter length of hospital stay, duration of mechanical ventilation. Consultation of a nutritional support team could have a positive effect in providing appropriate nutrition support.
- 1,646 View
- 12 Download

- Role of Parenteral Glutamine in Nutrition Support for Critically Ill Patients
- Hyo Jung Park
- J Clin Nutr 2015;7(2):42-48. Published online August 31, 2015
- DOI: https://doi.org/10.15747/jcn.2015.7.2.42
-
 Abstract
Abstract
 PDF
PDF Glutamine is the most abundant amino acid, composed of more than 50 percent of free amino acid in the human body. It had been regarded as a conditional essential amino acid and its concentration is markedly reduced in critically ill patients with trauma, burn, or sepsis. From the early 1990s, many parenteral glutamine studies on critical illness have reported the benefits in mortality, infection, and length of stay. However, its clinical efficacy was based on out-of-date, smaller, single-center studies. Clinical effects of parenteral glutamine have shown no benefits or even harms in recent clinical trials and meta-analysis. Furthermore, it has challenged the hypothesis that low plasma glutamine concentration was associated with poor outcomes in critically ill patients. Although many studies showing the efficacy of glutamine have been reported, parenteral glutamine supplementation may be harmful in patients with multiorgan failure or baseline kidney dysfunction. Further studies should be conducted to identify the use of glutamine supplementation in combination with parenteral and enteral nutrition or enteral/oral nutrition alone, specific adult or pediatric patients, the appropriate time and doses for administration of glutamine, cost-benefit analysis, and the exact mechanisms of action.
-
Citations
Citations to this article as recorded by- Efficacy of parenteral glutamine supplementation in adult hematopoietic stem cell transplantation patients
Yun Kyung Cho, So Yeon Hong, Su Jeoung Jeon, Hyung Wook Namgung, Eunsook Lee, Euni Lee, Soo-Mee Bang
BLOOD RESEARCH.2019; 54(1): 23. CrossRef
- Efficacy of parenteral glutamine supplementation in adult hematopoietic stem cell transplantation patients
- 2,446 View
- 4 Download
- 1 Crossref

- Trace-Element: Clinical Consideration in Patients with Parental Nutritional Support
- Junbeom Park
- Surg Metab Nutr 2015;6(1):1-6. Published online June 30, 2015
- DOI: https://doi.org/10.18858/smn.2015.6.1.1
-
 Abstract
Abstract
 PDF
PDF Trace-elements play an important role in human metabolism. Often overlooked by clinicians, they are mandatory to supply for the patient with parenteral nutrition. When it is deficient or excessive, inadequate provision of trace elements can lead to serious complication. The nutrition provider should monitor deficiency and toxicity of each trace element carefully. In Korea, five trace elements (Zinc, Copper, Manganese, Chromium, and Selenium) are commercially available. However, according to the up to date recommendation, their dosages are not adequate for patients with long term parenteral nutrition. In this review, I considered the adequate dosage of each trace element under specific conditions, and provided a guideline for monitoring of trace elements.
- 1,362 View
- 5 Download


 E-submission
E-submission KSPEN
KSPEN KSSMN
KSSMN ASSMN
ASSMN JSSMN
JSSMN
 First
First Prev
Prev


